The COVID-19 pandemic disrupted healthcare services usage. We estimated the impact of the COVID-19 pandemic on healthcare services utilization among people living with HIV (PLWH) in Catalonia, Spain.
MethodsWe accessed public healthcare usage in HIV units, primary care, hospitals, and emergency departments among 17,738 PLWH in the PISCIS cohort from January 1, 2017, to December 31, 2020. We performed an interrupted time series analysis using the autoregressive integrated moving average to estimate the effect of COVID-19 on medical visits and HIV monitoring among PLWH.
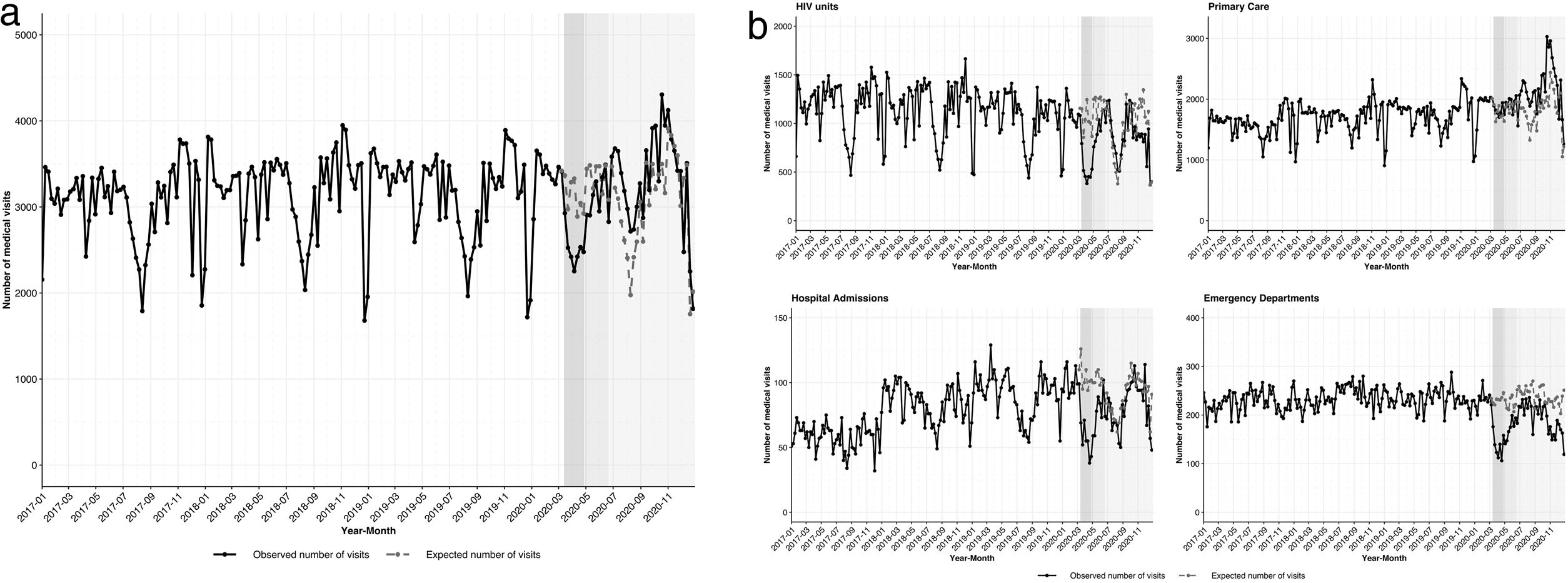
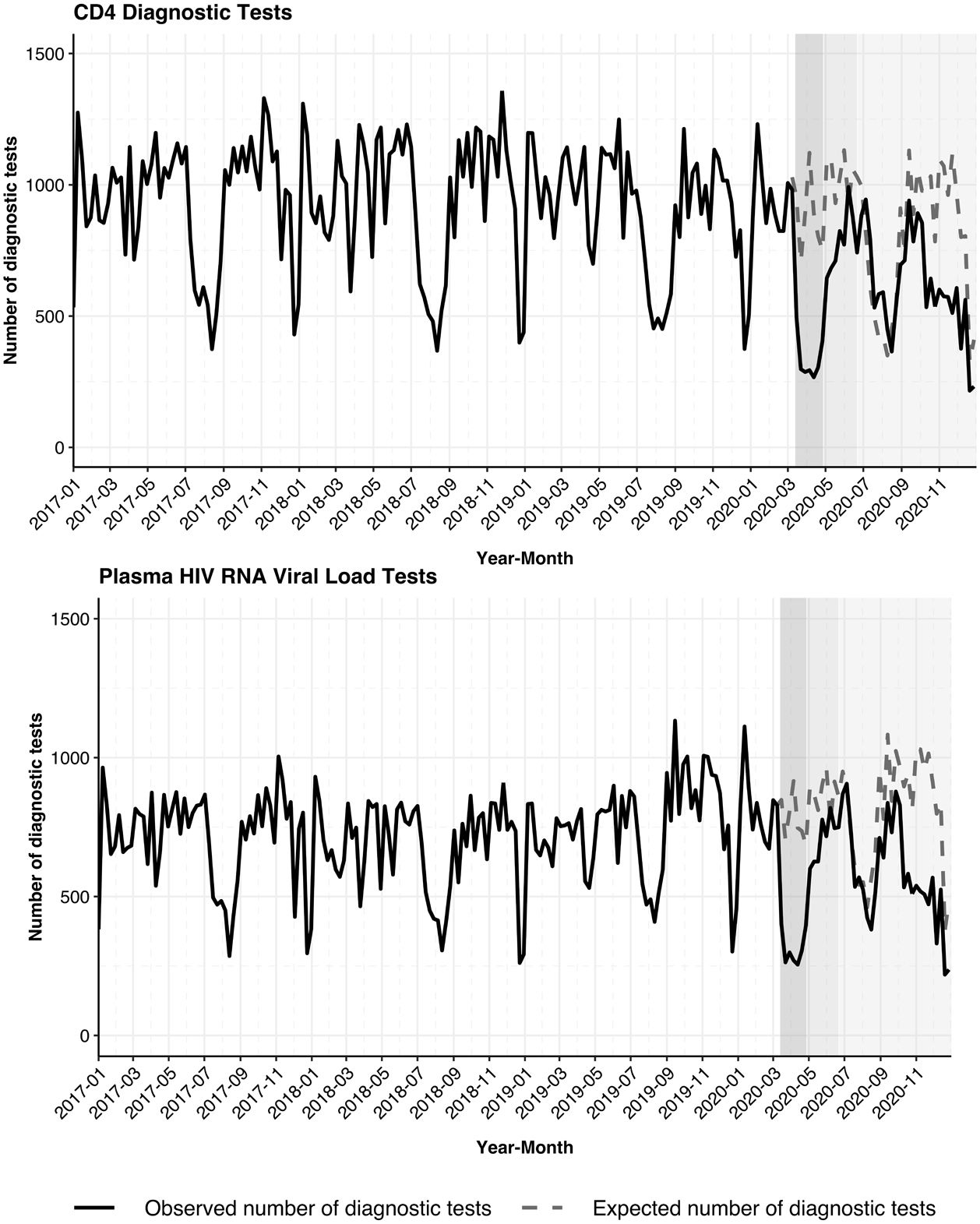
ResultsA non-significant decrease of 17.1% (95% CI: [−29.4, 0.4]) in overall medical visits was observed during the lockdown, followed by a steady resumption until the end of 2020. Three health facilities presented statistically significant declines in visits during the lockdown: HIV units (−44.8% [−56.7, −23.6]), hospitals (−40.4% [−52.8, −18.1]), and emergency departments (−36.9% [−47.0, −21.9]); thereafter, the visits have begun to increase steadily but not to previous levels as of December 2020. In contrast, primary care visits remained unchanged during the lockdown by 1.9% (95% CI: −13.5, 23.9). CD4 cell (54.2% [95% CI: −64.4, −36.0]) and HIV RNA viral load (53.1% [95% CI: −62.9, −36.1]) laboratory monitoring reduced significantly during the lockdown.
