To determine the incidence of dependence-related skin lesions (DRSL) in patients in prone position (PP) and to identify the predisposing factors.
MethodFollow-up study in two polyvalent intensive care units. Patients undergoing invasive mechanical ventilation and PP with no skin lesions on admission were included. We recorded the 3 types of DRSL: (pressure ulcers [PU], moisture-associated skin damage [MASD] and friction injuries [FI]), demographic variables, diagnosis, length of stay, PP episodes, postural changes, APACHE II (Acute Physiology and Chronic Health Disease Classification System), prealbumin level on admission, body mass index (BMI), diabetes, hypertension, smoking, peripheral vascular disease (PVD), vasoactive drugs, Braden scale and mortality. Bivariate analysis: chi-square test, t-test or Mann–Whitney U test. Multivariate analysis: logistic regression.
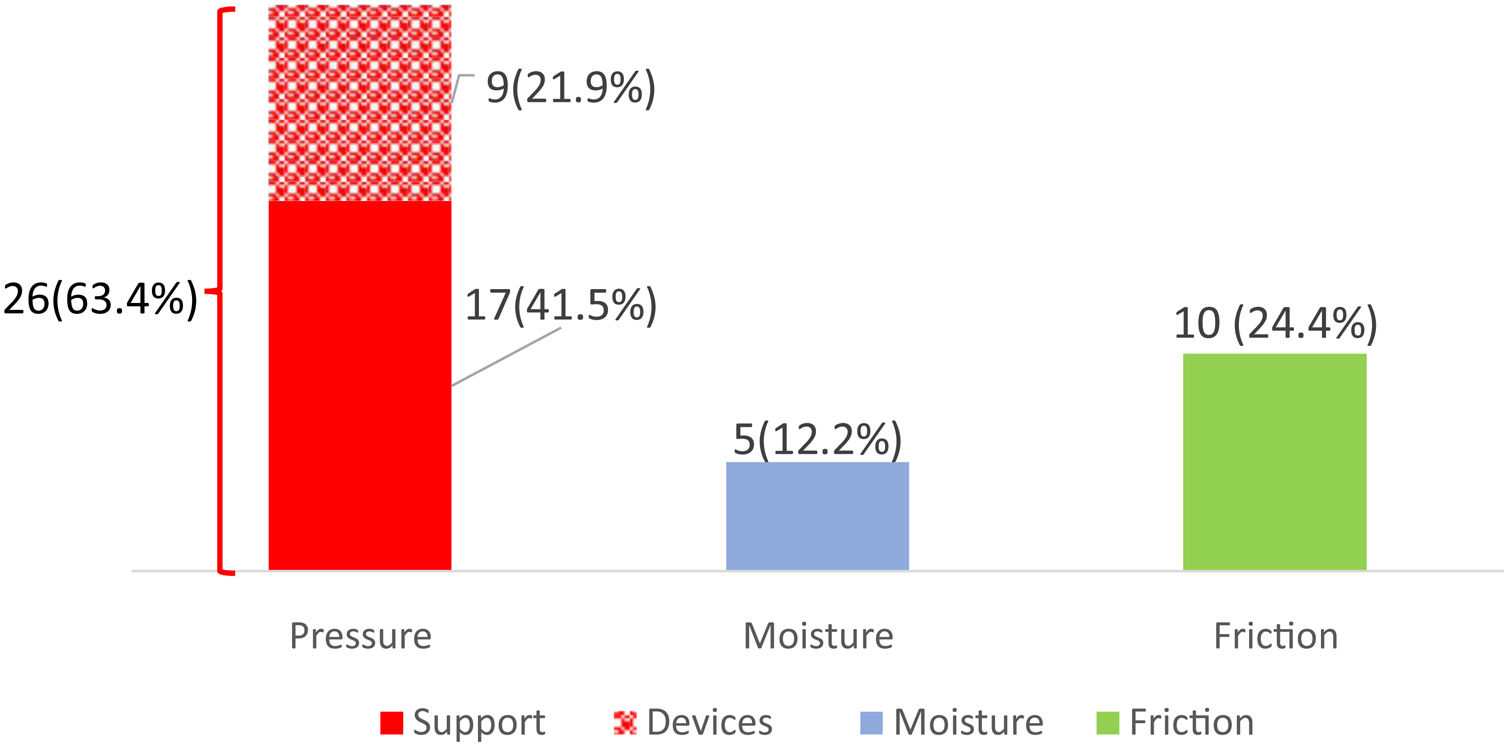
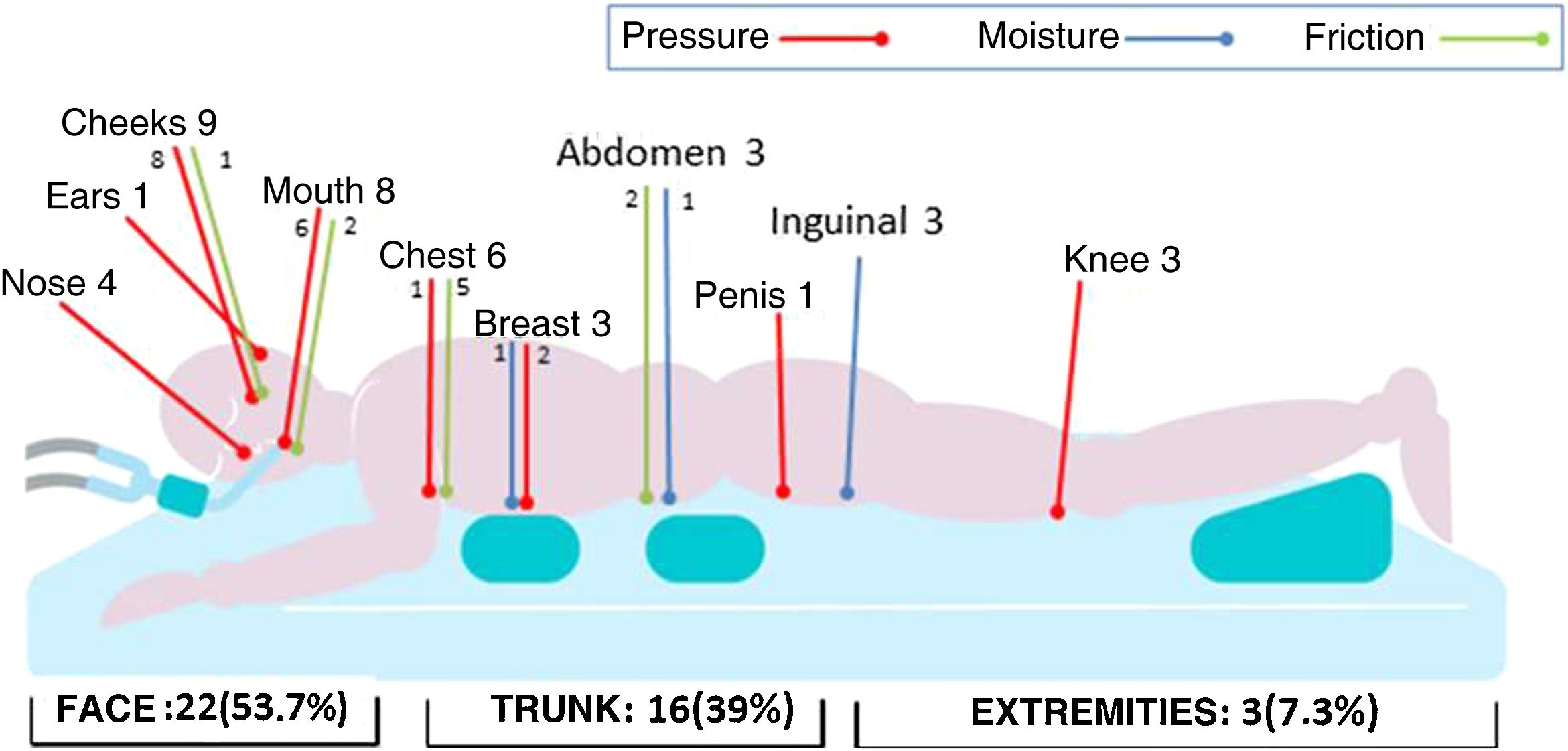
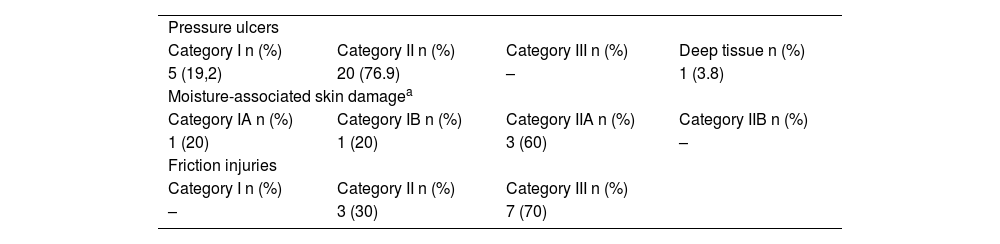
ResultsForty nine patients were included and 170PP were performed.Forty-one DRSL appeared in 22 patients with a cumulative incidence of 44.9% (95%CI: 31.6–58.7). PU accounted for 63.4% (73.1% facial; 76.9% stage II), 12.2% were MASD (60% inguinal; 60% stage II) and 24.4% were FI (50% thoracic; 70% stage III).
