To describe the characteristics of case management in terms of population served, interventions, use of services and outcomes such as mortality, readmissions, pressure ulcers, falls, drug problems and institutionalisation.
MethodFollow-up study of a cohort, from the RANGECOM Multicentric Registry of Andalusia. The study population were patients included in the case management services of Health Centres and their family caregivers.
ResultsData from 835 patients with a mean age of 76.8years (SD: 12.1), 50.24% women, are presented. They had an important comorbidity (Charlson 3.1, SD: 2.5) and high dependence (Barthel 37.5, SD: 31.4). Sixty-two point two percent of the interventions deployed by the case managers were grouped into three domains: behavioural (26.0%), health system (20.2%) and safety (14.1%). Mortality was 34.4% and hospital admissions 38.1%. Patients with more hospital readmissions had more visits to the Emergency Department (OR: 1.41; 95% CI: 1.22–1.63), more telephone interventions by case managers (OR: 1.12; 95% CI: 1.02–1.24) and imaging tests (OR: 1.37; 95% CI: 1.17–1.60), together with greater caregiver burden (OR: 1.31; 95% CI: 1.08–1.59), the presence of medical devices at home (OR: 1.69; 95% CI: 1.00–2.87) and received less “Case Management” intervention.
ConclusionsThe patients who absorb the demand of case management nurses present high complexity, for which they deploy behavioural interventions, navigation through the health system and clinical safety.
Describir las características de la gestión de casos en cuanto a población atendida, intervenciones, utilización de servicios y los desenlaces mortalidad, reingresos, úlceras por presión, caídas, problemas con medicamentos e institucionalización.
MétodoEstudio de seguimiento de una cohorte a partir del registro multicéntrico RANGECOM de Andalucía. La población de estudio son pacientes atendidos en la cartera de servicios de gestión de casos de centros de salud y sus cuidadores familiares.
ResultadosSe presentan datos de 835 pacientes con edad media de 76,8años (DE: 12,1), un 50,24% mujeres. Presentan una comorbilidad importante (Charlson 3,1; DE: 2,5) y dependencia elevada (Barthel 37,5; DE: 31,4). El 60,2% de las intervenciones desplegadas por las gestoras de casos se aglutina en tres dominios: conductual (26,0%), sistema sanitario (20,2%) y seguridad (14,1%). La mortalidad fue del 34,4% y los ingresos hospitalarios, del 38,1%. Los pacientes con más reingresos hospitalarios tenían más visitas a urgencias (OR: 1,41; IC 95%: 1,22-1,63), más intervenciones telefónicas de las gestoras de casos (OR: 1,12; IC 95%: 1,02-1,24) y pruebas de imagen (OR: 1,37; IC 95%: 1,17-1,60), junto con un mayor cansancio en la cuidadora (OR: 1,31; IC 95%: 1,08-1,59), la presencia de dispositivos médicos en domicilio (OR: 1,69; IC 95%: 1,00-2,87) y recibían menos la intervención «Gestión de Casos».
ConclusionesLos pacientes que absorben la demanda de las enfermeras gestoras de casos presentan una alta complejidad, frente a la cual despliegan intervenciones conductuales, de navegación por el sistema sanitario y de seguridad clínica.
