To analyse the prevalence of post-traumatic stress disorder (PTSD) in nursing staff and the variables that may contribute to its development.
MethodCross-sectional study using a self-administered questionnaire given to nurses, nursing assistants and nursing supervisors in June 2020. It included sociodemographic, mental health, occupational, COVID-19 related variables, Modified Risk Perception Scale (modified RPS) score, Brief Resilience Scale (BRS) and Davidson Trauma Scale (DTS) score for the assessment of PTSD. Descriptive, bivariate, and multivariate analyses were performed.
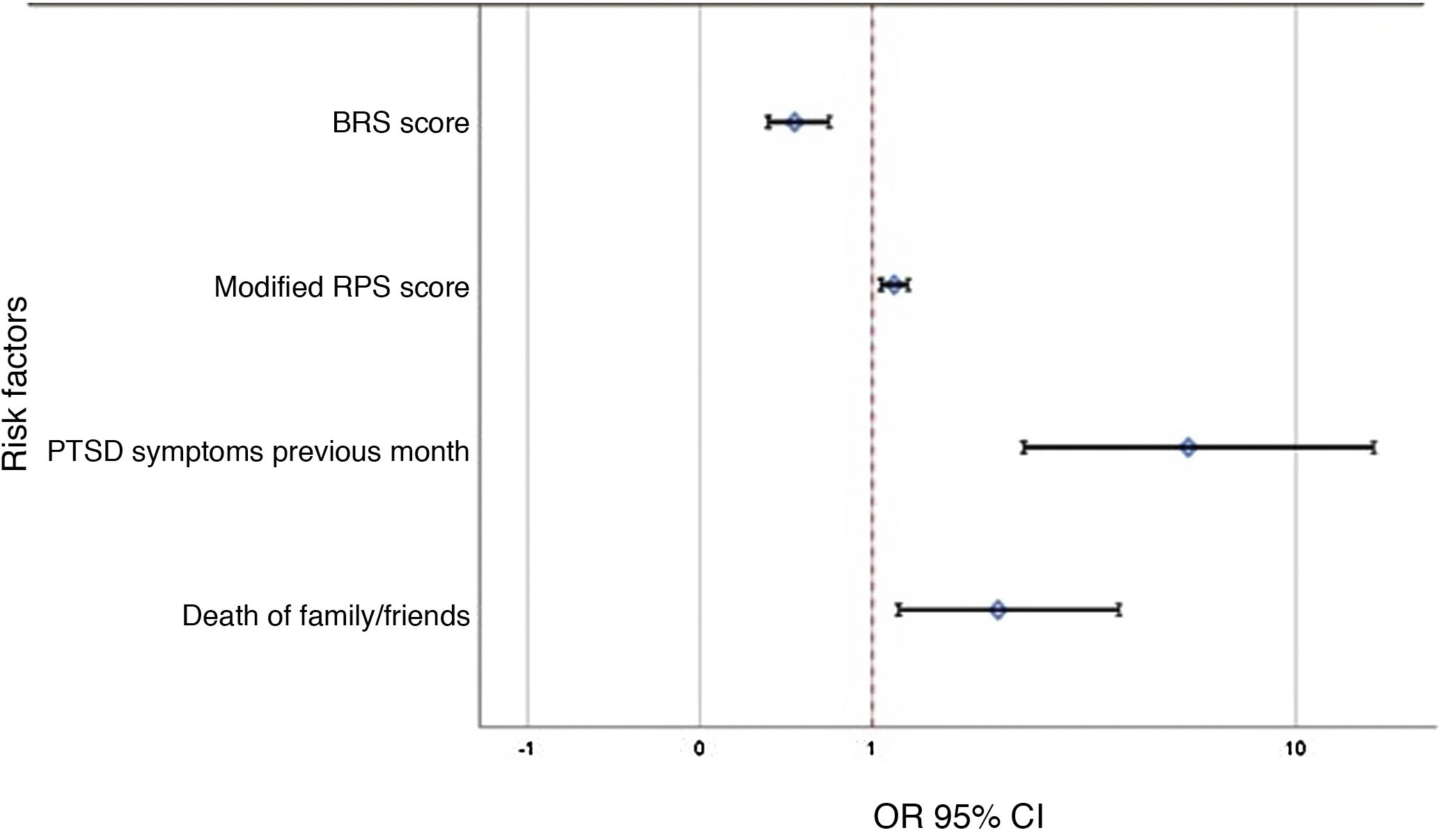
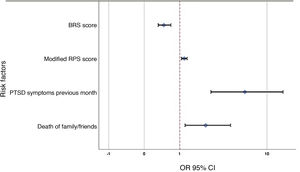
ResultsOf the 344 participants, 88.7% were women and 93.6% cared for infected patients; 45.9% had PTSD (DTS≥40). The variables associated with PTSD were previous PTSD symptoms (OR=6.1, 95% CI [2.68-14.03]), death of a family member or friend due to COVID-19 (OR=2.3, 95% CI [1.22-4.39]), and higher scores on the modified RPS (OR= 1.1, 95% CI [1.07-1.31]). Higher BRS scores were associated with a lower risk of PTSD (OR=0.4, 95% CI [0.31-0.68]).
ConclusionsThe prevalence of PTSD in nursing staff is high, mainly in professionals with previous PTSD symptoms, family members or friends deceased from COVID-19, high risk perception and/or low resilience.
Analizar la prevalencia del trastorno de estrés postraumático (TEPT) en el personal de enfermería y las variables que pudieran contribuir en su desarrollo.
MétodoEstudio transversal mediante un cuestionario autoadministrado a enfermeras, técnicos en cuidados de enfermería y supervisoras de enfermería en junio del 2020. Incluía variables sociodemográficas, de salud mental, laborales, relacionadas con la COVID-19, puntuación de Escala de Percepción de Riesgo modificada (PRS modificada), Escala Breve de Resiliencia (BRS) y Escala de Trauma de Davidson (DTS) para la evaluación del TEPT. Se realizó análisis descriptivo, bivariado y multivariante.
ResultadosDe los 344 participantes, el 88,7% eran mujeres y el 93,6% atendieron a pacientes infectados. El 45,9% presentaba TEPT (DTS ≥40). Las variables asociadas con padecer TEPT fueron haber presentado síntomas del trastorno previamente (OR= 6,1, IC 95% [2,68-14,03]), el fallecimiento de algún familiar o amigo por la COVID-19 (OR= 2,3, IC 95% [1,22-4,39]) y presentar las puntuaciones más elevadas en la PRS modificada (OR= 1,1, IC 95% [1,07-1,31]). Las puntuaciones más altas en la BRS se asociaron con menor riesgo de padecer TEPT (OR = 0,4, IC 95% [0,31-0,68]).