ConclusionCOVID-19 lockdowns significantly disrupted in-person healthcare services usage among PLWH. The reduction in healthcare utilization however did not affect primary care services. Despite services gradually rebounding to pre-pandemic levels, it is imperative to effectively prepare for future pandemics and implement measures to ensure continuous provision of care to PLWH during pandemic lockdowns.
La pandemia de COVID-19 interrumpió el uso de los servicios sanitarios. Estimamos el impacto de la pandemia de COVID-19 en la utilización de los servicios de salud entre las personas que viven con el VIH (PVV) en Cataluña, España.
MétodosRegistramos el uso de la atención médica pública en unidades de VIH, atención primaria, hospitales y centros de urgencias en 17.738PVV de la cohorte PISCIS desde el 1 de enero de 2017 hasta el 31 de diciembre de 2020. Realizamos un análisis de series temporales interrumpidas utilizando el promedio móvil integrado autorregresivo para estimar el efecto de la COVID-19 en las consultas médicas y el seguimiento del VIH entre las PVV.
ResultadosSe observó una disminución no significativa del 17,1% (IC95%: −29,4 a 0,4) en las visitas médicas generales durante el confinamiento, seguida de una reanudación constante hasta finales de 2020. Tres establecimientos de salud presentaron disminuciones estadísticamente significativas en las visitas durante el confinamiento: unidades de VIH (−44,8% [−56,7 a −23,6]), hospitales (−40,4% [−52,8 a −18,1]) y urgencias (−36,9% [−47,0 a −21,9]); a partir de entonces, las visitas han comenzado a aumentar de manera constante, pero no a los niveles anteriores a diciembre de 2020. Por el contrario, las visitas de atención primaria se mantuvieron sin cambios durante el confinamiento en un 1,9% (ICIC 95%: −13,5 a 23,9). El control de las analíticas de células CD4 (54,2% [IC95%: −64,4 a −36,0]) y de la carga viral de ARN del VIH (53,1% [IC95%: −62,9 a −36,1]) se redujo significativamente durante el confinamiento.
ConclusiónLos bloqueos de COVID-19 interrumpieron significativamente el uso de servicios de atención médica en persona entre las PVV. Sin embargo, la reducción en la utilización de la atención sanitaria no afectó a los servicios de atención primaria. A pesar de que los servicios se recuperan gradualmente a los niveles previos a la pandemia, es imperativo prepararse de manera efectiva para futuras pandemias e implementar medidas para garantizar la provisión continua de atención a las PVV durante los bloqueos por pandemia.
Since the emergence of the novel Coronavirus Disease 2019 (COVID-19) pandemic, governments across the globe implemented several response strategies to limit its transmission and maintain the accessibility and quality of healthcare services. The critical policy responses to COVID-19 included the closure of non-essential businesses and physical contact restrictions, such as curfews and lockdowns in the early phase of the pandemic. Lockdown proved effective in reducing community transmissions of the virus.1 However, it led to an unintentional diminution in the accessibility of healthcare services.2
According to the World Health Organization (WHO), over 90% of countries reported ongoing disruptions in primary care, emergency care, hospital access, and essential health services, such as HIV care, over one year into the COVID-19 pandemic.3,4 Besides, different studies have revealed significant disruptions in the HIV care continuum.5,6 A survey from Central and Eastern Europe reported that only 31.6% of HIV clinics were operating normally.7
In Spain, the government announced a countrywide lockdown on March 13, 2020, with strict stay-at-home measures.8 A study in Barcelona, Spain, found a 25% reduction in outpatient visits in people living with HIV (PLWH), a 45% reduction in post-exposure prophylaxis visits, and a 12% reduction in hospital admissions in 2020 compared to 2019.9 Approximately 160,000 people were living with HIV in Spain as of the end of 2021 and 3900 new infections were reported in the same year.10 With a significant burden of underlying comorbidities and pre-existing health inequalities among PLWH, there were concerns that PLWH were more susceptible to COVID-19 infection and poor clinical outcomes in the early phases of the outbreak.11 Particularly, some sub-populations including those with advanced immunodeficiency, chronic co-morbidities, and migrants were vulnerable to severe COVID-19.12 Compared to the general population, PLWH have high rates of health service use because of the higher prevalence of other medical conditions in this population and hence the importance of maintaining engagement with the healthcare system.13
Information on the impact of the COVID-19 pandemic on health service utilization among PLWH specifically is scanty. In this study, we estimated the magnitude of the effect of COVID-19 on public healthcare services usage in four types of facilities; HIV units, primary care, hospitals, and emergency departments, among PLWH in Catalonia, Spain. Additionally, we investigated the impact of the pandemic on CD4 cell count and HIV RNA viral load monitoring.