No health service can escape the huge epidemiological, care, social and economic challenge posed by chronic diseases. People with complex chronic disease processes are now the norm and no longer the exception, yet our health services have failed to adapt since their initial conception, which focussed on acute disease.1 The list of models to tackle this challenge is ever longer, but all studies agree on the development of self-care programmes, case management enhancement and strengthening primary care, together with the harmonisation of policies and strategies.2 Case management has become an essential ingredient3 due to the nature of this type of service, which contains fundamental elements for chronic care. It facilitates the accessibility and integration of multiple services guided by an assessment of the needs of highly complex, at-risk populations. It maximises continuity of care, and timely and prompt access to services and providers, establishes collaborative relationships proactively with other care team members, and helps patients and family carers to navigate their way through the labyrinth of decisions, providers and environments.4
Although it is a fairly widespread advanced nursing practice, the results of research into case management are fragmented, and contain some contraindications, such as the consequence of ambiguity of the role in many of the implementations made, the context-dependence of the services, and target patients and populations, and the selection and assessment methods, or its implementation in countries where primary care is poorly developed.4 Thus, we found results that indicate highly effective case management for people with dementia5 or chronic heart failure,6 and for family caregivers.7 But when the studies mix case management with other interventions, imprecisely define their target population, or assess a specific care aspect from a very limited perspective, the research results are rather unenlightening, leaving many gaps.8
Andalusia is one of the Spanish regions with a greater tradition in the development of case management, in a public system that cares for more than eight million citizens, and that has had more than 300 case managers for 15 years, most of whom in primary care. This advanced practice service has demonstrated its effectiveness in domiciliary care with improved access to the health services, coordination, improved functionality and satisfaction, and in reducing caregiver burden.9
Due to the extensive casuistry creating the demand for chronic care in the health services, it is not precisely known whether the most complex patients are being detected or whether those with fewer complex needs but a higher demand capacity are absorbing these services, resulting in reverse care due to the lower access or demand capacity of more vulnerable patients or those with socio-economic determinants.10 Furthermore, there is no precise information available on the outcomes achieved for patients who have been case managed under real clinical practice conditions, in terms of mortality, readmissions or certain adverse events, such as falls, pressure ulcers or drug-related problems.
The availability of electronic clinical histories does not provide sufficiently thorough information, especially due to methodological concerns as to the validity of the data, and monitoring of potentially confusing variables.11 A frequently used solution to this weakness has been to create registries of diseases or specific clinical situations. The registries can be population-based or clinical, and record information limited to cases attended in a specific institution, or in a network of centres, or from a notification system for a health problem.12 In these cases representativeness is not population-based, although their strength lies in the great value added by homogeneity in data collection.13 Registry-based research has great potential to cover health processes from a longitudinal perspective, and to obtain data under routine practice conditions.
In 2012 the RANGECOM registry was created throughout Andalusia to tackle many of these issues, standardising a body of variables that could be assessed longitudinally under real clinical practice conditions for chronic patients receiving case management services based in primary care, because this offers possibilities of longitudinality that are essential for appropriate patient follow-up.14 Since its initial years, there is sufficient volume and diversity of patients to establish the current case management situation. The objective of this study was to describe the essential characteristics of this advanced practice from the perspective of the population served, interventions deployed, usage and accessibility to services and mortality outcomes, hospital admissions, pressure ulcers, falls, drug-related problems and institutionalisation.
MethodsA longitudinal follow-up study was carried out of a cohort based on subjects introduced over the period 2013–2017. The study population comprised patients cared for in the case management service portfolio of Andalusian Healthcare Centres, and their main family caregivers. In order to be included in the registry the patients had to be beginner patients, over the age of 18, and have a reference caregiver. Subjects already included in the case management service portfolio (not beginners), and those who died before validation of their inclusion in the Registry, were excluded. The decision to include only de novo patients was to prevent potential information bias by including subjects who had been receiving the service over time, and whose outcomes and characteristics might not be comprehensively available.
Case management nurses (CMN) keep the registries of the different Andalusian health centres, coordinated by a provincial co-ordinator. Each case management nurse must apply to become a registrar. There is an online platform for the registry (www.range.com.es), which enables access with login and different profiles. A description of the features of the registry, its nature and type of variables are available in a previous publication.14 In sum, the registry currently has 102 standardised variables that collect data regarding the registrar, the features of the patients, their context and life conditions, interventions performed, services and providers that the patient has contacted, and events-outcomes-results that have occurred during follow-up. Each patient is monitored quarterly for any events (mortality, falls, pressure ulcers, drug-related problems, hospital readmissions, institutionalisation), contact with the various health providers, and interventions performed by the case management nurse during that period.
The data analysed correspond with the cut-off of the first quarterly follow-up of the complete sample.
AnalysisAn exploratory analysis of the data was carried out; obtaining measures of central tendency and dispersion or percentages. The normality of distribution of all the data was assessed using the Kolmogorov–Smirnov test, check of skewness, and histograms of the distributions.