ConclusionesLa prevalencia del TEPT en el personal de enfermería es elevada, principalmente en profesionales con síntomas de TEPT previos, familiares o amigos fallecidos por la COVID-19, una alta percepción de riesgo y/o una baja resiliencia.
What is known?
- •
The international health crisis caused by COVID-19 pandemic has reinforced the role of nurses as agents providing care, attention, and innovation to save lives and reduce suffering.
- •
This work on the front line of defence impacts the mental health of healthcare professionals, which is compromised and impaired.
- •
Post-traumatic stress disorder (PTSD) is the most common disorder following a major traumatic experience. If not adequately diagnosed it constitutes a public health issue and increases associated comorbidity, and impacts the work environment.
What does this paper contribute?
- •
This study shows the prevalence of PTSD, as well as the factors that most influence its development, onset of previous PTSD symptoms, the death of family members or friends due to COVID, a high perception of risk and low resilience being the most significant.
- •
It is essential to work on risk perception and resilience to prepare health professionals psychologically for future health crises.
The first case in Spain of the new SARS-CoV-2 coronavirus (COVID-19) was diagnosed on 31 January, and the number of infections has increased exponentially and continuously. In June 2020, Spain was one of the most affected countries in Europe with more than 240,000 cases.1
This scenario caused the healthcare system to be overwhelmed, and contingency plans had to be implemented. In particular, the psychological wellbeing of nurses and nursing care technicians (NCT), as they are on the front line, has been affected even though they are used to dealing with critical situations.2 Caregiving during stressful events such as epidemics poses a significant risk for the development of post-traumatic stress disorder (PTSD).3,4
DSM-5 defines PTSD as the characteristic clinical picture of victims who have been exposed to traumatic events and whose symptoms are of intrusion, avoidance, negative cognitive and emotional alterations, and disturbances in arousal and reactivity. The duration of symptoms must be longer than one month.5 PTSD poses a risk to personal and occupational health, and interpersonal relationships. Moreover, up to 75% of people diagnosed with PTSD will have another associated psychiatric disorder, including anxiety and depression.6
Studies undertaken in epidemics like the current situation have described high prevalence rates of PTSD in healthcare workers. In Taiwan, 33% of nurses in severe acute respiratory syndrome (SARS) units had PTSD, compared to 19% in non-SARS units.3 In Korea, during the Middle East Respiratory Syndrome (MERS) outbreak, PTSD was reported in 51.5% of healthcare workers.4 In the current COVID-19 outbreak, the prevalence of PTSD in healthcare workers varies from 9.1%7 reported in China to 52.8% in Italy.8 In Spain, Luceño-Moreno et al.2 found that 56.6% of healthcare workers had PTSD.
The main risk factors associated with PTSD in healthcare workers were female sex, being a nurse, having a lower level of education, and concern about infecting people living with them.2,9–11 On the other hand, resilience was a protective factor. Healthcare workers with greater resilience had a lower prevalence of anxiety, depression, and burnout.2,9
Despite the recommendations made during the pandemic aimed at protecting mental health, due to its magnitude, it is likely that there are psychological consequences for nurses. The main objective of the study was to analyse the prevalence of PTSD in nursing staff one month after contingency measures ended in a tertiary level hospital, and the secondary objective was to analyse the variables that could contribute to the development of PTSD in nursing staff.
MethodologyWe designed a descriptive cross-sectional study in which 377 nursing professionals (nurses, NCT and nursing supervisors) from the Hospital 12 de Octubre in Madrid were included from 15 June to 15 July 2020 by convenience sampling. This referral hospital for the southern area of Madrid has 1,368 beds and is defined as a highly complex hospital (level III).
Adult and paediatric departments of the entire hospital were included in the study: inpatient units, surgical services, intensive care units, emergency, dialysis, and endoscopy.
The inclusion criteria were to have consented to participate in the study and having worked in the hospital between 1 March and 15 May 2020 (ending of contingency measures). Exclusion criteria were not having fully completed the Davidson Trauma Scale (DTS) or having been on sick leave for 60 days or more, as this was considered insufficient exposure to the stressors specific to nursing work during the pandemic.
The sample size was calculated based on the percentage of PTSD in nurses (28.4%) as described by Su et al. during the SARS outbreak in Taiwan.3 Based on the population of 3,149 nurses in the hospital, a minimum sample size of 335 subjects was estimated with a 95% CI and a margin of error of 5%, assuming a loss rate of 15%.
For the data collection, an ad hoc anonymous paper form was drafted and piloted by 10 professionals representative of the sample, which collected the following data:
- •
Socio-demographic data: age, sex, living alone, marital status, dependents, educational level, professional category.
- •
Mental health data: history of mood disorder, psychopharmacological and/or psychotherapeutic treatment during or after the COVID-19 crisis, presence of PTSD symptoms in the last month (anxiety, insomnia, anger, nightmares, negative thoughts, flashback).
- •
Work data: work unit during the crisis, unit other than the usual, care of COVID patients, professional experience.
- •
Data relating to COVID-19: sick leave during the pandemic, number of days of sick leave, becoming infected themselves by COVID-19, infection of cohabitants by COVID-19, infection of close relatives or friends by COVID-19, death of close relatives or friends due to COVID-19.
