Leclercia adecarboxylata is a rare human pathogen belonging to the family Enterobacteriaceae that mainly affects to immunosuppressed patients. These infections, often polymicrobial, are related to impairment of the skin barrier and have been described cases of bacteraemia, endocarditis, peritonitis, pneumonia, cellulitis or septic arthritis unrelated with prosthetic material.1–4
We describe the first case, to our knowledge, of prosthetic joint infection due to L. adecarboxylata and we review the cases of infection by this microorganism in our hospital during a ten year period (2010–2019). All samples were processed according to the standardized procedures established by the Spanish Society of Clinical Microbiology and Infectious Diseases (SEIMC). Leclercia isolates were identified by mass spectrometry (MALDI-TOF MS) and the antimicrobial susceptibilities were performed by turbidimetry (Vitek2) or broth microdilution (Wider and MicroScan WalkAway). Susceptibility to antimicrobials were interpreted according to European Committee on Antimicrobial Susceptibility Testing (EUCAST) criteria.5
We present the case of a 72-year-old female with multiple comorbidities including type 2 diabetes mellitus, a non-determined psychiatric disorder and a mixoid condrosarcoma, who carried a modular knee megaprosthesis secondary to a pathologic fracture. The patient showed a necrotic wound with purulent exudation and exposure of the prosthetic material and during the anamnesis, she reported self-care of the surgical wound with lack of hygiene. She needed treatment with DAIR (debridement, antimicrobials, implant retention) and surgical samples for microbiological culture were obtained. After 24h of incubation, L. adercaboxylata was isolated in 4/5 samples. After 48h Stenotrophomonas maltophilia was also isolated in the same samples. The strain of L. adecarboxylata was susceptible to all tested antimicrobials (penicillins, cephalosporins, carbapenems, aminoglycosides, quinolones, tigecycline, cotrimoxazole, colistin) and S. maltophilia was susceptible to cotrimoxazole and levofloxacin. The patient was treated with intravenous cotrimoxazole 800mg/160mg 3 times a day at hospital. After 15 days the patient was discharged with oral levofloxacin 500mg/day for several months.
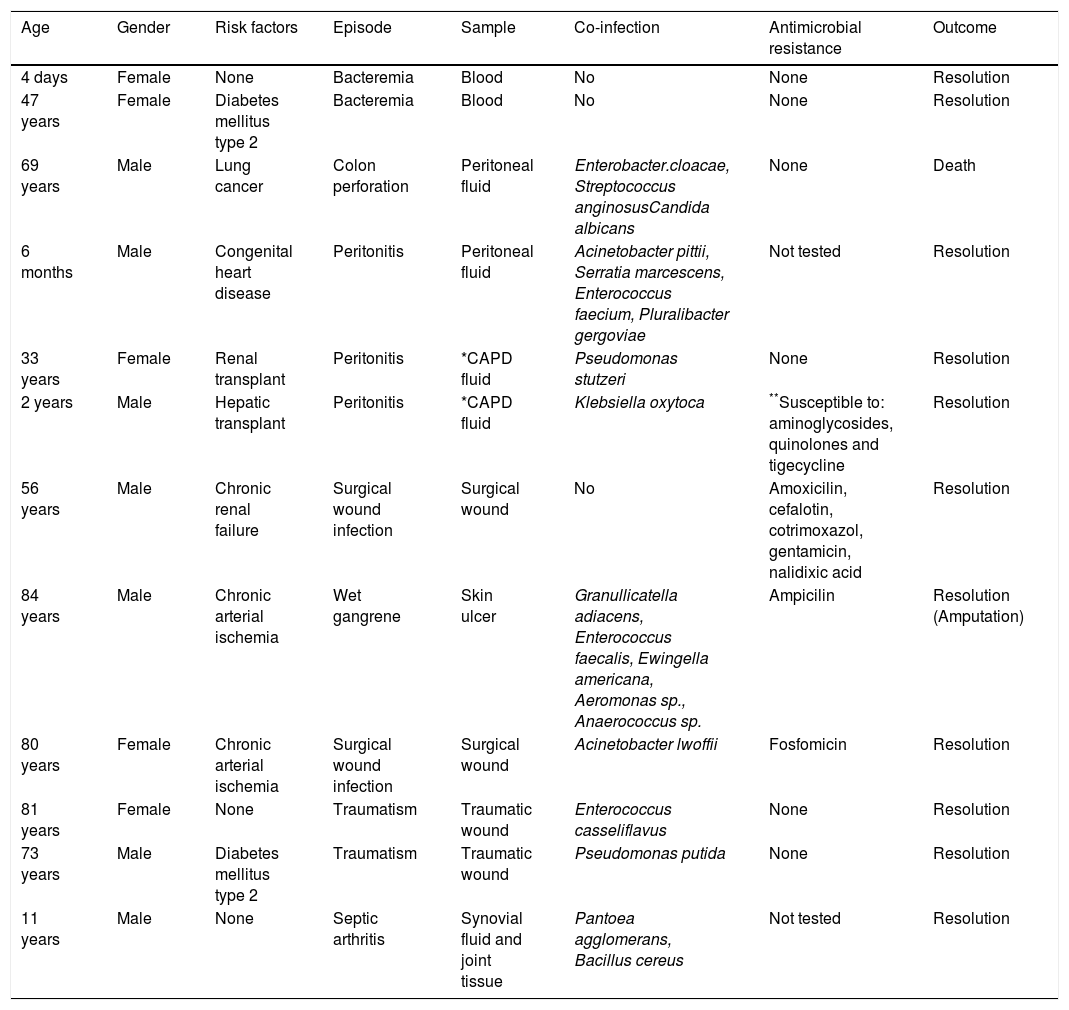
Leclercia adecarboxylata is a pathogen very rarely isolated in our hospital. In the last ten years, it was identified in 13 clinical samples from 12 different patients: two bacteraemia, four intra-abdominal infections, five infections of the skin and soft tissues and one septic arthritis (articular fluid and biopsy). Clinical and demographic characteristics of the patients are shown in Table 1.