A bivariate analysis was performed using the Student's t-test and Chi-square test according to the characteristics of the variables analysed, if they were normally distributed. Otherwise, non-parametric tests were used, such as Wilcoxon and Mann–Whitney U test. Similarly, the ANOVA was calculated for the relationship of quantitative and qualitative variables in the appropriate cases, with measures of central robustness in the case of non-homoscedasticity (checked with the Levene test) using the Welch and Brown-Forsythe test.
Multivariate logistical regression models were later completed to determine factors associated with certain events, such as hospital admissions and mortality. A discriminatory analysis was performed to determine service usage according to the types of patients, calculating the Wilks’ lambda statistic. All the analyses were completed using SPSS 23.
Ethical aspectsThe registry was authorised by the Provincial Research Ethics Committee of Malaga. The clinical data are kept separate from identifying data, and the databases are encrypted and safeguarded on servers protected by password access. All of the registries are made in compliance with the current data protection legislation. Before participating in the study, each patient was informed verbally and in writing of the objectives of the project and its methodology, and asked for their consent to be included in the Registry, or that of their representative if the patient was cognitively impaired.
ResultsThe study sample comprised 835 patients, included by a total of 157 registrars distributed throughout the eight provinces of Andalusia. The mean age of the patients was 76.8 years (SD: 12.1), and 50.24% were female. Of the patients, 87.5% had no education or had primary education, 85.3% had a family caregiver. Only 4.3% had an advance directive in place. The mean age of the caregivers was 50.8 years (SD: 34.2), 76.7% were female, with a mean of 21.8 months of caring (SD: 39.9). Of the caregivers, 75.4% had primary or secondary education, and 86.4% were the children or spouses of the patients. Eighty-six point four percent devoted more than 6h per day to caring tasks, and there was a paid caregiver in 23.4% of cases.
In terms of clinical features, 56.3% of the patients had diabetes, palliative care, dementia, multiple and oncological diseases, 26.6% were hospital discharges. The patients had high social support (Duke 41.1; SD: 10.2), although they had major comorbidity (Charlson 3.1; SD: 2.5), and a high level of dependence (Barthel 37.5; SD: 31.4); the caregiver burden assessed using the caregiver's effort index (IEC) was 6.5 (SD: 3.3).
With regard to the most frequent nursing diagnoses, risk for falls came first (20.9%), followed by ineffective denial (16.5%), and self-care deficit for feeding (14.5%).
With regard to the interventions deployed by case managers, 53 interventions were registered 6077 times, 18 of which constituted 75.1% of all the interventions undertaken, the first ten interventions included case management (70.5%), holistic assessment (87.2%) (not defined as an intervention under the Nursing Interventions Classification [NIC], but coded as another intervention in RANGECOM because it is a key component of the attributes of case management), main caregiver support (65.3%), counselling (45.9%), prevention of falls (42.4%), management of medication (41.2%), active listening (35.8%), referral (35%), environment-safety management (29.8%), and healthcare education (28.4%). Per NIC domain, 60.2% of the interventions were included under three domains: behavioural (26.0%), health system (20.2%), and safety (14.1%).
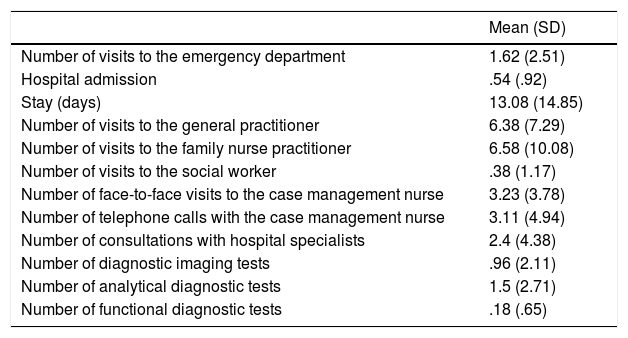
Accessibility to providers and service usage showed a usage profile that focussed on family practitioners and nurses, followed by face-to-face and telephone contact with the case manager and hospital specialists (Table 1). Over the period, 37.9% ended the case management service. A moderate significant correlation (p<.001) was found between the number of contacts with the CMN, and consultations with hospital specialists (r=.47), and with technical aids provided at home (r=.34).