- •
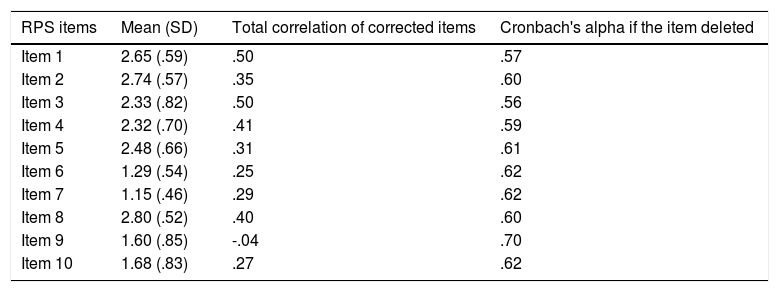
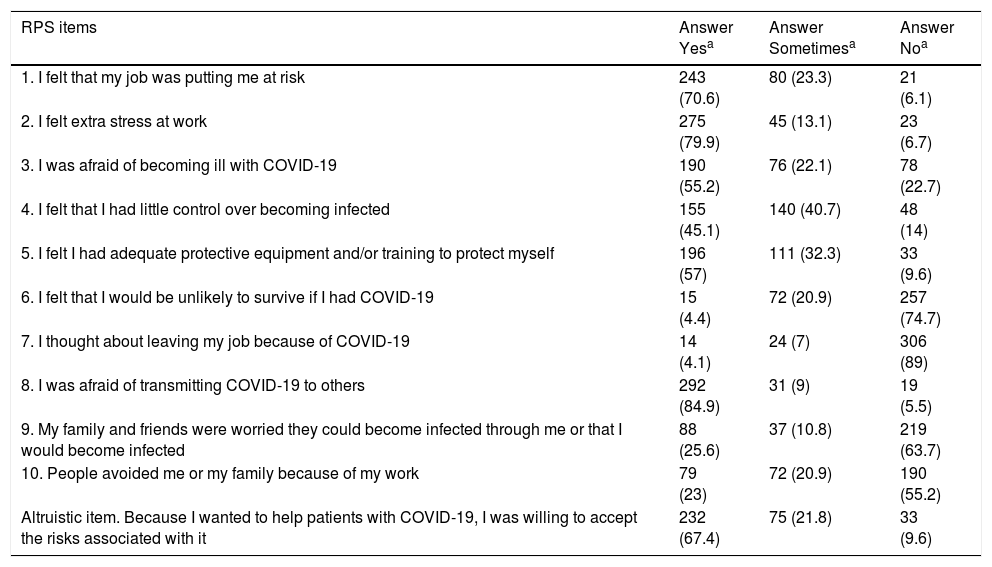
Data relating to the Risk Perception Scale (RPS): this scale was created from 9 items that were used to quantify the risk perception of healthcare workers during the SARS epidemic of 2003.12 In the present study, we also added the item: "I felt that I did not have the protective equipment and/or adequate training to protect myself". In the internal consistency study, Cronbach's alpha coefficient was .64 for the scale. Based on this same analysis, an increase in Cronbach's alpha was shown on omitting item 9, reaching a coefficient of .7 and thus acceptable reliability for the scale. Thereafter, the modified RPS scores (Table 1) were used in the analysis. These were scored on a Likert scale (no = 1, sometimes = 2, yes = 3), obtaining a range from 9 to 27 points. The item "Because I wanted to help patients with COVID-19, I was willing to accept the risks involved" was added to this 9-item scale. This item was scored separately as a measure of altruistic risk acceptance and was not part of the scale score.
Table 1.Homogeneity index of the Risk Perception Scale.
RPS items Mean (SD) Total correlation of corrected items Cronbach's alpha if the item deleted Item 1 2.65 (.59) .50 .57 Item 2 2.74 (.57) .35 .60 Item 3 2.33 (.82) .50 .56 Item 4 2.32 (.70) .41 .59 Item 5 2.48 (.66) .31 .61 Item 6 1.29 (.54) .25 .62 Item 7 1.15 (.46) .29 .62 Item 8 2.80 (.52) .40 .60 Item 9 1.60 (.85) -.04 .70 Item 10 1.68 (.83) .27 .62 SD: standard deviation; RPS: Risk Perception Scale.
- •
Data relating to the Brief Resilience Scale (BRS): created by Smith et al. en 2008,13 adapted and validated in Spanish in 2016.14 The scale assesses the ability to recover from adversity, with a Cronbach's alpha of .83 in its Spanish version. It is a self-administered scale with 6 items formulated positively (items 1, 3, 5) and negatively (items 2, 4, 6). Likert-type responses range from 1 (strongly disagree) to 5 (strongly agree). The sum of the items ranges from 6 to 30 points. For interpretation, the scores of negative items should be reversed (1 would be 5, 2 would be 4, etc.). The scores are then added and divided by 6 to find the mean. The higher the score, the higher the resilience.12,14
- •
Data relating to the DTS: devised in 1997 by Davidson et al. to assess PTSD symptoms,15 and translated and adapted to Spanish, showing adequate reliability and validity.16 This is a self-administered scale consisting of 17 items that quantify the frequency and severity of a series of symptoms grouped into categories according to the criteria established in DSM-4 for PTSD. The time reference is the previous week. Each item is rated from 0 to 4 on a frequency scale and on a severity scale (0 = never or no severity, 4 = daily or extreme severity) generating two scores. The sum of the two is the total score, which ranges from 0 to 136. A score of 40 is the cut-off used to diagnose PTSD.16
The study began following approval by the Research Commission of the Hospital Universitario 12 de Octubre (TP20/0144).
The research team contacted each of the nursing supervisors of the units involved in the study and explained in detail both the objective of the study and the methodology for data collection.
One month after contingency measures ended, each supervisor was given alphanumerically coded forms to guarantee the confidentiality of the participants. They distributed these forms to staff in their units who had given their consent to participate in the study. They then kept them until the research team collected them to be transcribed into a database created in Microsoft Excel 2016 to which only the team had access.
