The COVID-19 pandemic has led to the admission of numerous patients to intensive care units (ICUs) with acute respiratory distress syndrome (ARDS) and severe respiratory failure. Most of these patients require invasive mechanical ventilation with prolonged orotracheal intubation times and intermittent prone positioning sessions.
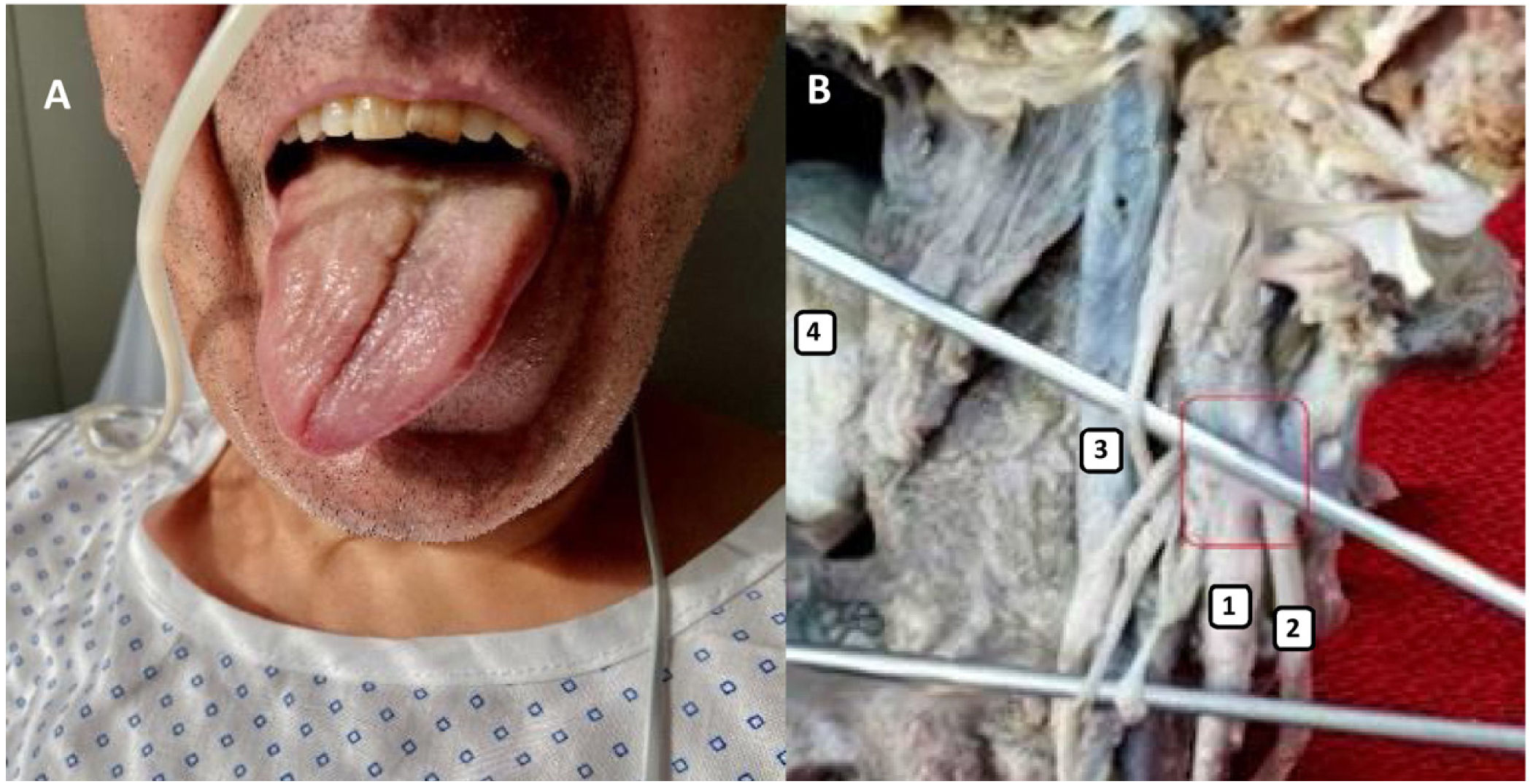
We present the case of a 56-year-old man, with no history of interest, who was admitted to the pulmonology department ward in November 2020 with a diagnosis of acute respiratory failure in the context of bilateral SARS-CoV-2 pneumonia. He worsened rapidly, with severe hypoxaemia refractory to the use of oxygen and elevated FiO2, and orotracheal intubation was decided on. This was maintained for 26 days with invasive mechanical ventilation, requiring up to 18 prone positioning sessions, lasting between 13 and 20h each. After being extubated without incident, the patient suffered from dysphagia and dysphonia not present on admission. He was assessed by otorhinolaryngology and neurology, observing complete paralysis of the right vocal cord and right hemitongue with ipsilateral deviation, as well as paresis of the contralateral vocal cord (Fig. 1A). A diagnosis of Tapia syndrome was established.