Consultations with providers and services.
| Mean (SD) | |
|---|---|
| Number of visits to the emergency department | 1.62 (2.51) |
| Hospital admission | .54 (.92) |
| Stay (days) | 13.08 (14.85) |
| Number of visits to the general practitioner | 6.38 (7.29) |
| Number of visits to the family nurse practitioner | 6.58 (10.08) |
| Number of visits to the social worker | .38 (1.17) |
| Number of face-to-face visits to the case management nurse | 3.23 (3.78) |
| Number of telephone calls with the case management nurse | 3.11 (4.94) |
| Number of consultations with hospital specialists | 2.4 (4.38) |
| Number of diagnostic imaging tests | .96 (2.11) |
| Number of analytical diagnostic tests | 1.5 (2.71) |
| Number of functional diagnostic tests | .18 (.65) |
With regard to the outcomes evaluated in the RANGECOM registry, there was 34.4% mortality and 38.1% hospital admissions. There were 17.1% falls, 14.1% pressure ulcers, 5.5% had drug-related problems, and 4.9% were institutionalised.
The patients with a hospital admission had significantly more contact with family practitioners (p=.048) and family nurses (p=.004), more face-to-face (p=.011), and telephone contact (p<.001) with the case management nurse, with hospital specialists (p<.001), and more diagnostic and functional tests (p<.001).
Of the hospitalisations, 83.7% were urgent in nature, Internal Medicine was the department with the most admissions (45.5%). The subjects who were admitted had a mean stay of 13 days; 16.6% died in hospital.
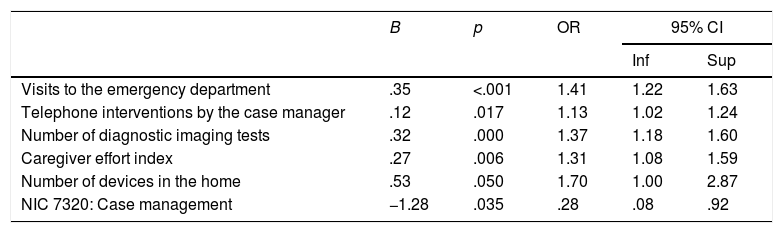
The multivariate analysis enabled identification of a model of good fit for a greater number of visits to the emergency department (OR: 1.41; 95%CI: 1.22–1.63), of telephone interventions by the CMN (OR: 1.12; 95%CI: 1.02–1.24), and performing imaging tests (OR: 1.37; 95%CI: 1.17–1.60), together with greater caregiver exhaustion (OR: 1.31; 95%CI: 1.08–1.59), the presence of medical devices in the home (OR: 1.69; 95%CI: 1.00–2.87), and receiving intervention 7320 “Case Management” less being associated with the occurrence of more than three readmissions (Table 2).
Multivariate analysis for multiple re-admissions to hospital (more than three).
| B | p | OR | 95% CI | ||
|---|---|---|---|---|---|
| Inf | Sup | ||||
| Visits to the emergency department | .35 | <.001 | 1.41 | 1.22 | 1.63 |
| Telephone interventions by the case manager | .12 | .017 | 1.13 | 1.02 | 1.24 |
| Number of diagnostic imaging tests | .32 | .000 | 1.37 | 1.18 | 1.60 |
| Caregiver effort index | .27 | .006 | 1.31 | 1.08 | 1.59 |
| Number of devices in the home | .53 | .050 | 1.70 | 1.00 | 2.87 |
| NIC 7320: Case management | −1.28 | .035 | .28 | .08 | .92 |
Correct classification: 96%; Hosmer–Lemeshow: .794.
Moreover, a multivariate model was constructed to determine factors associated with mortality, and found that the patients with poorer perceived social support, fewer technical aids and hospital admissions, and who ended case management had higher mortality, but the fit was not appropriate (Hosmer–Lemeshow p=.009) and was rejected.
DiscussionThis study sought to describe the characteristics of care provision to case-managed people with complex chronic diseases. The results leave no doubt that the patients who absorb the demand for this service are likely to be highly complex. Their comorbidities, levels of dependence and service usage profiles are highly complex, which is also reflected in the nursing diagnoses identified.
Furthermore, more than half the patients continued to be monitored by the case manager, which could be a further indicator of complexity, although it might also be due to inappropriate prolongation of the service by the case manager.