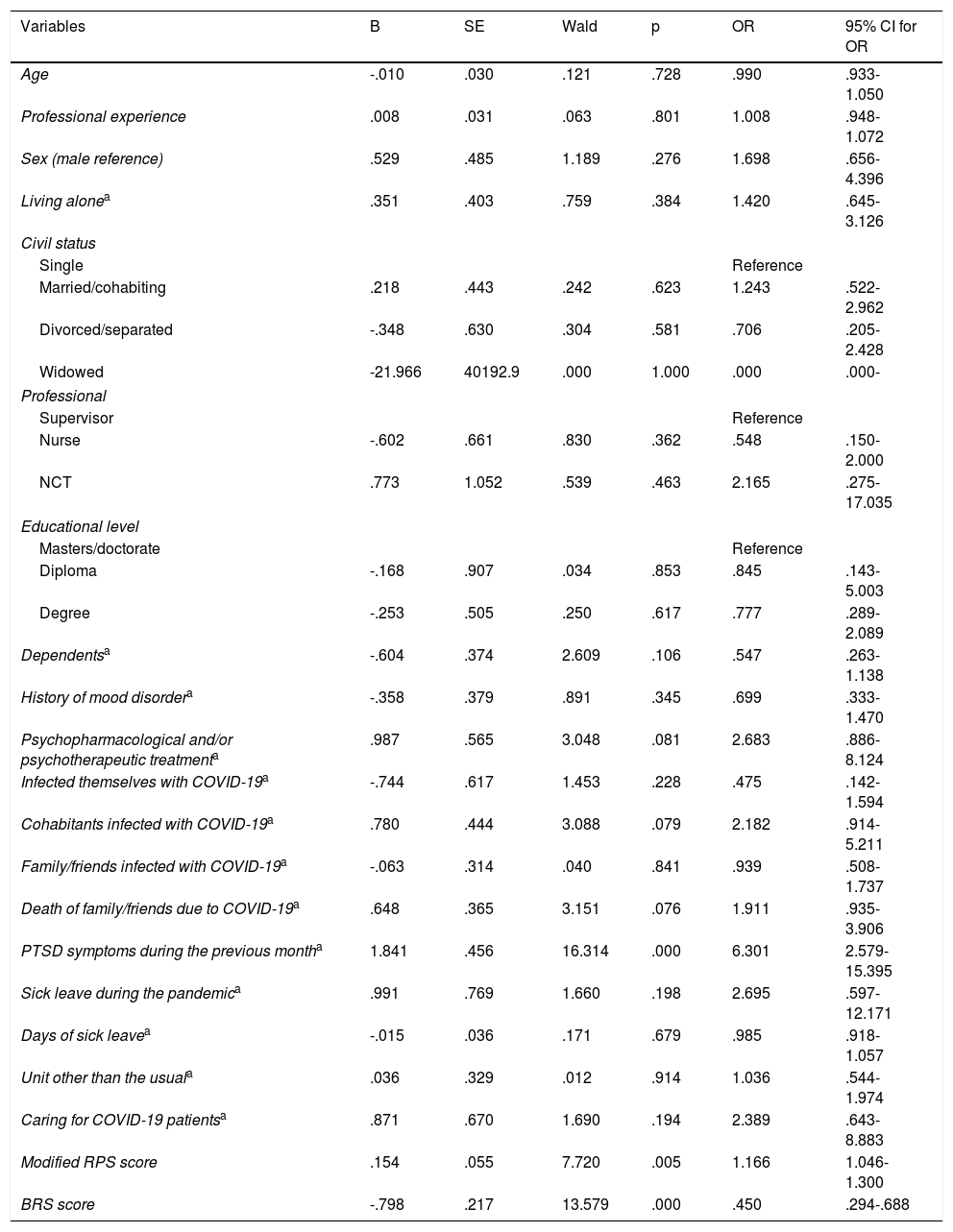
The results were processed statistically using the IBM® SPSS v25 software package. Qualitative variables were described by frequencies and percentages and quantitative variables by median and interquartile range, because after performing the normality test using the Kolmogorov-Smirnov test we observed that the sample did not follow a normal distribution. Differences were compared with non-parametric statistical tests: χ2, Mann-Whitney U test and Spearman correlation. To analyse the impact of the different variables on onset of PTSD, initially we performed a bivariate binary logistic regression, followed by a multivariate regression using the backward stepwise method (Wald). For this purpose, the variables that obtained a p-value of less than .25 were included, in addition to the variables sex and age. The statistical and inferential analysis was performed establishing a 95% CI and a statistical significance level of p < .05.
ResultsWe received 377 of the 470 questionnaires submitted, with a response rate of 80.2%. Thirty-three were rejected as they met the exclusion criteria (29 due to incomplete completion of the DTS scale and 4 due to sick leave of 60 days or more). Eventually, 344 questionnaires were included in the analysis.
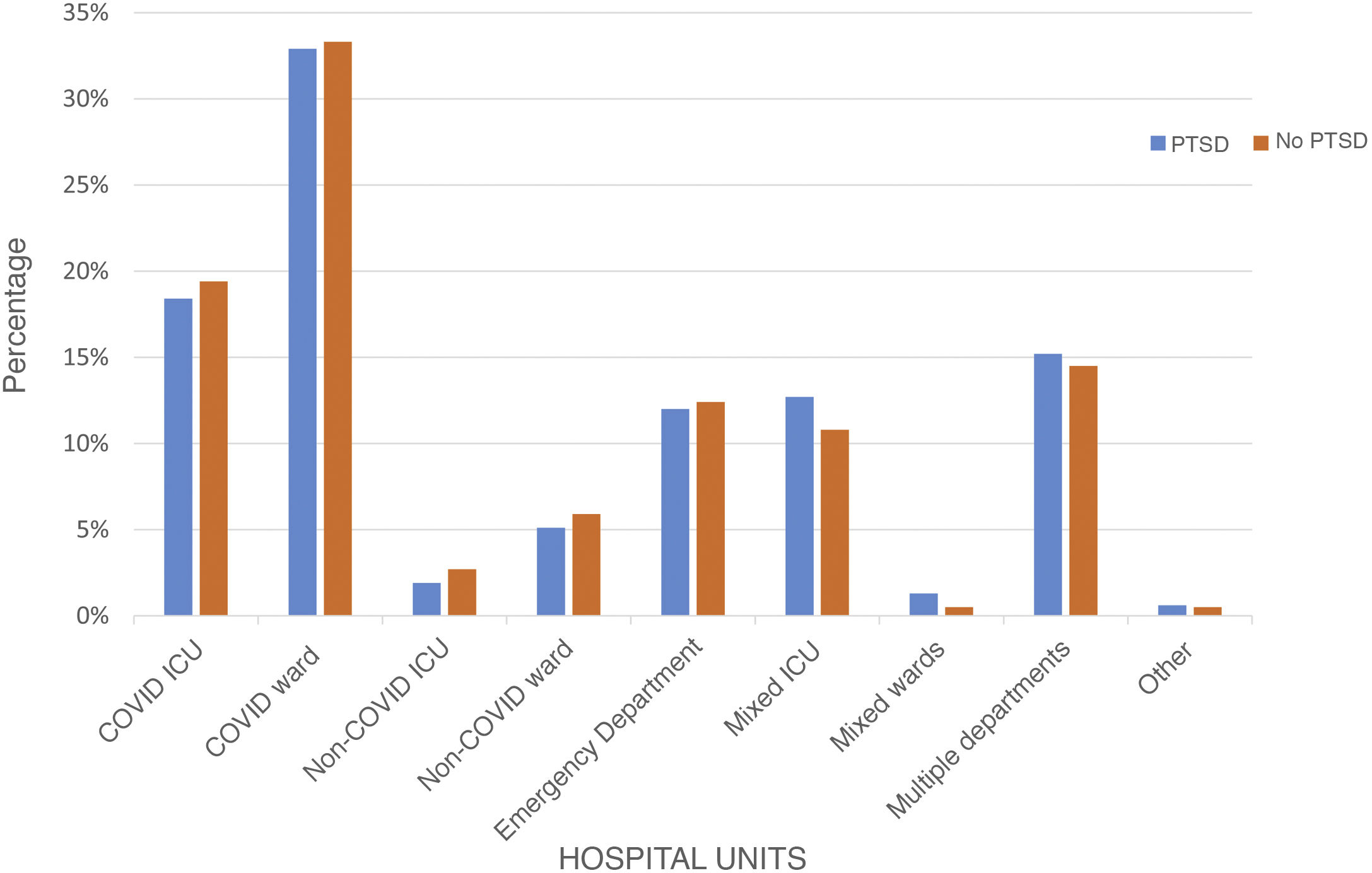
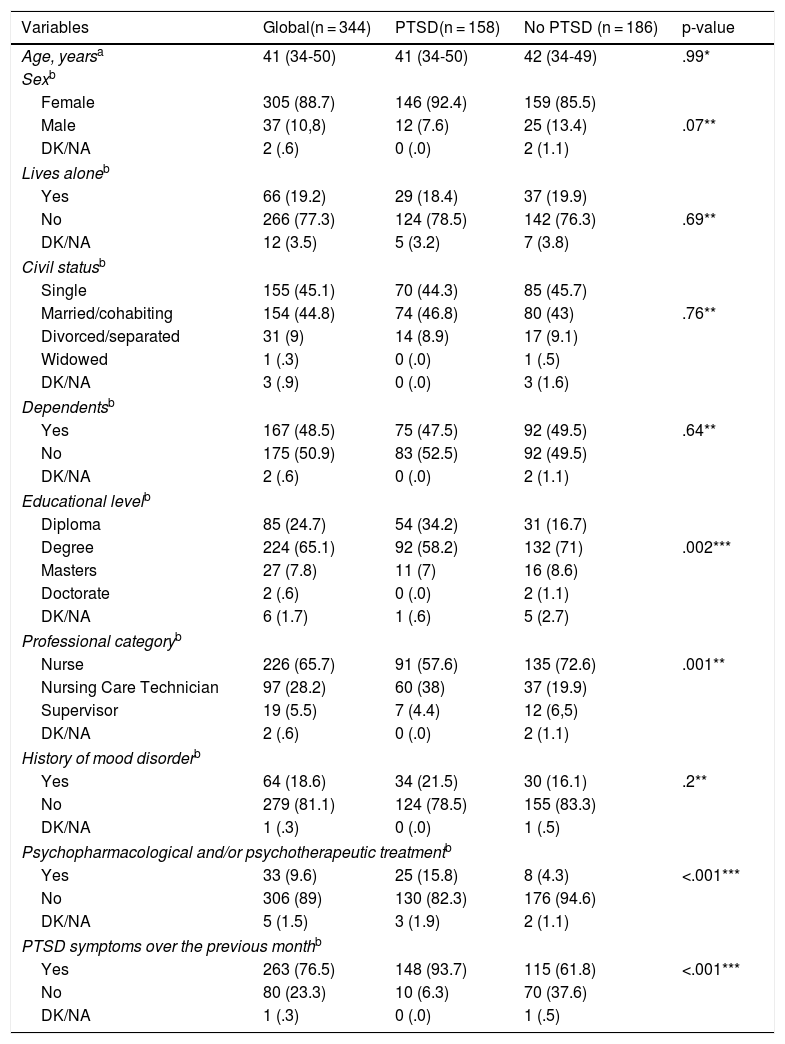
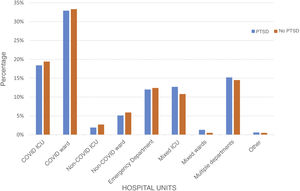
Of the 344 participants, 305 (88.7%) were women, with a median age of 41 years [34-50]. The sociodemographic and mental health characteristics of the sample are presented in Table 2. In this study, 322 professionals (93.6%) cared for infected patients, and their distribution by unit is shown in Fig. 1. Work and COVID-19 characteristics are presented in Table 3.
Socio-demographic and mental health characteristics of the sample and according to distribution of post-traumatic stress disorder.
| Variables | Global(n = 344) | PTSD(n = 158) | No PTSD (n = 186) | p-value |
|---|---|---|---|---|
