To determine the impact that the COVID-19 pandemic has had on health professionals, in terms of work changes and mental health.
Method1) Cross-sectional study and 2) longitudinal prospective study on health professionals who worked directly with patients affected by COVID-19 pandemic during the period between March-June 2020 in a tertiary hospital in Barcelona. Baseline (July-November 2020) and follow-up (November 2020-March 2021) data were collected. Data related to the job and toxic habits were collected with ad hoc questionnaires, and data related to perceived stress, post-traumatic stress, depression, and anxiety using validated questionnaires.
ResultsIn the baseline group (cross-sectional study), 90 professionals participated, 76% nurses. More than a third were on sick leave or took drugs to manage stress. Half of smokers increased tobacco use, and one in 5 increased alcohol consumption. Habitual shift change is significantly associated with depression, professional profile with anxiety, and perceived stress with age. In the longitudinal prospective study, the follow-up group (n = 64) shows high levels of stress and anxiety, which are maintained or even significantly increased over time.
ConclusionsThe structural changes that occurred in the hospital during the first wave of the COVID-19 pandemic had a strong impact on professionals, many of them presenting an increase in toxic habits, as well as impaired mental health that is maintained over time.
Determinar el impacto que ha tenido la pandemia COVID-19 en profesionales sanitarios, en términos de cambios laborales y de salud mental.
Método1) Estudio transversal y 2) estudio longitudinal prospectivo sobre profesionales de la salud que trabajaron de forma directa con pacientes afectados por la pandemia COVID-19 durante el periodo comprendido entre marzo-junio de 2020 en un hospital de tercer nivel de Barcelona. Se recogieron datos basales (julio-noviembre de 2020) y de seguimiento (noviembre de 2020-marzo de 2021). Se recogieron datos relacionados con el puesto de trabajo y hábitos tóxicos con cuestionarios ad hoc, y de estrés percibido, estrés postraumático, depresión y ansiedad mediante cuestionarios validados.
ResultadosEn el grupo basal (estudio transversal) participaron 90 profesionales, 76% enfermeras. Más de un tercio estuvo de baja o tomó fármacos para gestionar el estrés. La mitad de los fumadores aumentó el consumo de tabaco, y uno de cada 5 aumentó el consumo de alcohol. Se asocia de forma significativa el cambio de turno habitual con la depresión, el perfil profesional con la ansiedad, y el estrés percibido con la edad. En el estudio longitudinal, el grupo de seguimiento (n = 64) muestra niveles elevados de estrés y ansiedad, que se mantienen o incluso aumentan en el tiempo de forma significativa.
ConclusionesLos cambios estructurales acontecidos en el hospital durante la primera ola de la pandemia por la COVID-19 tuvieron un fuerte impacto en los profesionales, presentando muchos de ellos un aumento en los hábitos tóxicos, así como una salud mental alterada que se mantiene en el tiempo.
- -
The outbreak of the COVID-19 pandemic has had a strong emotional impact on healthcare professionals.
- -
The mental health of healthcare professionals has been affected by the outbreak of the COVID-19 pandemic.
- -
Nurses' work environment is associated with patient health outcomes.
- -
The impact on the mental health of professionals due to the outbreak of the COVID-19 pandemic has been significant and is sustained over time.
- -
Age, change of location or professional profile are associated with professionals' mental health.
- -
There has been an increase in the toxic habits of healthcare professionals directly related to the outbreak of the COVID-19 pandemic.