MethodsStudy design and populationWe conducted a population-based retrospective study using data from the PISCIS cohort in Catalonia, Spain, between January 1, 2017, and December 31, 2020. The PISCIS cohort is described in detail elsewhere.14 Briefly, PISCIS is a multicentre and population-based cohort of PLWH aged ≥16 years in care at 16 participating hospitals in Catalonia. The cohort has collected sociodemographic and clinico-epidemiological data since 1998 and is estimated to represent approximately 84% of PLWH in Catalonia.
We linked PISCIS data with the Public Data Analysis for Health Research and Innovation Program of Catalonia (PADRIS) to access data on public healthcare usage. PADRIS is a longitudinal and quality-controlled information system that periodically collects individual-level information from Catalan residents on demographic, socioeconomic characteristics, health-related and medical data, and public healthcare usage, including laboratory tests, pharmacy prescription fillings, and primary, outpatient, inpatient, and emergency department visits.15 In Catalonia, residents have the right to access free public healthcare regardless of their immigration status.16
The PISCIS cohort study has been approved by the Ethics Committee of the Germans Trias i Pujol University Hospital, Badalona, Spain (EO-11-108). Data collection has also been approved by the ethics committees of participating hospitals. Patient-level information obtained from PADRIS was anonymized and deidentified before the analysis. The planning, conduct, and reporting of the study were in line with the Declaration of Helsinki, as revised in 2013.
ProceduresThe weekly health services utilization from HIV units, primary care, hospitals, and emergency departments was assessed among PLWH in our cohort from January 1, 2017, to December 31, 2020. The study periods were categorized as follows: pre-lockdown (before March 13, 2020), lockdown (March 13 to April 27, 2020), de-escalation phase (April 28 to June 21, 2020), and the new normality (since June 22, 2020).17
Primary care visits were defined as all visits to the primary care centres (CAPs) in Catalonia, Spain. All teleconsultations are also recorded as primary care visits in the database of the Catalan Health Institute (ICS). Hospital visits are outpatient and inpatient visits to the hospital excluding visits to the HIV units. HIV unit visits are outpatient visits to the HIV unit excluding HIV-related hospitalizations. Visits to the emergency departments include all visits to the emergency unit.
We included the data on sociodemographic information (age, sex assigned at birth, country of origin, socioeconomic deprivation, HIV transmission groups, CD4 cell counts, plasma HIV viral loads (detectable and undetectable), chronic comorbidities, and antiretroviral therapy (ART) records. Undetectable HIV viral load was defined as values lower than 50 copies of HIV RNA per mL. The International Classification of Diseases (ICD) codes were used to extract the most prevalent chronic comorbidities. Socioeconomic deprivation was divided into three levels according to the socio-economic index of the Government of Catalonia, which includes five indicators: the proportion of manual workers, the proportion of residents with low education levels, the proportion with low income, the rate of premature mortality, and the rate of avoidable hospitalization according to the basic health area of residence in Catalonia. The first tertile represents the highest socioeconomic level (least deprived), while the third tertile represents the lowest level (most deprived).
Statistical analysisCategorical variables were presented in counts and percentages, while continuous variables were presented in medians and interquartile ranges (IQR). We compared normally distributed continuous data using Student's t-tests, whereas Mann–Whitney U test was used for non-normally distributed data. χ2 and fisher's exact tests were used to examine the differences between categorical variables as appropriate.