| Age, yearsa | 41 (34-50) | 41 (34-50) | 42 (34-49) | .99* |
| Sexb | ||||
| Female | 305 (88.7) | 146 (92.4) | 159 (85.5) | |
| Male | 37 (10,8) | 12 (7.6) | 25 (13.4) | .07** |
| DK/NA | 2 (.6) | 0 (.0) | 2 (1.1) | |
| Lives aloneb | ||||
| Yes | 66 (19.2) | 29 (18.4) | 37 (19.9) | |
| No | 266 (77.3) | 124 (78.5) | 142 (76.3) | .69** |
| DK/NA | 12 (3.5) | 5 (3.2) | 7 (3.8) | |
| Civil statusb | ||||
| Single | 155 (45.1) | 70 (44.3) | 85 (45.7) | |
| Married/cohabiting | 154 (44.8) | 74 (46.8) | 80 (43) | .76** |
| Divorced/separated | 31 (9) | 14 (8.9) | 17 (9.1) | |
| Widowed | 1 (.3) | 0 (.0) | 1 (.5) | |
| DK/NA | 3 (.9) | 0 (.0) | 3 (1.6) | |
| Dependentsb | ||||
| Yes | 167 (48.5) | 75 (47.5) | 92 (49.5) | .64** |
| No | 175 (50.9) | 83 (52.5) | 92 (49.5) | |
| DK/NA | 2 (.6) | 0 (.0) | 2 (1.1) | |
| Educational levelb | ||||
| Diploma | 85 (24.7) | 54 (34.2) | 31 (16.7) | |
| Degree | 224 (65.1) | 92 (58.2) | 132 (71) | .002*** |
| Masters | 27 (7.8) | 11 (7) | 16 (8.6) | |
| Doctorate | 2 (.6) | 0 (.0) | 2 (1.1) | |
| DK/NA | 6 (1.7) | 1 (.6) | 5 (2.7) | |
| Professional categoryb | ||||
| Nurse | 226 (65.7) | 91 (57.6) | 135 (72.6) | .001** |
| Nursing Care Technician | 97 (28.2) | 60 (38) | 37 (19.9) | |
| Supervisor | 19 (5.5) | 7 (4.4) | 12 (6,5) | |
| DK/NA | 2 (.6) | 0 (.0) | 2 (1.1) | |
| History of mood disorderb | ||||
| Yes | 64 (18.6) | 34 (21.5) | 30 (16.1) | .2** |
| No | 279 (81.1) | 124 (78.5) | 155 (83.3) | |
| DK/NA | 1 (.3) | 0 (.0) | 1 (.5) | |
| Psychopharmacological and/or psychotherapeutic treatmentb | ||||
| Yes | 33 (9.6) | 25 (15.8) | 8 (4.3) | <.001*** |
| No | 306 (89) | 130 (82.3) | 176 (94.6) | |
| DK/NA | 5 (1.5) | 3 (1.9) | 2 (1.1) | |
| PTSD symptoms over the previous monthb | ||||
| Yes | 263 (76.5) | 148 (93.7) | 115 (61.8) | <.001*** |
| No | 80 (23.3) | 10 (6.3) | 70 (37.6) | |
| DK/NA | 1 (.3) | 0 (.0) | 1 (.5) | |
DK/NA: does not know/no answer; PSTD: post-traumatic stress disorder if Davidson Trauma Score ≥ 40.