The current COVID-19 pandemic has led to mental health issues across the population,1 with reports of serious levels of stress, depression, insomnia, decreased perceived quality of life, and even higher rates of suicide.2,3 In the case of healthcare professionals, there has been a high prevalence of insomnia and post-traumatic stress disorder, anxiety disorders, and depression,2,4 as in previous pandemics,5 with nurses in particular suffering the highest rates, as was the case in 2003 with the SARS-CoV-16 outbreak. Indeed, previous pandemic situations have required a rapid and intense response from healthcare professionals, who were already exposed to numerous physical and emotional stressors, such as increased workloads, physical exhaustion, inadequate protective equipment, and decision making that could have posed ethical challenges.7,8
Post-traumatic stress9 can develop after experiencing a shocking or dangerous event, and anxiety disorders and their diagnosis include symptoms such as reliving the traumatic event, avoidance, negative or blaming thoughts, irritability, insomnia or difficulty concentrating, among others. People with anxiety disorders may also have fatigue, physical symptoms and difficulty controlling feelings of worry.10 People affected by depression have feelings of pessimism and hopelessness, sadness, loss of interest, physical symptoms, and even thoughts and behaviours of death or suicide.11 An increase in the latter was reported in Spanish healthcare professionals during the first wave of the COVID-1912 pandemic.
The persistence of this type of symptomatology, together with uncertainty and heavy workloads can also lead to burnout in health professionals who have been on the front line of the COVID-1913 pandemic.
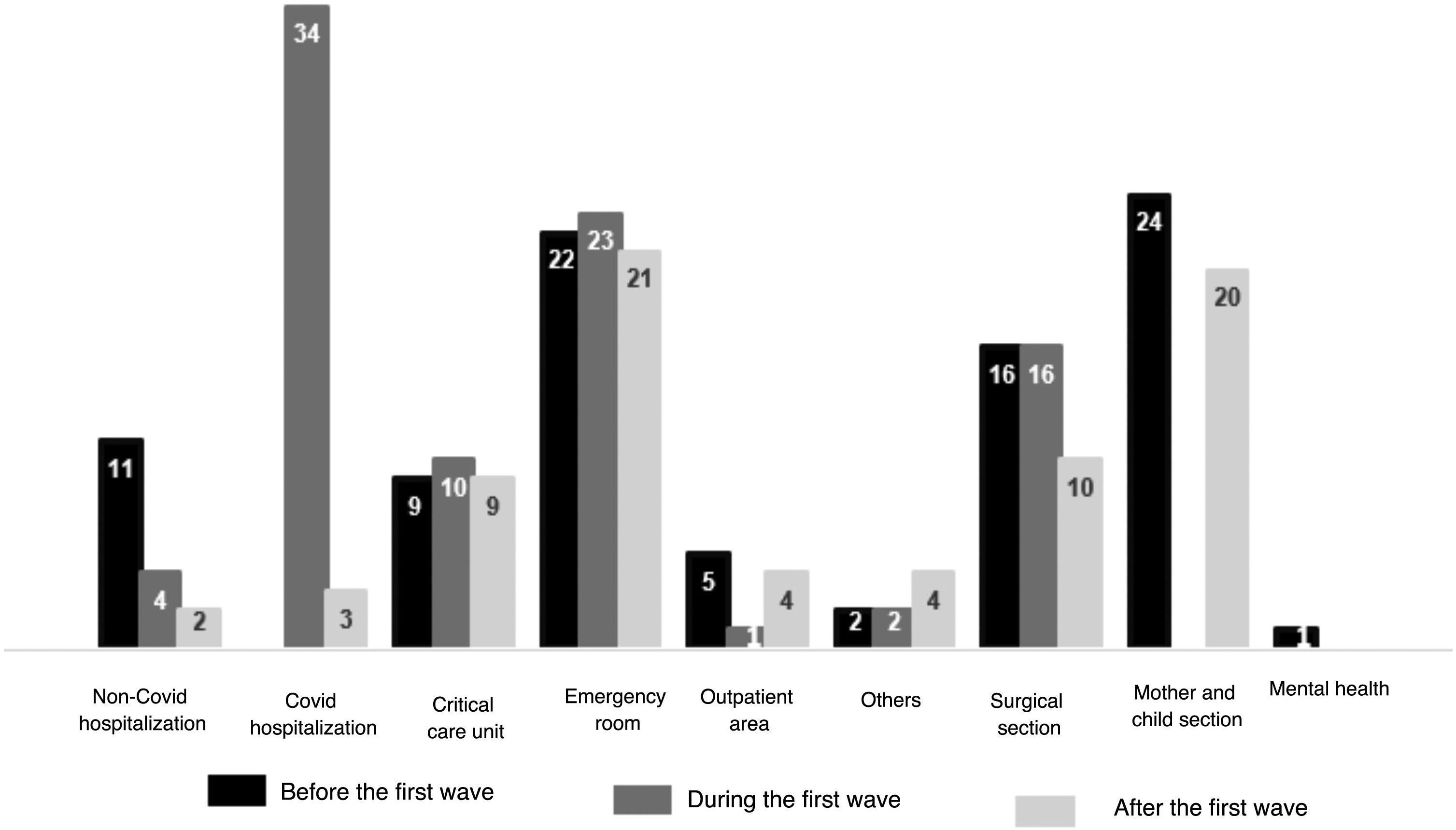
With the outbreak of the first wave of the COVID-19 pandemic, the Hospital del Mar in Barcelona changed its portfolio of services in 15 days: specialties were diverted, scheduled surgery was halted, and COVID-19 patients accounted for 73.33% of hospital occupancy. The high demand for hospital beds meant that spaces had to be made available to admit patients, increasing the hospital's capacity by 50% at the busiest times. In many cases, in addition to the change in patient profile, this involved changes in professionals’ location, schedules, and work crews for more than three months. Understanding healthcare professionals' mental health at these times of health crisis, as well as how it evolves over time and what factors may be associated with it, is critically important in order to be able to take specific actions, and even to rethink possible actions should similar situations arise in the future. Therefore, the objectives of this study are to determine the status of the mental health of healthcare professionals who worked on the front line during the first wave of the COVID-19 pandemic and to establish possible associations with occupational factors (cross-sectional study,) in addition to the evolution of their mental health after 4 months (longitudinal study).
