A 72-year-old woman, hypertensive, diagnosed with mantle cell lymphoma in 1999 for which she received chemotherapy and haematopoietic stem cell transplantation. She relapsed in 2008, undergoing a second haematopoietic stem cell transplant, achieving complete remission. She was later diagnosed with intraductal breast carcinoma in 2009 and was treated with surgery and adjuvant radiation therapy. There was no subsequent evidence of neoplastic disease. She was admitted to hospital in April 2020 due to intense right ear pain with irradiation to the cervical region and asthenia of one week duration. Examination of the ENT territory was normal. Analytical tests showed a C-reactive protein (CRP) 280 mg/dl (0–50 mg/dl), normocytic anaemia with haemoglobin of 10.3 g/dl and leukocytosis (16,000/mm3) with neutrophilia (13,900/mm3). The rest of the biochemical tests were normal and the chest X-ray was without relevant alterations.
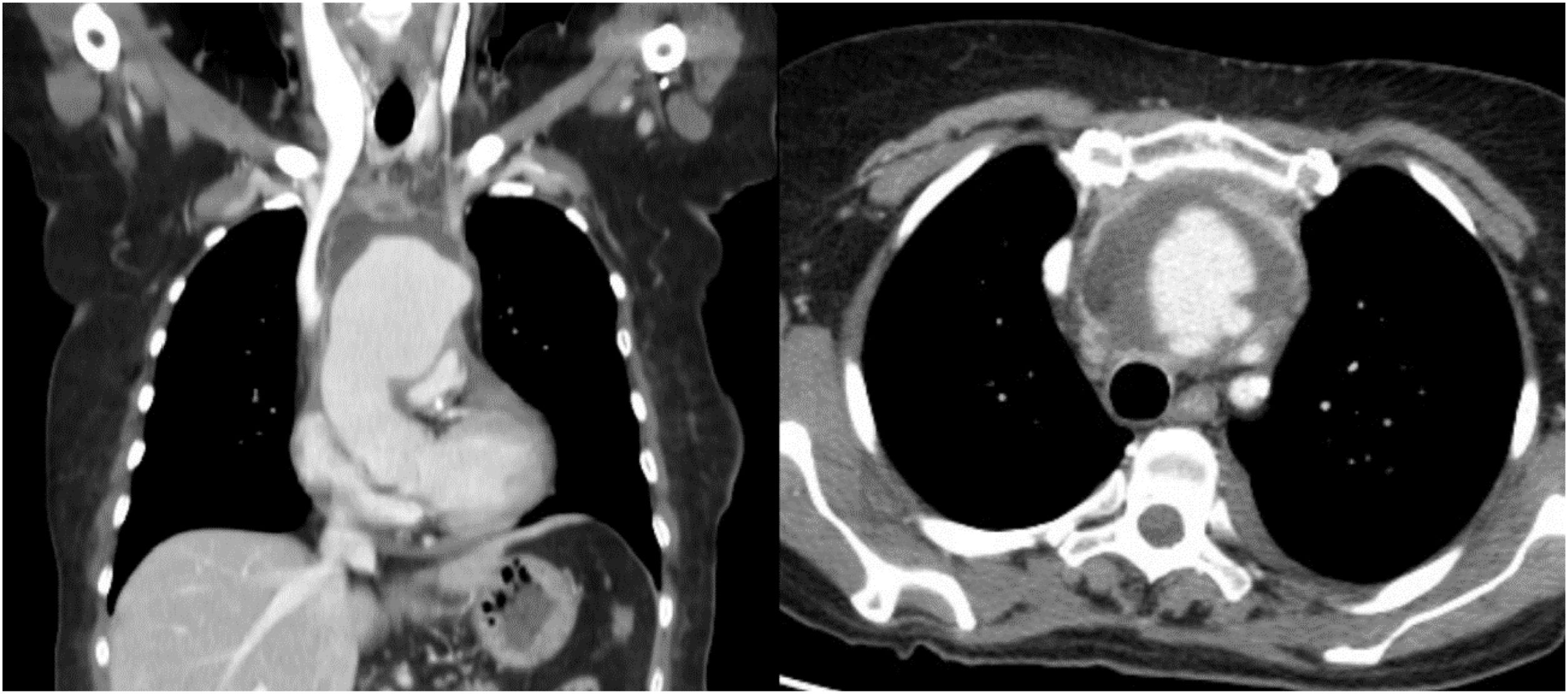
In the context of the COVID pandemic, a SARS-CoV-2 PCR test was requested, which was negative, as well as an ICT serological test, which was positive, for which reason she was admitted to the Internal Medicine Service with a diagnosis of COVID-19 disease. Her symptoms persisted despite increasing analgesic treatment and the laboratory parameters worsened, so blood cultures were drawn, empirical antibiotic treatment with amoxicillin/clavulanate 875/125 mg every 8 h was initiated, and a cervicothoracic CT scan was performed that revealed a mycotic ascending aortic aneurysm extending to the origin of the supra-aortic trunks (Fig. 1).