We evaluated the impact of the COVID-19 pandemic on healthcare services utilization using the autoregressive integrated moving average (ARIMA) model. This approach was selected for this study considering the underlying trends, autocorrelation, and seasonality in our data. Between January 1, 2017, to December 31, 2020, we observed 209 weeks of visits, and the date of the lockdown (March 13, 2020) was used as a change point in the model. Weekly medical visits were modelled to forecast the expected number of medical visits with their 95% confidence intervals (95% CIs) in the absence of the lockdown across study periods based on the three years of historical data. We calculated the percentage changes between the observed and expected visits in each period. Same approach was used to analyze the frequency of CD4 and plasma HIV RNA viral load laboratory monitoring. All analyses were done with R (version 4.1.2).
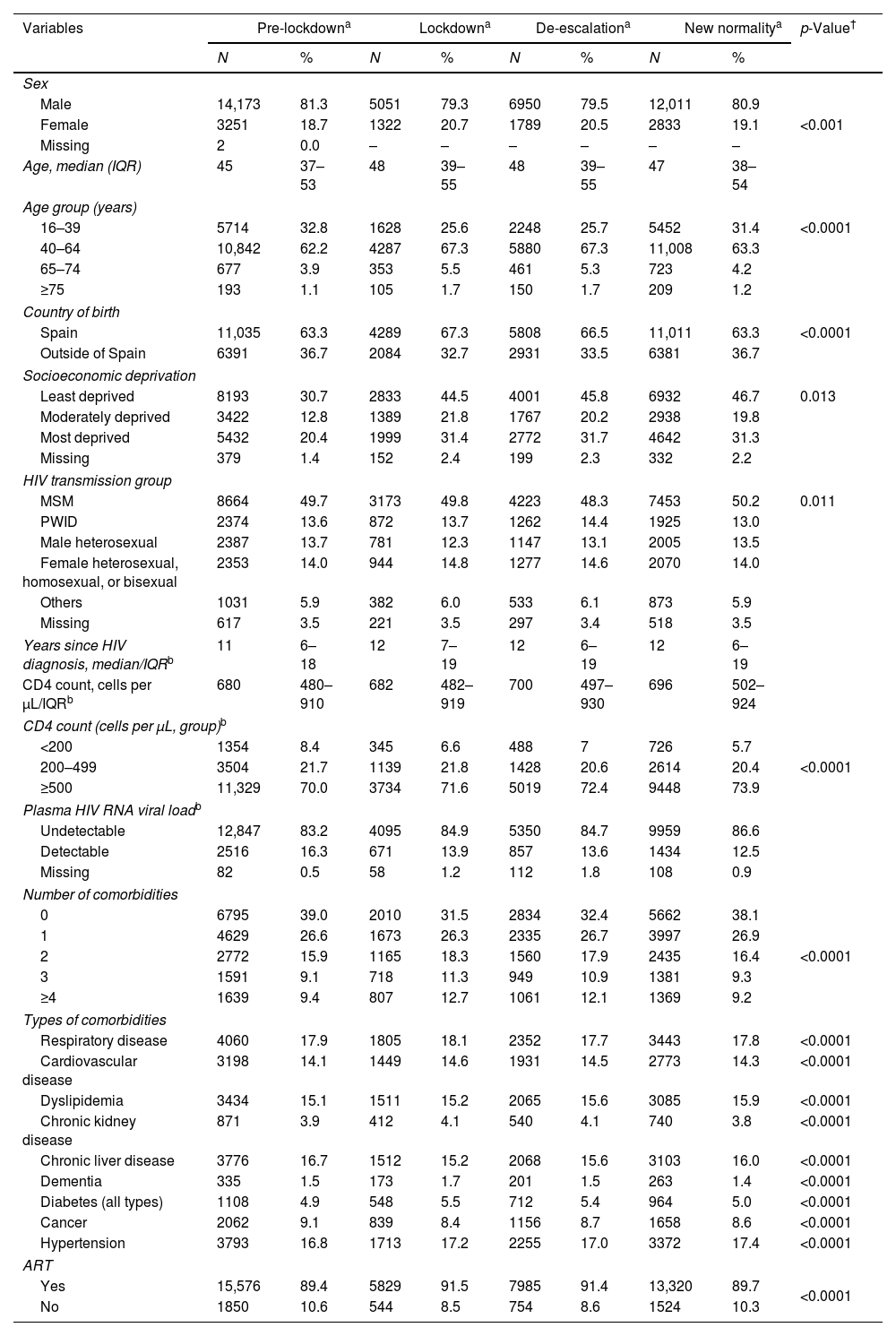
ResultsCharacteristics of the study population and visits during the study periodDuring the study period, the 17,639 PLWH in our cohort made 656,135 visits to healthcare facilities. At baseline, the majority of participants were males (81.4%), with a median age of 45.0 years (IQR: 37.0–52.0). Migrants represented 37.3% of the study cohort, and 47.1% belonged to a high socioeconomic class. The median time since HIV diagnosis among the population was 12 (IQR 6.0–19.0) years. The main reported HIV transmission group was MSM (49.8%). Seventy percent of participants had a CD4 count greater than 500cells per μL, and 83.2% had an HIV-RNA <50copies/mL (Table 1). At baseline, 60.2% had chronic comorbidities. Regarding treatment, 89.4% of patients were receiving ART during the pre-lockdown period, followed by 91.5%, 91.4%, and 89.7% during the lockdown, de-escalation, and new normality, respectively (Table 1).
Baseline characteristics of people living with HIV in Catalonia during the different study periods, 2017–2020.
| Variables | Pre-lockdowna | Lockdowna | De-escalationa | New normalitya | p-Value† | ||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | ||
| Sex | |||||||||
| Male | 14,173 | 81.3 | 5051 | 79.3 | 6950 | 79.5 | 12,011 | 80.9 | <0.001 |
| Female | 3251 | 18.7 | 1322 | 20.7 | 1789 | 20.5 | 2833 | 19.1 | |
| Missing | 2 | 0.0 | – | – | – | – | – | – | |
| Age, median (IQR) | 45 | 37–53 | 48 | 39–55 | 48 | 39–55 | 47 | 38–54 | |
| Age group (years) | |||||||||
| 16–39 | 5714 | 32.8 | 1628 | 25.6 | 2248 | 25.7 | 5452 | 31.4 | <0.0001 |
| 40–64 | 10,842 | 62.2 | 4287 | 67.3 | 5880 | 67.3 | 11,008 | 63.3 | |
| 65–74 | 677 | 3.9 | 353 | 5.5 | 461 | 5.3 | 723 | 4.2 | |
| ≥75 | 193 | 1.1 | 105 | 1.7 | 150 | 1.7 | 209 | 1.2 | |
| Country of birth | |||||||||
| Spain | 11,035 | 63.3 | 4289 | 67.3 | 5808 | 66.5 | 11,011 | 63.3 | <0.0001 |
| Outside of Spain | 6391 | 36.7 | 2084 | 32.7 | 2931 | 33.5 | 6381 | 36.7 | |
| Socioeconomic deprivation | |||||||||
| Least deprived | 8193 | 30.7 | 2833 | 44.5 | 4001 | 45.8 | 6932 | 46.7 | 0.013 |
| Moderately deprived | 3422 | 12.8 | 1389 | 21.8 | 1767 | 20.2 | 2938 | 19.8 | |
| Most deprived | 5432 | 20.4 | 1999 | 31.4 | 2772 | 31.7 | 4642 | 31.3 | |
| Missing | 379 | 1.4 | 152 | 2.4 | 199 | 2.3 | 332 | 2.2 | |
| HIV transmission group | |||||||||
| MSM | 8664 | 49.7 | 3173 | 49.8 | 4223 | 48.3 | 7453 | 50.2 | 0.011 |
| PWID | 2374 | 13.6 | 872 | 13.7 | 1262 | 14.4 | 1925 | 13.0 | |
| Male heterosexual | 2387 | 13.7 | 781 | 12.3 | 1147 | 13.1 | 2005 | 13.5 | |
| Female heterosexual, homosexual, or bisexual | 2353 | 14.0 | 944 | 14.8 | 1277 | 14.6 | 2070 | 14.0 | |
| Others | 1031 | 5.9 | 382 | 6.0 | 533 | 6.1 | 873 | 5.9 | |