Method1) Cross-sectional study and 2) prospective, longitudinal, cohort study conducted at the Hospital del Mar in Barcelona from July 2020 to April 2021.
Hospital del Mar is a tertiary acute care hospital located near the centre of Barcelona, with a 470-bed capacity and different levels of care (conventional hospitalisation, surgical complex, intensive care unit, mother and child unit, outpatient clinics, and day hospital).
This study is part of the «ES-3-PT: early detection of vulnerability to post-traumatic stress disorder (PTSD) in populations at high risk of exposure to COVID-19»1 project, in which, at the same time as questionnaires were being completed, electrophysiological measurements were taken with the aim of validating a device for early stress detection.
Variables and assessment instruments: 1) socio-demographic, occupational, and other data specific to the study: age, sex, location, shift (in the context studied, the work shifts are mostly fixed: morning shift, afternoon shift, night shift, and split shift (from 8:00 to 17:00). However, some professionals alternate more than one shift; in this case, it is categorised as “various”), hours worked, alcohol/ tobacco/ drug use, demand for psychological help. 2) Level of stress using a) the Spanish version of the Perceived Stress Scale (Escala de Estrés Percibido, PSS).14 The scale consists of 14 items with 5 possible ratings (never, almost never, occasionally, often, and very often) and a maximum score of 40; scores above 27 were classified as high stress. Participants also rated their level of stress using a numerical scale (NS) from 0 to 100, with cut-off points established according to Aguiló Mir et al.15 b) Post-traumatic stress scale PCL-5,16 comprising 20 items with 5 possible ratings (not at all, a little, moderately, quite a bit, extremely); the maximum score is 80 and the threshold for possible post-traumatic stress is 30. 3) Anxiety, using the STAI17 scale that is composed of 20 items scored on a scale for each of its subscales (STAI-S and STAI-T)17; the highest score is 60 for each of them. The cut-off point for high anxiety has been set at 37 and 26, respectively,18 and 4) depression as quantified by the PHQ-2 questionnaire,19,20 which consists of 2 items and has a cut-off point of 3 to determine a possible diagnosis of depression.