The profile of service usage and access made primary care the principal source of service provision, although high levels of hospital service usage were found, in terms of consultations with specialists, visits to the emergency department, and admissions.
From the perspective of increasing care complexity, the patients with multiple morbidity had high mortality,15 higher risk of falls16 and pressure ulcers,17 among some of the outcomes assessed in the registry. This also corroborates the complexity of the subjects cared for by the case management nurses.
Problems in accessibility to services for these patients have been described in the literature, due to the availability of these services or due to problems in their provision (discontinuity, needs left uncovered, rigidity in service organisation, etc.) which, on most occasions, involves the patient and those around them having to make an effort, become resigned to a system that does not meet their needs, using informal care for many uncovered demands, or having to make personal sacrifices.18 The data that this first analysis provides offer good hints that there is high accessibility of providers and services, which was also detected a decade ago when case management in the Andalusian system was assessed,9 and which has been regularly reported in studies on case management.5 Other questions are whether or not this usage is appropriate, which is not currently assessed on the registry, and whether these services might be being used to replace other needs that are not being met, and finally, whether there are public health service users who are left under the radar of case management. The latter does not appear to be the case, in that most patients are grouped under simultaneous chronic diseases. Nonetheless, much research is yet to be done on the systems for identifying and classifying patients who are candidates for case management.19 This is a line where the RANGECOM registry can provide many research possibilities in the future.
Another question that always arises regarding the analysis of advanced practice services is the controversial distribution of the ingredients and components of interventions. In the case of case management this is a widely debated aspect,4 in the RANGECOM registry the NIC interventions were included as a standardised way of approaching this issue, due to the demonstrated capacity of this classification for this purpose.20 In this regard, the distribution of registered NIC interventions correspond with the characteristic attributes of case management described in the literature, especially the behavioural interventions, those for help in decision-making, and those for navigation through the health system, also highlighting the major commitment of interventions to clinical safety, an unavoidable aspect bearing mind the increased risk of adverse events for this population.21 The NIC domains that we found are similar to those described in a previous study on a population with the same features.22
These findings are positive regarding the description of active ingredients in case management provision for multimorbid patients; for example, the identification of case management in the multivariate model of frequent readmissions as an independent predictor of the NIC. Nevertheless, progress needs to be made in identifying the “optimal doses”, and in analysing possible patterns of variability between professionals, centres, provinces, etc. These aspects could be covered by the RANGECOM registry, and will be the subject of analysis in future studies.
However, an in-depth examination of the magnitude of the power of associations found is necessary, and corroboration of the time sequence between factors and outcomes, as well as an exploration of possible gradients of exposure-response between them. Furthermore, confirmation of the consistency of the previous results in a wider sample size with longer follow-up periods is mandatory, to examine the prediction of events.
It is also necessary to look into the levels of variability in the interventions and services deployed in isogroups of patients adjusted by age, sex, functionality and clinical profile, at different levels of aggregation.
Registry-based research has great potential for the understanding of health processes from a longitudinal perspective, and for obtaining data in routine practice conditions. Registries enable the characteristics of providers to be linked with the decisions they make, and to the results that are produced in care,23 making comparisons possible between different practice environments. Registries have been criticised for their possible lack of control over potentially confusing variables and missing data. However, these are common limitations of any non-randomised or observational study,24 and the long tradition of their contribution to cancer,25 heart failure,26 and mental health,27 and much more, indicate that this resource is an invaluable source of data for studying case management.
FinancingThis study was financed by the Health Council of the Andalusian Regional Government (PI 0268/2012).
Conflict of interestsThe authors have no conflict of interests to declare.
The authors would like to thank all the case management nurses who participated in the RANGECOM Registry for their collaboration and commitment.
Please cite this article as: Morales-Asencio JM, Cuevas-Fernández-Gallego M, Morilla-Herrera JC, Martín-Santos FJ, Silvano Arranz A, Batres Sicilia JP, et al. Características de la provisión del servicio de gestión de casos en el entorno comunitario en Andalucía a partir del registro RANGECOM. Enferm Clin. 2019. https://doi.org/10.1016/j.enfcli.2018.12.009