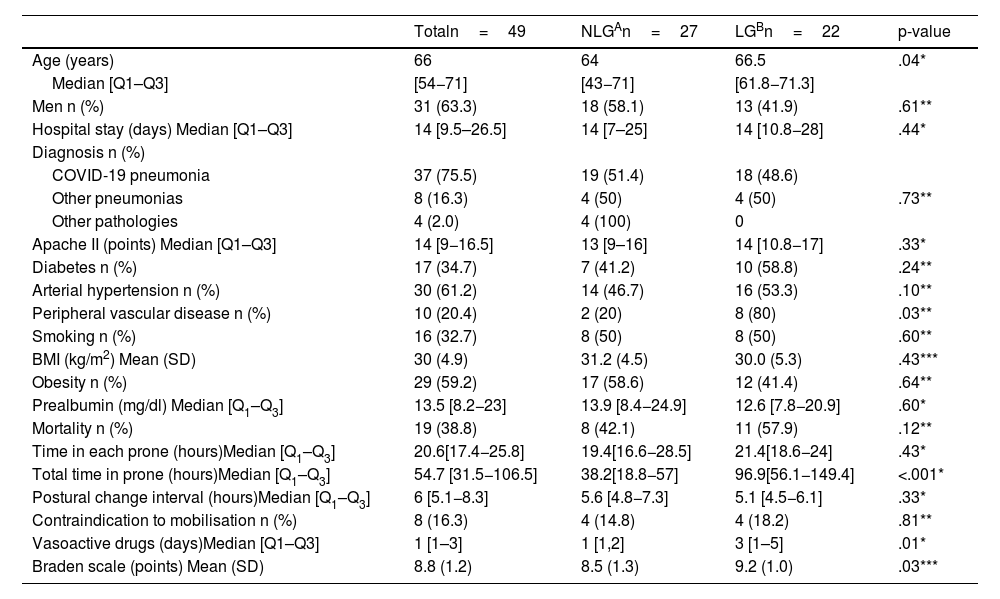
The median age of the lesion group (LG) was 66.5 [61.8−71.3] vs. 64 [43−71] years old in the non-lesion group (NLG), p=0.04. Eighty percent of the LG had PVD vs. 20% of the NLG, p=0.03. The median total hours on PP of the LG was 96.9 [56.1−149.4] vs. 38.2 [18.8−57] of the NIG, p<0.001. Multivariate analysis selected total PP hours (OR=1.03; 95%CI:1.01–1.05) and PVD (OR=8.9; 95%CI:1.3–58.9) as predisposing factors for developing DRSL.
ConclusionsThere is a high incidence of skin lesions related to prone decubitus dependence, mostly pressure lesions, although of low severity.The accumulated hours in probe position and peripheral vascular disease favor their development.
Determinar la incidencia de lesiones cutáneas relacionadas con la dependencia (LCRD) en pacientes en decúbito prono (DP) e identificar los factores predisponentes.
MétodoEstudio descriptivo-longitudinal en dos unidades de cuidados intensivos (UCI) polivalentes. Se incluyeron pacientes con ventilación mecánica invasiva y DP, sin lesiones al ingreso. Se registraron 3 tipos de LCRD: (lesiones por presión [LPP], lesiones cutáneas asociadas a la humedad [LESCAH] y lesiones por fricción [LF]), variables demográficas, diagnóstico, estancia, episodios en DP, cambios posturales, APACHE II (Acute Physiology and Chronic Health Disease Classification System), prealbúmina al ingreso, índice de masa corporal (IMC), diabetes, hipertensión arterial, tabaquismo, enfermedad vascular periférica (EVP), drogas vasoactivas, escala Braden y mortalidad. Análisis bivariante: prueba de χ2, t-Student o U de Mann–Whitney. Multivariante: regresión logística.
ResultadosSe incluyeron 49 pacientes. Se realizaron 170 DP. Aparecieron 41 LCRD en 22 pacientes con una incidencia acumulada de 44,9% (IC95%:31,6–58,7). El 63,4% LPP (73,1% faciales;76,9% categoría II), el 12,2% LESCAH (60% inguinales; 60% categoría II) y el 24,4% LF (50% torácicas; 70% categoría III). La mediana de edad del grupo con lesiones (GCL) fue de 66,5 [61,8–71,3] frente al 64 [43−71] años del grupo sin lesiones(GSL), p=0,04. El 80% del GCL tenía EVP frente al 20% del GSL, p=0,03. La mediana de horas totales en DP del GCL fue 96,9 [56,1–149,4] frente a 38,2 [18,8–57] del GSL, p<0,001. El análisis multivariante seleccionó horas totales DP (OR=1,03; IC95%:1,01−1,05) y la EVP (OR=8,9; IC95%:1,3–58,9) como factores predisponentes para desarrollar LCRD.
ConclusionesExiste una elevada incidencia de lesiones cutáneas relacionadas con la dependencia en decúbito prono, mayoritariamente lesiones por presión, aunque de baja severidad. Las horas acumuladas en decúbito prono y la enfermedad vascular periférica favorecen su desarrollo.