Participants: doctors, nurses and auxiliary nursing care technicians (ANCTs) in active employment who were in direct contact with patients diagnosed with COVID-19 during the period of March-June 2020. Institutional outreach was carried out (intranet, heads of service, and supervisors), facilitating an email address to those interested in participating so that they could contact the study’s PI, who, after a face-to-face appointment (electrophysiological measurements) assigned them an ID and a link to answer the questionnaires via the Google forms platform. Informed consent was obtained. Baseline data were collected between July and November 2020); 4 months later (between November 2020 and March 2021), they were contacted a second time and asked to complete the questionnaires again via Google forms with the same personalised ID for follow-up purposes.
Once the questionnaires were collected at both time points, the resulting database was scrubbed and descriptive and bivariate analyses (Wilcoxon and McNemar or Stuart-Maxwell test for continuous or categorical variables respectively) were performed with the statistical package STATA 15.1 (College Station, TX: StataCorp LLC). All results were interpreted with a 95% confidence interval (CI) and a significance level (p-value) of 0.05.
This study has been funded under the Supera Covid 2019 call for proposals,1 and has been approved by CEIm-PSMAR (2020/9406/I).
ResultsOf the 104 professionals recruited to carry out the electrophysiological measurements, 90 answered the questionnaires for the first measurement and 73 for the second. The follow-up group consisted of 64 professionals who answered the questionnaires on both occasions.
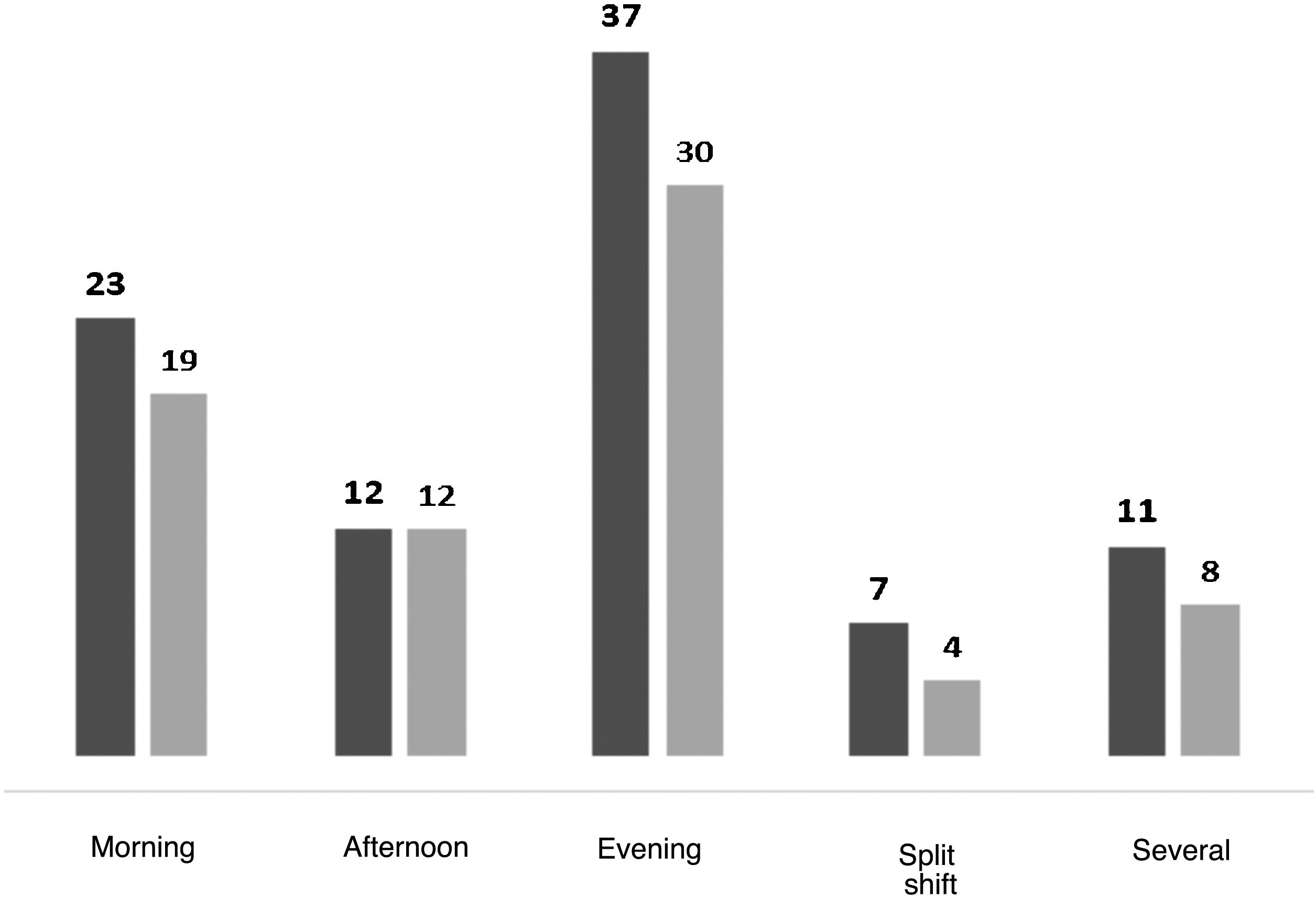
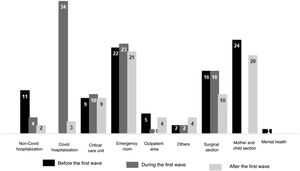
Measure 1: Initial group (n = 90)The median age was 39 years [min 22, max 64] and the mean age was 39.8 (SD 11.7), not following a normal distribution. All work shifts were represented as illustrated in Fig. 1. The before (usual location prior to the COVID-19 pandemic), during (period March-June 2020), and after (from July 2020 onwards) the first wave of the COVID-19 pandemic are detailed in Fig. 2.