Tongue deviation to the right along with loss of strength in the ipsilateral hemitongue in the absence of mechanical restriction suggest mononeuropathy of the 12th cranial nerve, while dysphagia, dysphonia and paralysis of the right vocal cord suggest mononeuropathy of the 10th cranial nerve.
At a topographical level, the absence of dysgeusia and the correct mobility of the soft palate make nuclear involvement of the 10th and 12th cranial nerves due to medulla oblongata lesion unlikely. The most likely lesional topography would be infranuclear, at the level of peripheral 10th and 12th cranial nerves. Although the 12th cranial nerve exits the cranium through the hypoglossal canal and the 10th cranial nerve does so through the jugular foramen, when emerging into the retrostyloid space, the hypoglossal nerve crosses the vagus nerve in the lateral portion of the transverse process of the atlas, with both nerves then remaining in proximity at the piriformis fossa1,2 (Fig. 1B).3
This syndrome is a rare complication that can be associated with invasive airway management. Two cases of patients with Tapia syndrome have been reported in relation to mechanical ventilation processes in patients with SARS-CoV-2 infection. In the case reported by Decavel et al.,4 the patient did not require prone positioning, while the patient described by Yatim et al.5 did.
Probable neurotropism of SARS-CoV-2 is known and its presence in the medulla oblongata of infected patients has been described,6 but not selectively in the nuclei of the 10th and 12th cranial nerves. Cerebral involvement, extrinsic compression and inflammatory disease were ruled out by craniocervical neuroimaging, with traumatic cause considered the most likely aetiology.
Although prone positioning ventilation is a strategy that reduces mortality in patients with ARDS,7,8 it is not without risk and, while it cannot be confirmed unequivocally, in our case in the context of mechanical ventilation and prone positioning, traumatic aetiology was postulated as the most likely. Incorrect use of the laryngoscope and prolonged pressure on the trachea due to excessive inflation of the endotracheal tube cuff have been suggested as the most common mechanisms of injury in ventilated patients.9
The treatment of this syndrome involves establishing a speech therapy and swallowing rehabilitation programme. In this case, the patient experienced complete clinical recovery of swallowing and speech capacity after six months of rehabilitation, with complete mobility of the vocal cords confirmed via control fibreoptic laryngoscopy. This clinical course points to mild neuropraxia or axonotmesis as the mechanism of injury.
Although the scientific evidence is limited, the majority of diagnosed cases are neuropraxia-type injuries, which, by definition, is a reversible process.10 The definitive diagnosis is established by electromyography. However, it is not performed routinely due to difficult access to the muscles of the larynx and because it is an uncomfortable technique. As such, a favourable clinical course would confirm such injury. The therapy aims to reduce recovery time and achieve early functionality.
Finally, the neurological repercussions that orotracheal intubation can cause related to prone positioning changes must be stressed. Although most cases of this syndrome are mild, irreversible damage could occur, requiring the use of a nasogastric tube or gastrostomy to avoid the risk of bronchial aspiration.
Please cite this article as: Cardozo AR, Ruiz I, de la Rosa Carrillo D, Peñacoba P. Síndrome de Tapia y pronación en paciente con neumonía por COVID-19: a propósito de un caso. Enferm Infecc Microbiol Clin. 2022;40:519–520.