Clinical and demographic characteristics of patients with L. adecarboxylata isolates in a ten-year period.
| Age | Gender | Risk factors | Episode | Sample | Co-infection | Antimicrobial resistance | Outcome |
|---|---|---|---|---|---|---|---|
| 4 days | Female | None | Bacteremia | Blood | No | None | Resolution |
| 47 years | Female | Diabetes mellitus type 2 | Bacteremia | Blood | No | None | Resolution |
| 69 years | Male | Lung cancer | Colon perforation | Peritoneal fluid | Enterobacter.cloacae, Streptococcus anginosusCandida albicans | None | Death |
| 6 months | Male | Congenital heart disease | Peritonitis | Peritoneal fluid | Acinetobacter pittii, Serratia marcescens, Enterococcus faecium, Pluralibacter gergoviae | Not tested | Resolution |
| 33 years | Female | Renal transplant | Peritonitis | *CAPD fluid | Pseudomonas stutzeri | None | Resolution |
| 2 years | Male | Hepatic transplant | Peritonitis | *CAPD fluid | Klebsiella oxytoca | **Susceptible to: aminoglycosides, quinolones and tigecycline | Resolution |
| 56 years | Male | Chronic renal failure | Surgical wound infection | Surgical wound | No | Amoxicilin, cefalotin, cotrimoxazol, gentamicin, nalidixic acid | Resolution |
| 84 years | Male | Chronic arterial ischemia | Wet gangrene | Skin ulcer | Granullicatella adiacens, Enterococcus faecalis, Ewingella americana, Aeromonas sp., Anaerococcus sp. | Ampicilin | Resolution (Amputation) |
| 80 years | Female | Chronic arterial ischemia | Surgical wound infection | Surgical wound | Acinetobacter lwoffii | Fosfomicin | Resolution |
| 81 years | Female | None | Traumatism | Traumatic wound | Enterococcus casseliflavus | None | Resolution |
| 73 years | Male | Diabetes mellitus type 2 | Traumatism | Traumatic wound | Pseudomonas putida | None | Resolution |
| 11 years | Male | None | Septic arthritis | Synovial fluid and joint tissue | Pantoea agglomerans, Bacillus cereus | Not tested | Resolution |
L. adecarboxylata infections range from superficial infections by skin lacerations in immunocompetent patients to invasive infections in immunosuppressed patients secondary to cirrhosis, type 2 diabetes mellitus or solid organ transplant.1,6 There are many similarities between our series and the cases reported in the literature, such as immunosuppressed patients due to cancer, chronic organ insufficiency or a failure in defense barriers. The described population is elderly or midlife. In our series, most patients are in that age range, but four out of eleven were pediatric patients (including one newborn). According to previously published cases, L. adecarboxylata can be isolated from many different sample types, though it is mostly found in blood samples.1,7,8 In our series, skin and soft tissue where the main sources followed by abdominal samples (CAPD or peritoneal fluids). We also present the singularity of this first documented case of joint infection related to prosthetic material.
Antimicrobial susceptibility in the reported cases presents a pattern similar to Escherichia coli, and this is also found in our isolates. Most strains are susceptible to all antimicrobials with activity against gram-negative bacteria,1,7,8 though it may acquire resistance mechanisms as other members of the Enterobacteriaceae. We detected one case in which L. adecarboxylata showed resistance to carbapenems, due to a VIM metallobetalactamase, probably from a VIM producer K.oxytoca that was isolated in the same sample. A previous report described the isolation of VIM-producing L. adecarboxylata9 from a surveillance study focused in hands hygiene. There has been another case described of carbapenem resistance, but it was due to NDM producer.10
The episodes published describe that L. adecarboxylata was mostly identified by biochemistry panels such as Microscan®1,2 or turbidimetry by Vitek2 Compact®,3,8 and in one case by proteomic techniques as MALDI-TOF.6 In some cases, genomic techniques were needed to confirm the isolate identification, as the sequencing of 16S rRNA gene.1,7 In our case MALDI-TOF was the main tool for bacterial identification. The similarities between Escherichia species and L. adecarboxylata for diagnosis by phenotypic procedures may lead to misidentification. For that reason, molecular methods are needed in order to distinguish between these two microorganisms and to avoid misdiagnosis.