Seventy-six per cent (76%) (n = 68) were nurses. During the first wave of COVID-19 (March-June 2020), 81% of the participants (n = 73) worked extra hours; 57% (n = 51) changed shifts and colleagues; 42% (n = 38) were on sick leave at some point; 27% (n = 24) sought professional help to manage their mental health, and 36.7% (n = 33) took medication for stress management. Of the 38 participants who were smokers, 50% (n = 19) increased their smoking, and of the 68 who did not claim to abstain from drinking [alcohol], 25% (n = 17) reported increased alcohol consumption.
Mean perceived stress was 17.66 out of a maximum of 40 (SD = 5.18) according to the PSS, and 47.07 out of 100 (SD = 22.36), based on the numerical scale. With regard to the PSS, 5.56% (n = 5) exhibited high levels of stress. As for the numerical scale, 23.3% (n = 21) had values categorised as high stress (≥70). High anxiety was scored by 11.11% (n = 10) of the participants on the state scale and 38.88% (n = 35) on the trait scale. On the subject of post-traumatic stress, the mean was 21.53 out of 80; 22 participants were found to have post-traumatic stress. Of the total sample, 18.18% of the participants had scores indicating susceptibility to depression (positive screening). Data on sociodemographic and stress-related variables are displayed in Tables 1 and 2.
Baseline group results (measure 1, n=90).
| Age | |
| Mean(SD) | 39.79 (11.71) |
| Median (Q1, Q3) | 39 (29.49) |
| Physical activity | n (%) |
| Usual | 33 (36.66) |
| Occasional | 41 (45.55) |
| Almost never | 16 (17.77) |
| Tobacco use | |
| Non-smoker | 52 (57.77) |
| Has not increased | 19 (21.11) |
| Has increased | 19 (21.11) |
| Alcohol consumption | |
| Non-drinker | 22 (24.44) |
| Has not increased | 51 (56.66) |
| Has increased | 17 (18.88) |
| Sick leave | |
| Yes | 38 (42.22) |
| Medication to manage stress | |
| Yes | 33 (36.66) |
| Has sought help | |
| Yes | 24 (26.67) |
SD: Standard Deviation; Q1: quartile 1; Q3: quartile 3.