| Missing | 617 | 3.5 | 221 | 3.5 | 297 | 3.4 | 518 | 3.5 | |
| Years since HIV diagnosis, median/IQRb | 11 | 6–18 | 12 | 7–19 | 12 | 6–19 | 12 | 6–19 | |
| CD4 count, cells per μL/IQRb | 680 | 480–910 | 682 | 482–919 | 700 | 497–930 | 696 | 502–924 | |
| CD4 count (cells per μL, group)b | |||||||||
| <200 | 1354 | 8.4 | 345 | 6.6 | 488 | 7 | 726 | 5.7 | <0.0001 |
| 200–499 | 3504 | 21.7 | 1139 | 21.8 | 1428 | 20.6 | 2614 | 20.4 | |
| ≥500 | 11,329 | 70.0 | 3734 | 71.6 | 5019 | 72.4 | 9448 | 73.9 | |
| Plasma HIV RNA viral loadb | |||||||||
| Undetectable | 12,847 | 83.2 | 4095 | 84.9 | 5350 | 84.7 | 9959 | 86.6 | |
| Detectable | 2516 | 16.3 | 671 | 13.9 | 857 | 13.6 | 1434 | 12.5 | |
| Missing | 82 | 0.5 | 58 | 1.2 | 112 | 1.8 | 108 | 0.9 | |
| Number of comorbidities | |||||||||
| 0 | 6795 | 39.0 | 2010 | 31.5 | 2834 | 32.4 | 5662 | 38.1 | <0.0001 |
| 1 | 4629 | 26.6 | 1673 | 26.3 | 2335 | 26.7 | 3997 | 26.9 | |
| 2 | 2772 | 15.9 | 1165 | 18.3 | 1560 | 17.9 | 2435 | 16.4 | |
| 3 | 1591 | 9.1 | 718 | 11.3 | 949 | 10.9 | 1381 | 9.3 | |
| ≥4 | 1639 | 9.4 | 807 | 12.7 | 1061 | 12.1 | 1369 | 9.2 | |
| Types of comorbidities | |||||||||
| Respiratory disease | 4060 | 17.9 | 1805 | 18.1 | 2352 | 17.7 | 3443 | 17.8 | <0.0001 |
| Cardiovascular disease | 3198 | 14.1 | 1449 | 14.6 | 1931 | 14.5 | 2773 | 14.3 | <0.0001 |
| Dyslipidemia | 3434 | 15.1 | 1511 | 15.2 | 2065 | 15.6 | 3085 | 15.9 | <0.0001 |
| Chronic kidney disease | 871 | 3.9 | 412 | 4.1 | 540 | 4.1 | 740 | 3.8 | <0.0001 |
| Chronic liver disease | 3776 | 16.7 | 1512 | 15.2 | 2068 | 15.6 | 3103 | 16.0 | <0.0001 |
| Dementia | 335 | 1.5 | 173 | 1.7 | 201 | 1.5 | 263 | 1.4 | <0.0001 |
| Diabetes (all types) | 1108 | 4.9 | 548 | 5.5 | 712 | 5.4 | 964 | 5.0 | <0.0001 |
| Cancer | 2062 | 9.1 | 839 | 8.4 | 1156 | 8.7 | 1658 | 8.6 | <0.0001 |
| Hypertension | 3793 | 16.8 | 1713 | 17.2 | 2255 | 17.0 | 3372 | 17.4 | <0.0001 |
| ART | |||||||||
| Yes | 15,576 | 89.4 | 5829 | 91.5 | 7985 | 91.4 | 13,320 | 89.7 | <0.0001 |
| No | 1850 | 10.6 | 544 | 8.5 | 754 | 8.6 | 1524 | 10.3 | |
Abbreviations: ART, antiretroviral therapy; IQR, interquartile range; MSM, men who have sex with men; PLWH, people living with HIV; PWID, people who inject drugs.
The study time periods are defined as pre-lockdown (before March 13, 2020), during lockdown (March 13 to April 27, 2020), during de-escalation phases (April 28 to June 21, 2020), and during the new normality (since June 22, 2020).
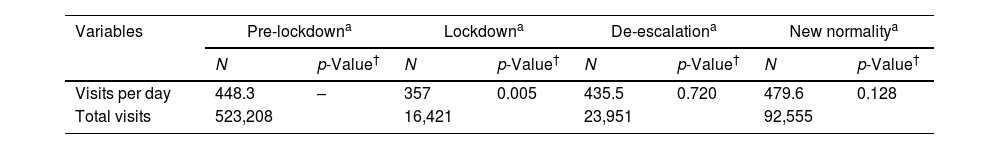
Among 656,135 visits to healthcare facilities, 56.4% (370,116) were in primary care, followed by 34.0% (223,230) in the HIV units, 7.0% (46,390) at the emergency department, and 2.5% (16,399) were hospital admissions. In the cohort, PLWH made an average of 448.3 visits daily before the lockdown, 357.0 visits per day during the lockdown, 435.5 visits per day in the de-escalation phase, and 479.6 visits per day in the new normality. Over the course of four years, the average visits to HIV units per PLWH showed a slightly declining trend, dropping from 4.32 visits in 2017 to 3.23 visits in 2020. Conversely, in primary healthcare settings, a contrasting trend emerged. The mean visits per PLWH displayed consistent growth, rising from 6.59 visits in 2017 to 8.16 visits in 2020. Hospital admissions and emergency department visits demonstrated relative stability in the annual average visits. The mean hospital admissions per PLWH ranged from 1.47 to 1.80, while for the emergency departments, the average visits ranged from 2.07 to 2.18 (Suppl. Table 2). For the predefined study periods, visits to primary health care remained the highest among all other health facilities in each study periods, reaching 71.7% of total visits during the lockdown (Table 2).
Number of visits among people living with HIV in Catalonia in health facilities during four study periods, 2017–2020.