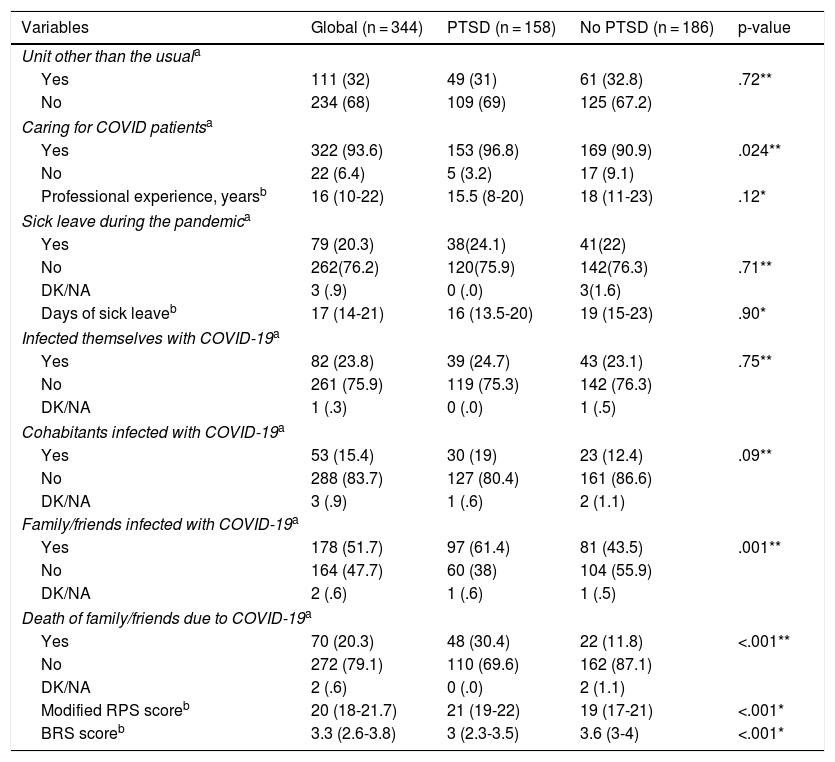
Work and relationship characteristics with COVID-19, modified Risk Perception Scale score, Brief Resilience Scale score, in the sample and according to onset of post-traumatic stress disorder.
| Variables | Global (n = 344) | PTSD (n = 158) | No PTSD (n = 186) | p-value |
|---|---|---|---|---|
| Unit other than the usuala | ||||
| Yes | 111 (32) | 49 (31) | 61 (32.8) | .72** |
| No | 234 (68) | 109 (69) | 125 (67.2) | |
| Caring for COVID patientsa | ||||
| Yes | 322 (93.6) | 153 (96.8) | 169 (90.9) | .024** |
| No | 22 (6.4) | 5 (3.2) | 17 (9.1) | |
| Professional experience, yearsb | 16 (10-22) | 15.5 (8-20) | 18 (11-23) | .12* |
| Sick leave during the pandemica | ||||
| Yes | 79 (20.3) | 38(24.1) | 41(22) | |
| No | 262(76.2) | 120(75.9) | 142(76.3) | .71** |
| DK/NA | 3 (.9) | 0 (.0) | 3(1.6) | |
| Days of sick leaveb | 17 (14-21) | 16 (13.5-20) | 19 (15-23) | .90* |
| Infected themselves with COVID-19a | ||||
| Yes | 82 (23.8) | 39 (24.7) | 43 (23.1) | .75** |
| No | 261 (75.9) | 119 (75.3) | 142 (76.3) | |
| DK/NA | 1 (.3) | 0 (.0) | 1 (.5) | |
| Cohabitants infected with COVID-19a | ||||
| Yes | 53 (15.4) | 30 (19) | 23 (12.4) | .09** |
| No | 288 (83.7) | 127 (80.4) | 161 (86.6) | |
| DK/NA | 3 (.9) | 1 (.6) | 2 (1.1) | |
| Family/friends infected with COVID-19a | ||||
| Yes | 178 (51.7) | 97 (61.4) | 81 (43.5) | .001** |
| No | 164 (47.7) | 60 (38) | 104 (55.9) | |
| DK/NA | 2 (.6) | 1 (.6) | 1 (.5) | |
| Death of family/friends due to COVID-19a | ||||
| Yes | 70 (20.3) | 48 (30.4) | 22 (11.8) | <.001** |
| No | 272 (79.1) | 110 (69.6) | 162 (87.1) | |
| DK/NA | 2 (.6) | 0 (.0) | 2 (1.1) | |
| Modified RPS scoreb | 20 (18-21.7) | 21 (19-22) | 19 (17-21) | <.001* |
| BRS scoreb | 3.3 (2.6-3.8) | 3 (2.3-3.5) | 3.6 (3-4) | <.001* |
BRS: Brief Resilience Scale; DK/NA: does not know/no answer; PTSD: post-traumatic stress if Davidson Trauma Score ≥ 40 RPS: modified Risk Perception Scale.
The items of the RPS are presented by percentages in Table 4. Item 8 had the highest mean score (2.8 [SD .52]) and item 7 had the lowest score (1.15 [SD .46]). The median of the modified RPS was 20 [18-21.7] (Table 3).