Baseline group mental health results (measure 1, n=90).
| STAI-S | |
| Mean (SD) | 25.91 (7.97) |
| Median (Q1, Q2) | 28(19.33) |
| Low (≤10.53) | 4 (4.44) |
| Intermediate (>10.53 ≤ 37) | 76 (84.44) |
| High (>37) | 10 (11.11) |
| STAI-T | |
| Mean (Sd) | 21.94 (8.45) |
| Median (Q1, Q2) | 25(15.29) |
| Low (≤14) | 21 (23.33) |
| Intermediate (>15 ≤ 25) | 34 (37.77) |
| High (>25) | 35 (38.88) |
| PCL-5 | |
| Mean (SD) | 21.53 (11.69) |
| Median (Q1, Q2) | 19 (12.32) |
| >30 (positive screening) | 22 (24.44) |
| PSS | |
| Mean (SD) | 17.65 (4.60) |
| Median (Q1, Q2) | 18 (14.22) |
| Low (≤13) | 20 (22.22) |
| Moderate (14-25) | 65 (72.22) |
| High (≥26) | 5 (5.55) |
| NS (n = 104) | |
| Mean (SD) | 48.58 (22.15) |
| Median (Q1, Q2) | 50 (30.65) |
| Low (≤30) | 28 (31.81) |
| Moderate (31-70) | 39 (44.32) |
| High (≥71) | 21 (23.86) |
| PHQ-2 (n = 88) | |
| ≥3 (positive screening) | 16 (18.18) |
SD: Standard Deviation; PSS: Perceived Stress Scale; NS: Numerical Scale; PCL-5: Posttraumatic Stress Disorder Checklist for DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition); PHQ-2: Patient Health Questionnaire-2; Q1: Quartile 1; Q3: Quartile 3; STAI-S/T: State-Trait Anxiety Inventory -- State/ Trait.
A significant inverse association was noted between perceived stress and age (NS p = 0.042; PSS p = 0.047), between depression and having changed shifts (p = 0.049), and between anxiety (STAI-S) and professional profile (0.042), with higher anxiety levels detected among physicians, followed by nurses, and finally HCWs.
Variables in the follow-up group (n = 64)Perceived stress measured by the PSS revealed little change with respect to mean values and distribution by category. However, the values reported with NS did demonstrate significant changes, from a mean rating of 49.7 to 58.1 (p = 0.003), and from 16 to 27 participants reporting a high level of stress (≥71). As for anxiety, more participants with high anxiety scores (9 vs. 14) were observed on the STAI-S; the difference between the mean values obtained on the two measures attained statistical significance (p = 0.023). However, the STAI-T indicated an increase in the number of participants scoring in the Intermediate anxiety category, from 35.9% (n = 23) to 48.4% (n = 31). With regard to the post-traumatic stress measure, the results remained virtually unchanged (Table 3).
Stress-related variables in the follow-up group (n=64).
| Baseline (measure 1) | Final (measure 2) | ||||
|---|---|---|---|---|---|
| Mean (SD) | n (%) | Mean (SD) | n (%) | P* | |
| Median (Q1, Q3) | Median (Q1, Q3) | ||||
| PSS | |||||
| Mean (ST) | 17.8 (5.3) | 14 (21.9) | 18.6 (5.7) | 11 (17.2) | .174 |
| Median (Q1, Q3) | 18.0 (14.22) | 46 (71.9) | 18.5 (14.22) | 47 (73.4) | .368 |
| Low (≤13) | 4 (6.2) | 6 (9.4) | |||
| Moderate (14-25) | |||||
| High (≥26) | |||||
| NS (n = 63) | |||||
| Mean (SD) | 49.7 (21.7) | 16 (25.4) | 58.1 (23.0) | 14 (22.2) | .003* |
| Median (Q1, Q3) | 50.0 (30.70) | 31 (49.2) | 60.0 (40.75) | 22 (34.9) | .071 |
| Low (≤30) | 16 (25.4) | 27 (42.9) | |||
| Moderate (31-70) | |||||
| High (≥71) | |||||
| STAI-S | |||||
| Mean (SD) | 27.0 (8.7) | 1 (1.5) | 29.6 (9.9) | 0 | .023* |
| Median (Q1, Q3) | 25.0 (20.32) | 54 (84.4) | 29.0 (20.37) | 50 (78.1) | .195 |
| Low | 9 (14.1) | 14 (21.9) | |||
| Intermediate | |||||
| High | |||||
| STAI-T | |||||
| Mean (SD) | 22.9 (10.3) | 15 (23.5) | 23.9 (9.6) | 9 (14.1) | .085 |
| Median (Q1, Q3) | 22.0 (16.29) | 23 (35.9) | 22.5 (17.30) | 31 (48.4) | .174 |
| Low | 26 (40.6) | 24 (37.5) | |||
| Intermediate | |||||
| High | |||||
| PCL-5 | |||||
| Mean (SD) | 22.8 (14.0) | 16 (25) | 23.0 (14.4) | 17 (26.6) | 1.000 |
| Median (Q1, Q3) | 20.0 (12.31) | 20.0 (12.32) | |||
| PCL5+ | |||||
SD: Standard Deviation; PSS: Perceived Stress Scale; NS: Numerical Scale; PCL-5: Posttraumatic Stress Disorder Checklist for DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition); PHQ-2: Patient Health Questionnaire-2; Q1: quartile 1; Q3: quartile 3; STAI-S/R: State-Trait Anxiety Inventory -- State/ Trait.
