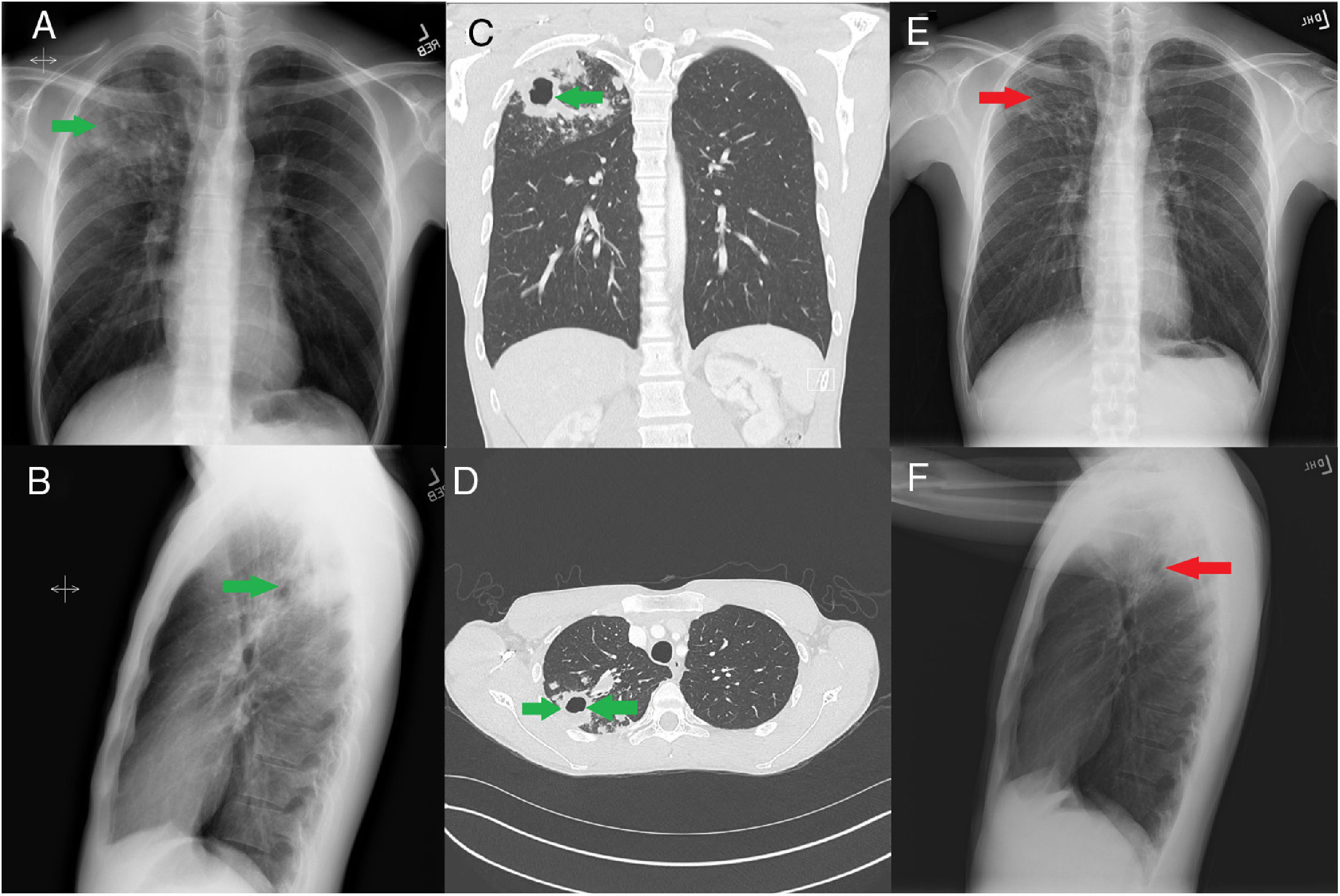
We read with great pleasure the article by Godoy et al. in your esteemed journal regarding surveillance of tuberculosis contacts and treatment strategies.1 We wish to compliment the article by extending the spectrum of disease for reader with an interesting case of treatment failure for latent tuberculosis and conversion to active disease. A 24-year-old asymptomatic male was seen in outpatient TB clinic after being sent from Department of Public health for positive Tuberculosis (TB) skin test (TST). He had recently migrated from China for university education in the US. He denied any past history of TB or close family members being treated for the same in recent past. As a part of immigration work up, he underwent TST which was positive (22mm of induration). QuantiFERON®-TB Gold (QIAGEN, Hilden, Germany) test was also positive. Chest X ray done at the time to rule out active TB was normal. Patient was initiated on Rifampin as treatment of latent TB infection (LTBI) after explaining the risks and benefits. He completed his 4 month regimen for LTBI uneventfully. Patient remained in the US after his treatment of LTBI. Nine months after completion of his treatment for LTBI, patient presented to the clinic with episodes of cough and hemoptysis, he also complained of upper back pain. Clinical examination revealed tympanic note on percussion of right supraclavicular region and cavernous breath sounds in the same region. Laboratory work up revealed normal blood counts and chemistry, HIV and hepatitis screen was found to be normal as well. Chest X ray done at this time showed right upper lobe cavitary lesion (Fig. 1A and B), computed tomography (CT) of the chest showed 2×3cm cavitary lesion in the right upper lobe (Fig. 1C and D). Induced sputum studies were positive for acid fast bacilli (AFB), 3 out of 3. Nucleic acid amplification testing (NAAT) for mycobacterium was positive for Mycobacterium tuberculosis. State lab TB polymerase chain reaction (PCR) test was negative for rifampin resistance. He was initiated on intensive phase of RIPE (Rifampin, Isoniazid, Pyrazinamide and Ethambutol) anti-tubercular regimen, at the end of 2 months he was found to be culture negative. Subsequently his treatment was changed to Isoniazid and Rifampin for 4 months to complete total of 6 months. His chest X-ray repeated at the end of treatment showed resolution of cavitary lesion with residual scarring (Fig. 1E and F).