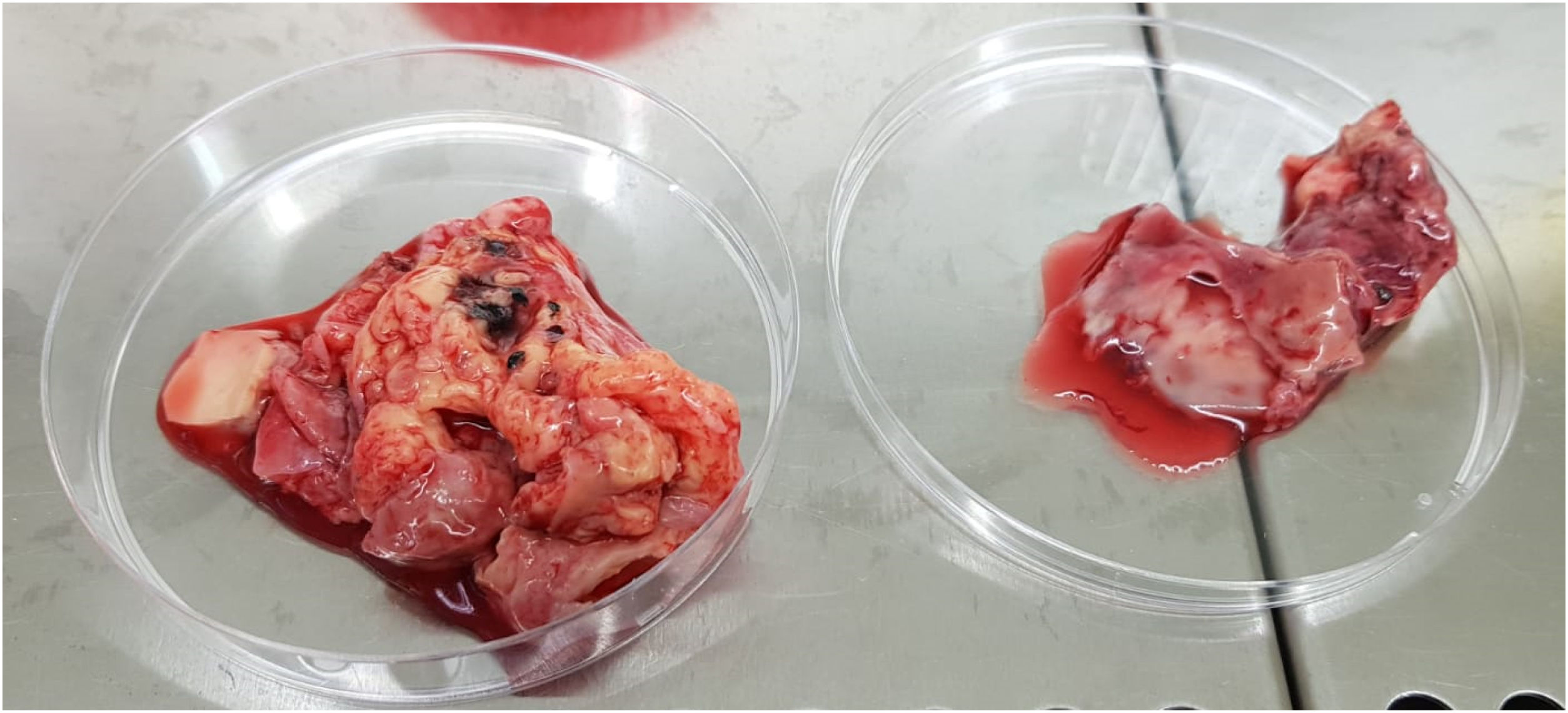
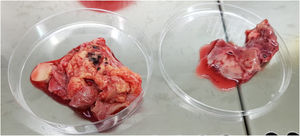
Clinical courseEmergent surgery was performed, observing mycotic pseudoaneurysm from the ascending aorta to the distal arch (Fig. 2), proceeding to its replacement with debranching of the supra-aortic trunks and implantation of a four-branch Polythese prosthesis. In the ICU, treatment was escalated to piperacillin/tazobactam 4/0.5 g every 6 h, requiring inotropic support at high doses, despite which the patient died in the immediate postoperative period. In the microbiological study of the surgical specimen, flat colonies with irregular borders and velum production were isolated in anaerobic media, and were identified as Clostridium septicum (C. septicum) by GRAM and MALDI TOF (Bruker Daltonic) staining. The sensitivity study by E-test showed sensitivity of the microorganism to penicillin, amoxicillin-clavulanate, piperacillin-tazobactam, carbapenems, clindamycin and metronidazole. Blood cultures were negative.