The results obtained display high values of anxiety and stress in the group under study that were maintained and even increased over time. These results are slightly lower than those reported in a recent systematic review,21 as well as in studies carried out among nurses in Wuhan,22 but are consistent with those presented by Feingold et al.23 who also reported figures for post-traumatic stress, depression, and anxiety among 23.3 and 26.6% of the respondents in a large sample, despite having used different measurement instruments. In addition, the findings remained the same or went up over time, similar to the findings of Sasaki in Japan,24 despite having reversed the situation that provoked these symptoms in the context studied. This fact is cause for great concern, as it reflects the fact that an essential group is in a situation of vulnerability.
High workload, low staffing ratios, long work shifts, and high emotional demands have been associated with the appearance of burnout.25 All these characteristics have been prevalent in the various waves of the COVID-19 pandemic, and high burnout rates were found to be associated with health professionals having been on the front line of the pandemic,26 as well as with anxiety and depression.27 In addition to being associated with a decline in the number of cases of burnout, it has also been found to be associated with a reduction in the number of cases of anxiety and depression in health professionals. In addition to being correlated with diminished quality of care,28 burnout can lead to presenteeism, and nurses' presenteeism has been reported to be associated with negative health outcomes and high economic costs.29
Moreover, a high percentage of participants have been found to report drug use, as well as increased consumption of alcohol and tobacco to deal with the emotional situation during the first wave of the COVID-19 pandemic. The use of these types of substances and addictive behaviours in nurses has been reported to put patient safety at risk,30 thereby highlighting how the impact of the COVID-19 pandemic on healthcare professionals' mental health can have a direct bearing on the health outcomes of both patients and the professionals themselves.
Many professionals were found to have sought professional help. At the study hospital, the one2one_mar initiative, a psychological support programme for professionals, patients, and families, was launched at the beginning of the first wave (25/3/2021). This programme was staffed by psychologists, psychiatrists, nurses, and social workers from the same institution, all of whom were specialised in mental health. One2one provided online and/ or telephone resources to deal with situations of emotional distress arising from the COVID-19 pandemic. It is plausible that having access to this resource was a determining factor in the high figures encountered in this study, bearing in mind that during the data collection period of this study, one2one_mar provided services to 397 professionals.
Following the recommendations of recent studies,22 this study underscores the need to invest in resources to increase resilience and reduce stress in healthcare professionals. Failure to do so could further stress an already strained healthcare system, which could, in turn, have a negative impact on health outcomes for the population. While it is true that part of the responsibility for managing the situation lies with the individuals themselves, the implementation of palliative strategies (sessions focusing on resilience, risk behaviours, and stress management, the creation of groups to share experiences and coping strategies, access to information on emotional management), corrective strategies (greater professional recognition, stabilisation of shifts, locations, and workplaces, and developing more effective and efficient stress management strategies), and corrective approaches (greater professional recognition, stabilisation of shifts, locations, and work teams), support (accessibility to professional support teams) and follow-up (monitoring the variables related to professionals’ mental health) by the corresponding administrations and institutions could be extremely useful in improving health professionals’ mental health.