| Variables | Pre-lockdowna | Lockdowna | De-escalationa | New normalitya | ||||
|---|---|---|---|---|---|---|---|---|
| N | p-Value† | N | p-Value† | N | p-Value† | N | p-Value† | |
| Visits per day | 448.3 | – | 357 | 0.005 | 435.5 | 0.720 | 479.6 | 0.128 |
| Total visits | 523,208 | 16,421 | 23,951 | 92,555 | ||||
| N | % | N | % | N | % | N | % | |
|---|---|---|---|---|---|---|---|---|
| HIV units | 188,713 | 36.1 | 3379 | 20.6 | 7103 | 29.7 | 24,035 | 26.0 |
| Primary care | 282,563 | 54.0 | 11,771 | 71.7 | 14,929 | 62.3 | 60,853 | 65.8 |
| Hospital admissions | 13,182 | 2.5 | 367 | 2.2 | 585 | 2.4 | 2265 | 2.5 |
| Emergency department | 38,750 | 7.4 | 904 | 5.5 | 1334 | 5.6 | 5402 | 5.8 |
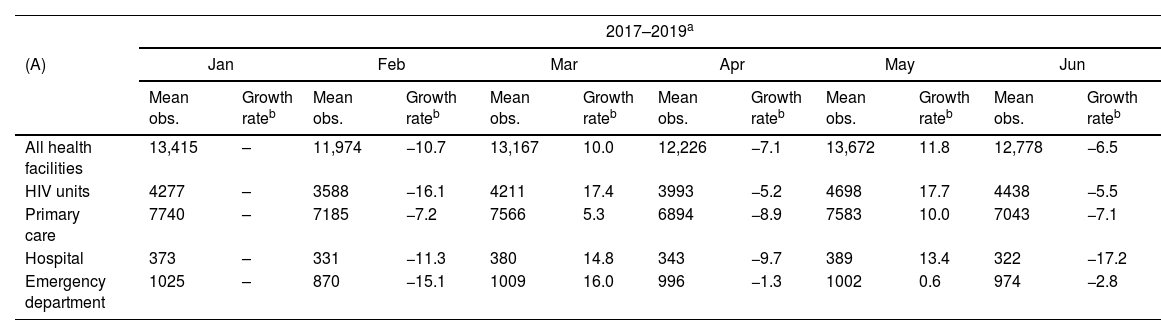
The monthly medical visits exhibited a distinct seasonal pattern of decreased visits in February, April, August, November, and December every year between 2017 and 2020. A drastic decline in overall medical visits occurred in April 2020 compared to the previous month, with a 17.3% reduction, while a 7.1% reduction was observed during the same period from 2017 to 2019. We found a sharp decline in in-person visits in HIV units with a 42.7% reduction (−5.2 in 2017–2019), followed by a 39.4% reduction in hospital admissions (−9.7 in 2017–2019), a 33.3% reduction in emergency departments (−1.3 in 2017–2019), and a 4.8% reduction in primary health care (−8.9 in 2017–2019) (Table 3).
Comparison of the average number of monthly visits among PLWH in Catalonia from 2017 to 2019 to visits in 2020 stratified by health facility types. (A) Number of monthly medical visits from January to June and (B) number of monthly medical visits from July to December.
| 2017–2019a | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (A) | Jan | Feb | Mar | Apr | May | Jun | ||||||
| Mean obs. | Growth rateb | Mean obs. | Growth rateb | Mean obs. | Growth rateb | Mean obs. | Growth rateb | Mean obs. | Growth rateb | Mean obs. | Growth rateb | |
| All health facilities | 13,415 | – | 11,974 | −10.7 | 13,167 | 10.0 | 12,226 | −7.1 | 13,672 | 11.8 | 12,778 | −6.5 |
| HIV units | 4277 | – | 3588 | −16.1 | 4211 | 17.4 | 3993 | −5.2 | 4698 | 17.7 | 4438 | −5.5 |
| Primary care | 7740 | – | 7185 | −7.2 | 7566 | 5.3 | 6894 | −8.9 | 7583 | 10.0 | 7043 | −7.1 |
| Hospital | 373 | – | 331 | −11.3 | 380 | 14.8 | 343 | −9.7 | 389 | 13.4 | 322 | −17.2 |
| Emergency department | 1025 | – | 870 | −15.1 | 1009 | 16.0 | 996 | −1.3 | 1002 | 0.6 | 974 | −2.8 |
| 2020 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (A) | Jan | Feb | Mar | Apr | May | Jun | ||||||
| Obs. | Growth rateb | Obs. | Growth rateb | Obs. | Growth rateb | Obs. | Growth rateb | Obs. | Growth rateb | Obs. | Growth rateb | |
| All health facilities | 13,226 | 16.6 | 12,446 | −5.9 | 12,463 | 0.1 | 10,311 | −17.3 | 11,507 | 11.6 | 12,571 | 9.2 |
| HIV units | 4281 | 27.0 | 3553 | −17.0 | 3226 | −9.2 | 1848 | −42.7 | 2968 | 60.6 | 3755 | 26.5 |
| Primary care | 8037 | 20.6 | 7965 | −0.9 | 8484 | 6.5 | 8077 | −4.8 | 7987 | −1.1 | 8142 | 1.9 |
| Hospital | 458 | 49.2 | 400 | −12.7 | 358 | −10.5 | 217 | −39.4 | 292 | 34.6 | 358 | 22.6 |
| Emergency department | 1005 | 0.9 | 990 | −1.5 | 829 | −16.3 | 553 | −33.3 | 682 | 23.3 | 827 | 21.3 |
| 2017–2019a | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (B) | Jul | Aug | Sep | Oct | Nov | Dec | ||||||
| Mean obs. | Growth rateb | Mean obs. | Growth rateb | Mean obs. | Growth rateb | Mean obs. | Growth rateb | Mean obs. | Growth rateb | Mean obs. | Growth rateb | |
| All health facilities | 12,856 | 0.6 | 10,018 | −22.1 | 11,797 | 17.8 | 14,430 | 22.3 | 14,293 | −0.9 | 11,339 | −20.7 |
| HIV units | 4025 | −9.3 | 2389 | −40.6 | 3839 | 60.7 | 4712 | 22.7 | 4605 | −2.3 | 3372 | −26.8 |
| Primary care | 7432 | 5.5 | 6250 | −15.9 | 6640 | 6.2 | 8255 | 24.3 | 8399 | 1.7 | 6664 | −20.7 |
| Hospital | 302 | −6.2 | 252 | −16.6 | 307 | 21.8 | 400 | 30.3 | 342 | −14.5 | 307 | −10.2 |
| Emergency department | 1097 | 12.6 | 1127 | 2.7 | 1012 | −10.2 | 1063 | 5.0 | 947 | −10.9 | 996 | 5.2 |
| 2020 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (B) | Jul | Aug | Sep | Oct | Nov | Dec | ||||||
| Obs. | Growth rateb | Obs. | Growth rateb | Obs. | Growth rateb | Obs. | Growth rateb | Obs. | Growth rateb | Obs. | Growth rateb | |
| All health facilities | 14,859 | 18.2 | 11,468 | −22.8 | 13,422 | 17.0 | 16,066 | 19.7 | 15,257 | −5.0 | 12,386 | −18.8 |
| HIV units | 4057 | 8.0 | 2240 | −44.8 | 3625 | 61.8 | 3873 | 6.8 | 3604 | −6.9 | 3009 | −16.5 |
| Primary care | 9998 | 22.8 | 8473 | −15.3 | 8971 | 5.9 | 11,383 | 26.9 | 11,005 | −3.3 | 8644 | −21.5 |
| Hospital | 349 | −2.5 | 262 | −24.9 | 369 | 40.8 | 453 | 22.8 | 395 | −12.8 | 341 | −13.7 |
| Emergency department | 981 | 18.6 | 913 | −6.9 | 919 | 0.7 | 879 | −4.4 | 681 | −22.5 | 775 | 13.8 |
Abbreviations: Obs., observations.