Proportion of answers according to Risk Perception Scale items.
| RPS items | Answer Yesa | Answer Sometimesa | Answer Noa |
|---|---|---|---|
| 1. I felt that my job was putting me at risk | 243 (70.6) | 80 (23.3) | 21 (6.1) |
| 2. I felt extra stress at work | 275 (79.9) | 45 (13.1) | 23 (6.7) |
| 3. I was afraid of becoming ill with COVID-19 | 190 (55.2) | 76 (22.1) | 78 (22.7) |
| 4. I felt that I had little control over becoming infected | 155 (45.1) | 140 (40.7) | 48 (14) |
| 5. I felt I had adequate protective equipment and/or training to protect myself | 196 (57) | 111 (32.3) | 33 (9.6) |
| 6. I felt that I would be unlikely to survive if I had COVID-19 | 15 (4.4) | 72 (20.9) | 257 (74.7) |
| 7. I thought about leaving my job because of COVID-19 | 14 (4.1) | 24 (7) | 306 (89) |
| 8. I was afraid of transmitting COVID-19 to others | 292 (84.9) | 31 (9) | 19 (5.5) |
| 9. My family and friends were worried they could become infected through me or that I would become infected | 88 (25.6) | 37 (10.8) | 219 (63.7) |
| 10. People avoided me or my family because of my work | 79 (23) | 72 (20.9) | 190 (55.2) |
| Altruistic item. Because I wanted to help patients with COVID-19, I was willing to accept the risks associated with it | 232 (67.4) | 75 (21.8) | 33 (9.6) |
RPS: Risk Perception Scale.
The median BRS was 3.3 [2.6-3.8] in the sample, with higher scores in the group without PTSD (Table 3). The median DTS score was 35.5 [17.25-60]. Of the professionals, 45.9% (n = 158) had a score ≥ 40 (Tables 2 and 3), this therefore suggests that they might have PTSD.
The analysis to find associations between onset of PTSD (DTS ≥ 40) and the other variables showed statistically significant differences as presented in Tables 2 and 3. No statistically significant difference was found between onset of PTSD and the work unit (Fig. 1).
A statistically significant, moderate, and inversely proportional linear relationship was found between the BRS score and the DTS score (r = -.410, p < .001). A statistically significant, moderate, and directly proportional linear relationship was also found between the DTS score and the modified PRS score (r = .423, p < .001).
After including the variables in the binary logistic regression model (Table 5), the following variables showed an impact on the development of PTSD using the multivariate model: having PTSD symptoms in the month prior to answering the questionnaire (OR = 6.1, 95% CI [2.68-14.03]), having had a family member or friend die from COVID-19 (OR = 2.3, 95% CI [1.22-4.39]), and having higher scores on the modified PRS (OR = 1.1, 95% CI [1.07-1.31]) increased the risk of developing PTSD. However, higher BRS scores (OR = .4, 95% CI [.31-.68]) were associated with a lower occurrence of PTSD (Fig. 2).
Binary logistic regression: bivariate analysis of post-traumatic stress disorder and socio-demographic, occupational, COVID-related, mental health-related, risk perception and resilience variables.
| Variables | B | SE | Wald | p | OR | 95% CI for OR |
|---|---|---|---|---|---|---|
| Age | -.010 | .030 | .121 | .728 | .990 | .933-1.050 |
| Professional experience | .008 | .031 | .063 | .801 | 1.008 | .948-1.072 |
| Sex (male reference) | .529 | .485 | 1.189 | .276 | 1.698 | .656-4.396 |
| Living alonea | .351 | .403 | .759 | .384 | 1.420 | .645-3.126 |
| Civil status | ||||||
| Single | Reference | |||||
| Married/cohabiting | .218 | .443 | .242 | .623 | 1.243 | .522-2.962 |
| Divorced/separated | -.348 | .630 | .304 | .581 | .706 | .205-2.428 |
| Widowed | -21.966 | 40192.9 | .000 | 1.000 | .000 | .000- |
| Professional | ||||||
| Supervisor | Reference | |||||
| Nurse | -.602 | .661 | .830 | .362 | .548 | .150-2.000 |
| NCT | .773 | 1.052 | .539 | .463 | 2.165 | .275-17.035 |
| Educational level | ||||||
| Masters/doctorate | Reference | |||||
| Diploma | -.168 | .907 | .034 | .853 | .845 | .143-5.003 |
| Degree | -.253 | .505 | .250 | .617 | .777 | .289-2.089 |
| Dependentsa | -.604 | .374 | 2.609 | .106 | .547 | .263-1.138 |
| History of mood disordera | -.358 | .379 | .891 | .345 | .699 | .333-1.470 |
| Psychopharmacological and/or psychotherapeutic treatmenta | .987 | .565 | 3.048 | .081 | 2.683 | .886-8.124 |
| Infected themselves with COVID-19a | -.744 | .617 | 1.453 | .228 | .475 | .142-1.594 |
| Cohabitants infected with COVID-19a | .780 | .444 | 3.088 | .079 | 2.182 | .914-5.211 |
| Family/friends infected with COVID-19a | -.063 | .314 | .040 | .841 | .939 | .508-1.737 |
| Death of family/friends due to COVID-19a | .648 | .365 | 3.151 | .076 | 1.911 | .935-3.906 |
| PTSD symptoms during the previous montha | 1.841 | .456 | 16.314 | .000 | 6.301 | 2.579-15.395 |
| Sick leave during the pandemica | .991 | .769 | 1.660 | .198 | 2.695 | .597-12.171 |
| Days of sick leavea | -.015 | .036 | .171 | .679 | .985 | .918-1.057 |
| Unit other than the usuala | .036 | .329 | .012 | .914 | 1.036 | .544-1.974 |
| Caring for COVID-19 patientsa | .871 | .670 | 1.690 | .194 | 2.389 | .643-8.883 |
| Modified RPS score | .154 | .055 | 7.720 | .005 | 1.166 | 1.046-1.300 |
| BRS score | -.798 | .217 | 13.579 | .000 | .450 | .294-.688 |
Coding = PTSD (1) and no PTSD (0); BRS: Brief Resilience Scale; CI: confidence interval; OR: odds ratio; RPS: Risk Perception Scale; SE: standard error; NCT: nursing care technician; PTSD: post-traumatic stress disorder.
The results show that nurses had a high prevalence of PTSD (45.9%) one month after contingency measures had ended. Similar figures have been reported in healthcare professionals in areas where the pandemic has been particularly severe, such as northern Italy (52.8%)8 or Madrid (56.6%),2 with nurses showing the highest prevalence,2,17,18 and this professional category is described as a risk factor for development of PTSD.17 We should exercise caution when comparing the different studies due to the variability of the instruments used.