LimitationsThe global framework in which the study was carried out involved in-person electrophysiological measurements, in which participants were asked to voluntarily answer the questionnaires later on via an online platform. Consequently, a record was kept of the people who opted to participate, as they were contacted after 4 months to do the second recording of the electrophysiological variables. However, priority was given to confidentiality and the voluntary nature of answering the questionnaires so as to foster honesty and freedom in the answers, and this led to a loss of follow-up, as some professionals did not answer the questionnaires on either of the two occasions. For the same reason, it was not possible to know the reasons for dropping out.
Although the outreach was institutional and participation was open to the three professional groups (physicians, nurses, and ANCTs), the participating sample was basically made up of nurses. This may have been due to the fact that the person in charge of the study is a nurse who is well-known in different areas of the institution, so that the nursing collective may have felt greater proximity. However, and although it was not the intention of the study, this fact has shown a more accurate approximation to the state of the collective with greater representation of the health system.
It is possible that the information presents a participant bias, as it may have been that the people most affected were the ones who felt most motivated to participate. However, it should be noted that there were also a substantial number of professionals with a high degree of emotional distress who felt totally disengaged from the system and who were also unresponsive.
The fact that no sample size was determined beforehand and that the sampling was not randomised does not make it possible to extrapolate the results. The sample is small, possibly because of the overall situation of exhaustion. That being said, the figures yield relevant information about a representation of professionals that should be taken into account and that may also have occurred in settings that have experienced similar situations.
ConclusionsIn view of the results obtained in this study, the mental health of healthcare professionals has been negatively affected during the COVID-19 pandemic, with high levels of anxiety and stress that have been maintained over time. Likewise, an increase in addictive behaviours has also been observed in the group studied. Some factors already reported in the literature and which have also occurred in the context studied, such as the pressure of care, uncertainty or fear of contagion may have conditioned the results obtained, but other elements not previously reported, such as the excess number of hours worked or the changes in shifts and colleagues in the study population, may also have exerted a major impact on the healthcare professionals' mental health. Indicators of emotional exhaustion were maintained or increased in the health professionals studied. Situations of stress within the healthcare system, such as the one experienced during the COVID-19 pandemic, highlight the need and benefit of contemplating proactive psychological interventions for its professionals (as attested to by the high demand for the psychological support system set up by the hospital under study), as well as compensatory work environment strategies, such as professional recognition, participation in decision-making, stable teams, and support from leaders.
Ethical responsibilitiesThis study was approved by the Research Ethics Committee of the Parc de Salut Mar, CEIm-PSMAR (dossier: RP 2016/6858/I).
FundingThis study is part of the global "Early detection of stress and post-traumatic stress symptoms after high exposure to COVID-19” project, whose global PI is Jordi Aguiló Llobet and has been funded through the Supera Funds COVID-2019 call of the Santander Bank (Spain), in collaboration with Crue Universidades Españolas and the Centro Superior de Investigaciones Científicas (CSIC).
Conflict of interestsThe authors have no conflict of interests to declare.
To all the healthcare professionals who have been and continue to tackle the COVID-19 pandemic, and especially to the participants at the Hospital del Mar, who, despite experiencing perhaps the most challenging situation of their professional careers, selflessly chose to take part in this study.
To the management of the Hospital del Mar for allowing us to carry out and support the study.
To the Banco de Santander and the CRUE for funding the entire project.
https://www.crue.org/proyecto/fondo-supera-covid-19/Tercera resolución del Comité Evaluador.
Please cite this article as: Esteban-Sepúlveda S, Terradas-Robledo R, Castro-Ribeiro T, García-Pagès E, Sobregrau-Sangrà P, Lacueva-Pérez L. Pandemia COVID-19 sobre profesionales sanitarios en un hospital de tercer nivel en España: cambios laborales durante la primera ola, salud mental a los 4 meses y seguimiento a los 9 meses. Enferm Clin. 2022;32:143–151.