Notes: Visits during the lockdown period were displayed in bold type.
Regarding overall medical visits, we observed a non-significant decrease of 17.1% (95% CI: −29.4, 0.4) during the lockdown period. This was followed by a slight decline of 8.0% (95% CI: [−21.4, 10.8]) during the de-escalation period; and a subsequent increase of 8.6% (95% CI: [−8.8, 34.2]) during the new normality phase (Fig. 1a). These changes were however not significant.
Weekly (a) overall health facility visits, (b) visits by health facility types of people living with HIV in Catalonia, 2017–2020. Notes: the solid line shows the actual visits from January 2017 to December 2020, and the dashed line represents the expected number of visits predicted by the ARIMA model from March to December 2020.
In terms of the different healthcare facilities, the number of visits in HIV units, hospitals, and emergency departments significantly declined during the lockdown (HIV units: −44.8%, [−56.7, −23.6]; hospitals: −40.4%, [−52.8, −18.1]; emergency departments: −36.9%, [−47.0, −21.9]). Visits to these units appear to be gradually restoring since the complete lift on lockdown measures (HIV units: −7.9% [−30.6, 36.6]; hospitals: −9.3%, [−34.9, 49.4]; emergency units −19.6% [−32.8, 0.1]). Visits to primary care have remained relatively unchanged (Fig. 1b).
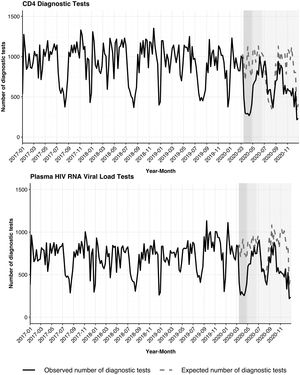
For laboratory tests, we observed reductions in CD4 cell count and plasma HIV RNA viral load laboratory monitoring, showing a statistically significant decrease of 54.2% (95% CI: [−64.4, −36.0]) and 53.1% (95% CI: [−62.9, −36.1]) during the lockdown, respectively. Both tests resumed after the lockdown period; however, none of them had returned to the pre-pandemic levels as of the end of 2020 (Fig. 2).
Weekly numbers of (a) CD4 cell counts, (b) plasma HIV RNA viral load laboratory tests among people living with HIV in Catalonia, 2017–2020. Notes: the solid line shows the actual visits from January 2017 to December 2020, and the dashed line represents the expected number of visits predicted by the ARIMA model from March to December 2020.
This study evaluated how the COVID-19 pandemic affected healthcare services utilization among PLWH in Catalonia, Spain. Following the lockdown announcement, a non-significant decrease of 17.1% (95% CI: [−29.4, 0.4]) in overall medical visits were followed by a steady resumption until the end of 2020. HIV units, hospital admissions, and emergency departments presented statistically significant declines in visits during the lockdown. Thereafter, the visits have begun to increase steadily but have not returned to previous levels. In contrast, primary care visits remained unchanged during the lockdown. Importantly, for HIV laboratory monitoring, we observed significant reductions in CD4 cells and plasma HIV RNA viral load testing. Both tests resumed after the lockdown period; however, none of them returned to pre-pandemic levels as of the end of 2020.
Multiple reasons may contribute to the dramatic decrease in visits during the lockdown among PLWH in our study. Generally, the unprecedented mobility restrictions have unintentionally hampered access to in-person healthcare services though they had a positive effect on our fight against the COVID-19 pandemic by reducing community transmission.1,2,18 Similar findings have been reported in China19 and the UK.20 A nationwide study in China found a statistically significant decrease in visits at all level health facilities and inpatient discharges after prohibiting intra-city and extra-city transportation in 95% of cities in each province following the lockdown in Wuhan.19 In England, a study observed around a 70% reduction in healthcare utilization immediately after the lockdown in comparison to the average of 2018–2019 in the same period.20 In Catalonia, at the heights of the pandemic, there was a closure of access to the hospitals which also prevented PLWH to access hospitals and HIV units.
Moreover, the lack of knowledge on SARS-CoV-2 at the very early stages of the pandemic and specific information about prevention strategies, as well as the purported potential higher risk among PLWH, might have led to shielding in this population and affected health-seeking behaviours.21,22 Subsequently, people tended to be reluctant to visit health facilities and particularly hospitals, resulting in foregoing or postponing in-person care. In Chicago, a study also found that 30 out of 98 PLWH rescheduled medical visits for a later date.22 A survey of reasons for foregoing care in the US demonstrated that 307 among 1055 individuals (29%) missed care from March to July 2020 due to the fear of SARS-CoV-2 infection.23 These findings are comparable to our study and visits did not return to pre-pandemic levels until the end of 2020, even though the restrictions were gradually lifted six months earlier.
Reduced visits to the HIV units can be explained by different factors. At the height of the pandemic, the health system employed some mitigation strategies to maintain the delivery of lifesaving ART to PLWH minimizing the necessity to visit the HIV units.24 Also, many personnel including infectious disease specialists who worked in the HIV units were channelled into the fight against COVID-19.7 Additionally, some HIV service centres were also repurposed for the fight against COVID-19 substantially reducing programmed visits even though this data for Spain is currently not available. These factors could partly explain the reason why the overall HIV visits were reduced. It is important to mention that, the proportion of PLWH on ART did not reduce in any of the study periods as hospitals in Catalonia made arrangements to deliver medications for chronic patients to pharmacies close to their place of resident during the COVID-19 pandemic.25 HIV units in Catalonia also dispensed ART for longer periods of time and were delivered to the homes of PLWH.
The prioritization policies for health care could explain the considerable impact on hospital admissions and emergency department visits during the pandemic. Healthcare facilities prioritized patients with COVID-19 and other respiratory symptoms to provide prompt medical treatment, which unintentionally reduced the accessibility to patients with non-COVID-19 illnesses.2 In Denmark, the hospital admission rate was reduced significantly for non-COVID-19 conditions.26 Hospital admission rates for respiratory diseases, cancer, and nervous system diseases remained consistently lower during the COVID-19 pandemic.26 These findings highlight the possibility of increased morbidity and mortality due to non-COVID illness in this population and should be investigated.