(A) Chest X-ray PA film showing right upper lobe cavitary lesion (green arrow). (B) Chest X-ray lateral film showing right upper lobe cavitary lesion (green arrow). (C) CT chest coronal view showing right upper lobe cavitary lesion (green arrow). (D) CT chest axial view showing right upper lobe cavitary lesion (green arrow). (E) Chest X-ray PA film showing right upper lobe scarring in area of previous cavitary lesion (red arrow). (F) Chest X-ray lateral film showing right upper lobe scarring in area of previous cavitary lesion (red arrow).
Lifetime risk of developing active disease from latent TB ranges from 5% to 15%.2 However, which latent TB case will transform into active disease remains an enigma. Centers for Disease Control (CDC) gives clear recommendations for treatment of latent as well as active TB infection.2 There is paucity of published literature where patient develops active TB after successful completion of treatment latent TB such as this. Our patient did not travel to any TB endemic region after his initial treatment and remained immunocompetent. Recent article by Jain et al. raised some reasonable doubts about our current understanding and recommendations for treatment of latent TB testing and treatment, especially in the group of patients presenting from the developing world and high risk population.1,3,4 There have been no randomized controlled trials to assess the efficacy of latent TB treatment, comparing patients who receive treatment versus the ones that do not, also there are no head to head comparisons equating various treatment regimens.
Cases such as ours raise many questions. Whether the initial treatment for latent TB was effective? Plausible explanations may include a re-infection (despite staying in the US; low TB prevalence region) or resistance to rifampin during his initial treatment (no rifampin resistance on TB PCR). Both the explanations are possible but seem unlikely. Development of active TB after treatment of latent TB is possible but not well reported. Treating clinicians should maintain a high index of suspicion. Drug resistance should also be tested in cases of recurrence. Bigger question of how effective our current testing for latent TB and subsequent treatment is; remains open ended and unanswered.
Conflict of interestsNone.