In terms of socio-demographic characteristics, the professionals educated to intermediate vocational training level and the NCTs had higher levels of PTSD. Previous studies during the pandemic associated the presence of PTSD with educational level, with lower levels of PTSD in health professionals with higher academic training, such as bachelor's, master’s, or doctorate degrees.2,9,17 These results could be explained by better development of coping strategies during academic training. In terms of professional category, most of the PTSD sufferers have a lower academic level, and deliver care that involves more contact with infected patients, such as hygiene and nutrition, and therefore greater exposure.
We found no relationship between PTSD and female sex, unlike previous studies19–22 but, from the results, it is evident that a larger sample is needed to reach statistical significance.
In terms of mental health characteristics, the need for psychopharmacological and/or psychotherapeutic treatment during the pandemic and the onset of PTSD-related symptoms during the month prior to completing the questionnaire increased the incidence of PTSD, and the presence of symptoms was considered a risk factor, with a 6-fold greater likelihood of suffering from PTSD. This is not surprising, since a confirmed diagnosis of PTSD requires these symptoms to be maintained for more than one month.5 Although the study did not distinguish between treatments received before the pandemic and those started after it, there was no association between a history of mood disorder and the onset of PTSD, and therefore it seems that these treatments were used acutely over that period as insomnia, stress and anxiety increased.8
In relation to work characteristics, about 30% of the professionals worked in a different unit to their usual unit, but this did not seem to influence the development of PTSD. Nor was there any particular unit with a higher concentration of PTSD. Almost half the staff in each unit had PTSD, following a similar distribution to that presented in the overall sample. Care of COVID patients did not play a role, unlike that described in different studies,9,11,23 possibly due to the few professionals who did not care for these patients. In addition, all the nurses were affected in some way by the contingency plans. They were obliged to move to different departments and the vast majority were in contact with COVID patients, which increased the likelihood of contagion and working in isolation conditions using personal protective equipment that made it difficult to perform procedures, creating visual and auditory barriers. Many of the professionals who remained in their unit cared for patients with different diseases to those they were accustomed to, and others had to work in improvised spaces.24 Professional experience was not shown to be a determining factor in the development of PTSD. In the evidence, there are discrepancies with the relationship between both variables.2,9,17,18,23 It is possible that nurses with less experience adapt better to forced change, as they have unstable contracts that entail greater mobility, and nurses with more experience may compensate for more difficult adaptation with more knowledge.
We could not establish a relationship between PTSD and self-infection with COVID (as in the study by Luceño-Moreno et al.2), nor with infection by cohabitants, friends, or relatives. However, the death of friends or relatives doubled the likelihood of developing PTSD. This factor has previously been described as a predisposing factor for the development of mental illness.12,25 It should be noted that the development of PTSD depends not only on the type of exposure event, but also on the frequency and intensity of anxiety.26 Nursing professionals who experienced the death of a loved one, were not able to carry out their farewell rituals due to the restrictions, thus prolonging their grief and, in these circumstances, continued to face the illness in their jobs and therefore repeatedly relive this event.
With respect to the variables making up the RPS, it is evident how the nursing team assumes the role of caregiver in the work environment, as well as in the family and in the community, as they are willing to assume the risk of contracting the disease to deliver the care required by patients. This extends to their private lives, with 20% fearing infection of their loved ones more than being infected themselves. Moreover, although it is reported that the work entailed significant risk, professionals were willing to take this risk because they wanted to help. Studies describe how nurses feared passing on the disease to their family, but also felt professionally valued and proud.27 They were also willing to work on the front line, making it a protective factor for mental health.28
The RPS score is high in the present study, as in other similar studies.28,29 In addition, a high RPS score was found to increase the likelihood of developing PTSD by 17%, as it did during the 2003 SARS epidemic.12,18 Therefore, it is not the exposure to a risky environment per se that can trigger PTSD, as described in several studies,18 but the extent to which the risk of exposure is perceived due to fear of infection.
The median resilience score was 3.3, similar to the study by Luceño-Moreno et al.2 If we consider that the highest score on this scale is 5, the score obtained can be improved. Furthermore, in different studies resilience appears as a protective factor against the development of PTSD,2,9,28 as in the present study, in which a high resilience score prevented the likelihood of developing this illness by 54%.
Given the relationship between resilience and PTSD, it would be useful to work on increasing this skill. A way of increasing it would be through the implementation of educational interventions such as group training sessions on stress coping models or training in emotional education and skills such as relaxation, assertiveness, and self-control.18
More general measures aimed at improving the feeling of control and reducing the perception of risk are also necessary.23 The most important of these are to provide the worker with information in advance and institutional support to ensure provision of protective equipment and access to psychological interventions. Other interventions that facilitate the well-being of the professional are appropriate rest with regular work shifts, voluntary relocation of care services, and the possibility of alternative accommodation that reduces the risk of infecting family members or cohabitants.23
Although in a significant percentage of PTSD sufferers symptoms remit over time without requiring intervention,30 those involved in delivering care are most at risk for the long-term consequences of PTSD. Specifically in epidemic contexts, the prevalence of PTSD remained in 10% of healthcare workers 3 years after the onset of PTSD.12,30
The data obtained and the evidence suggest the need for future longitudinal studies to assess the prevalence, incidence, and evolution of PTSD and its long-term consequences, as well as the interventions implemented in the socio-occupational-health context.
This study had some limitations. Firstly, convenience sampling was used, which may have resulted in selection bias and overestimated the results. Secondly, the collection of data through self-administered questionnaires may have implied a response bias. Finally, the RPS scale has good internal consistency but has not been validated by psychometric studies and the DTS scale has not been used in other current studies, which makes it difficult to compare results.
In conclusion, we observed a high prevalence of PTSD in nursing staff in the present study. Factors such as the onset of PTSD symptoms during the previous month, the death of family members or friends due to COVID-19, and a high perception of risk influenced onset of the condition. Resilience was shown to be a protective factor.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank our colleagues at the Hospital Universitario Doce de Octubre for participating in the study and for their commendable work over the past year.
Please cite this article as: Blanco-Daza M, de la Vieja-Soriano M, Macip-Belmonte S, Tercero-Cano MdC. Trastorno de estrés postraumático en personal de enfermería durante la pandemia de COVID-19. Enferm Clin. 2022;32:92–102.