In contrast, visits to primary care remained unchanged because these centres provided SARS-CoV-2 testing including contact tracing activities at the heights of the pandemic. Besides, the reception of medical care through the public telehealth platform of Catalonia, La Meva Salut,27 is recorded in primary care records as visits. In Catalonia, digital health solutions were deployed to minimize the impact of the COVID-19 pandemic on the accessibility of healthcare services. In this context, patients switched to telehealth visits and teleconsultations, drastically reducing face-to-face visits right after the lockdown was implemented.28 Similar approaches were adopted for visits to HIV units.29 Telehealth consultations are record as primary care visits in patients’ health records. These could explain the relatively stable primary care visits during the lockdown period.
Routinely available CD4 cell count and plasma HIV-RNA viral load testing serve the critical role of monitoring HIV progression and ensuring HIV viral suppression.30 We found reduced laboratory monitoring for these important HIV markers. Typically, stable PLWH with undetectable HIV RNA on ART are controlled twice a year. During the hospital lockdown, most of them had only one control during that whole year. Similar to our findings, another study conducted in an HIV care centre in Barcelona, Spain, also reported reductions in HIV diagnostic tests and plasma HIV RNA tests comparing 2020 versus 2019, albeit no significant difference was observed.9 Given the importance of monitoring HIV markers, it will be crucial to find solutions to keep testing at optimum during pandemic lockdowns and further studies will be important to examine the effects of reduced HIV monitoring on clinical outcomes.
To the best of our knowledge, this is the first study to estimate the utilization of four-type healthcare facilities during the COVID-19 pandemic, particularly in PLWH. Our data sources included a large cohort of PLWH in Catalonia and linked with the PADRIS to access data on public healthcare usage in Catalonia. Furthermore, we used the ARIMA model to predict the expected situation without COVID-19 based on medical visits data since 2017. This in turn allows us to capture the changing dynamics in visits across the different study phases and provides results that would be closer to real-life situations.
Our study has some limitations. First, we were unable to gather information regarding the utilization of telehealth services and distinguish them from the primary care records. This hinders our ability to identify trends in utilizing virtual visits and consultations in primary care services. As a result, we were not able to depict the potential changes in the adoption of digital health services during the three phases after implementing lockdown measures. Second, the absence of information on the specific purposes behind each visit hampers our ability to break down and analyze contacts within each health facility to provide informative insights. Third, we were not able to collect the data from patients who received care outside of Catalonia or Spain during the pandemic and we could be underestimating visits. We however do not expect the difference to be substantial. In addition, the socioeconomic deprivation index used in our analysis is an ecological variable based on place of residence. Place of residence, however, might not always depict an individual's socioeconomic deprivation.
In conclusion, our findings show a significant decline in medical visits in HIV units, hospital admissions, and emergency departments among PLWH during the COVID-19 pandemic. In contrast, visits to primary health care remained unchanged because there were the main centres offering SARS-CoV-2 testing in the early phases of the pandemic but visits to the primary care were not directed at controlling the HIV disease. Several mitigation strategies have been implemented to minimize the barriers, increase adherence to medical assistance, and bridge the gap in accessing care during the pandemic. In this context, the healthcare interruption might have a lesser impact on HIV patients who have been engaged with an annual monitoring system; however, the most vulnerable could be those who were never monitored and thus could not receive immediate diagnosis due to the displacement in hospital services. Therefore, it is imperative to improve the prioritization policy, aiming for a more balanced healthcare service supply that ensure equitable and continuous provision of care during future pandemics.
Data availabilityThe study protocol is available from Dr. Daniel Kwakye Nomah (e-mail, dnomah@igtp.cat). Statistical code for the analysis can be requested from Marcos Montoro-Fernandez, Yesika Diáz, Sergio Moreno, and Jordi Aceiton (mmontorof@iconcologia.net, ydiazr@iconcologia.net, smorenof@iconcologia.net, jaceiton@iconcologia.net). The data for this study is available at the Centre for Epidemiological Studies of Sexually Transmitted Diseases and HIV/AIDS in Catalonia (CEEISCAT), the coordinating centre of the PISCIS cohort and from each of the collaborating hospitals upon request.
Authors’ contributionsYHP, DKN, and JRU conceived and designed the study. YHP, DKN, JA, and MMF had full access to all of the study data, verified the data, and take responsibility for the integrity of the data and accuracy of the data analysis. YHP, DKN, JA, and MMF performed the analyses. YHP and DKN wrote the first draft of the paper and incorporated revisions. All authors contributed to the interpretation of results. All authors and the PISCIS cohort study group critically revised and approved the final manuscript.
FundingThis research was funded by Fundació La Marató de TV3, grant number 202117-30-31. The Fundació La Marató de TV3 had no role in study design, data collection, data analysis, data interpretation, or writing of the report. JMM received a personal 80:20 research grant from Institut d’Investigacions Biomèdiques August Pi i Sunyer (IDIBAPS), Barcelona, Spain, during 2017-2024.
Conflict of interestJMM reported receiving a personal 80:20 research grant from Institut d’Investigacions Biomèdiques August Pi i Sunyer (IDIBAPS), Barcelona, Spain, during 2017–2023 and consulting honoraria and/or research grants from Angelini, Contrafect, Genentech, Gilead Sciences, Jansen, Lysovant, Medtronic, MSD, Novartis, Pfizer, and ViiV Healthcare, outside the submitted work.
AI reported that his institution received grants from Gilead Sciences and MSD; and he personally received consultation fees from Gilead Sciences, ViiV Healthcare, and Thera Technologies; honoraria for lectures and presentations from Gilead Sciences, MSD, Jansen, and ViiV Healthcare; travel support for attending meetings from Gilead Sciences, Jansen, and ViiV Healthcare.
JML has received consulting honoraria from Gilead Sciences, Janssen-Cilag, and ViiV Healthcare outside of the present work.
For the remaining authors none were declared.
The authors are grateful to the Public Data Analysis for Health Research and Innovation Program of Catalonia (PADRIS), the Programme for the Prevention, Control, and Care for HIV, Sexually Transmitted Diseases and Viral Hepatitis (PCAVIHV) of the Ministry of Health, Government of Catalonia for their support, and all staff of PISCIS collaborating hospitals. We are also grateful to the Fundacio La Marato de TV3 for funding support.