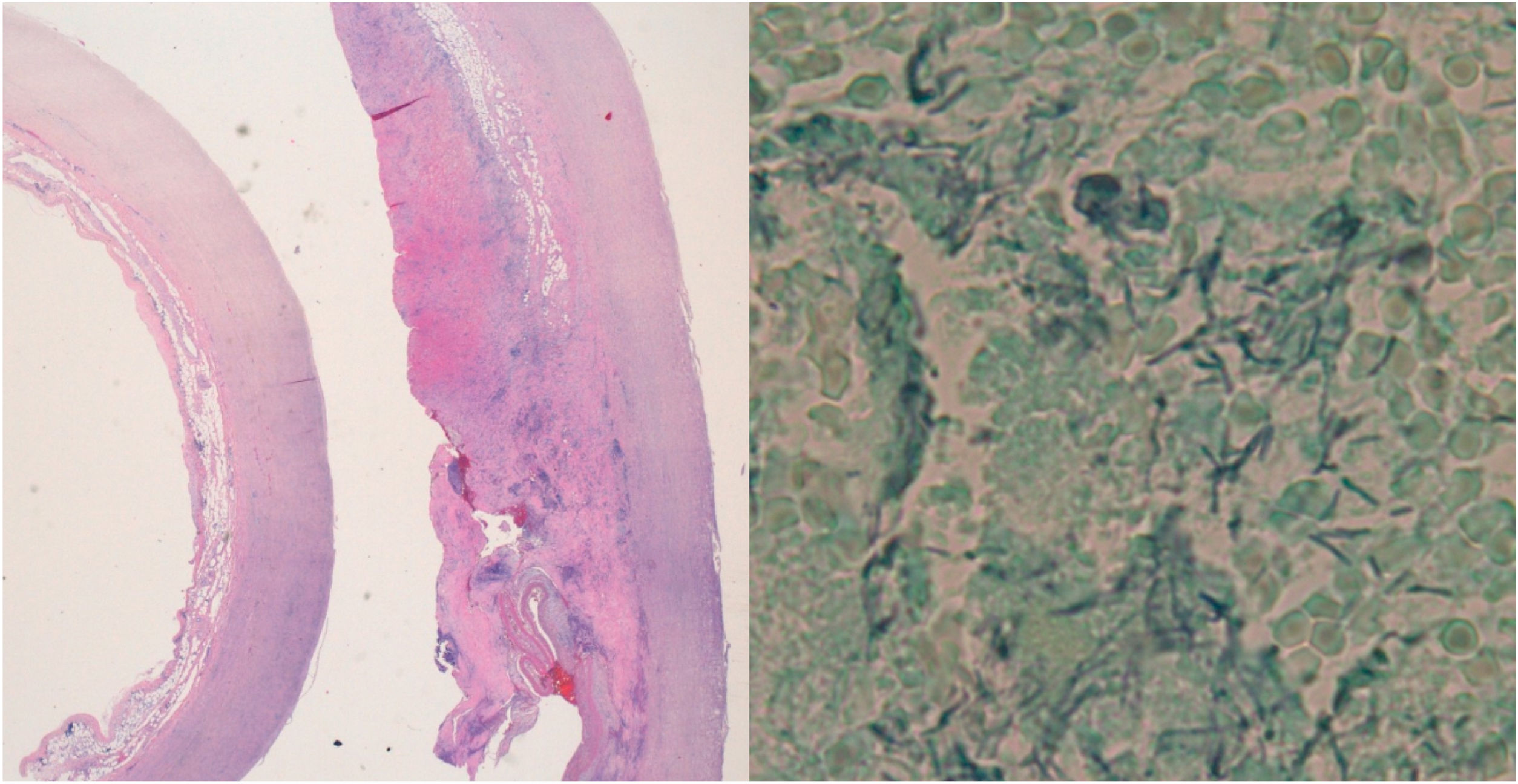
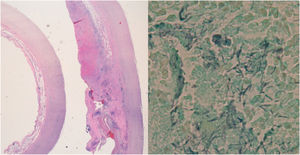
In the PAS stain and the Grocott's stain of the pathological anatomy (Fig. 3), filamentous pleomorphic bacilliform structures were observed, which were identified as C. septicum after sequencing the 16S and 18S regions of the rRNA in the paraffin biopsy.
DiscussionC. septicum is a sporulated anaerobic gram-positive bacillus found in soil and in the human gastrointestinal tract. It produces a toxin capable of rapidly inducing tissue necrosis, which explains its virulence. It represents 1.3%1 of Clostridium sp. infections and its most frequent form of presentation is as a skin and soft tissue disease, neutropenic enterocolitis and bacteraemia.2 Vascular infections are a rarity, with fewer than 100 reported cases of aortitis.
Infection of aortic aneurysms is rare, being observed in less than 3% of the total number of cases.3 The predominant microorganisms are Salmonella and Staphylococcus aureus, although others have also been described, such as Streptococcus sp. Listeria monocytogenes and Candida sp. Noteworthy as a peculiarity of aortitis caused by C. septicum is the presence of periaortic gas in more than 90% of cases.4 The antibiotic treatment of choice consists of beta-lactams together with clindamycin or doxycycline to inhibit toxin synthesis.5 In addition, patients should be screened for an underlying neoplasm, present in 60% of patients, the most frequent being a neoplasm of the colon (56%). Despite initiating early treatment, the prognosis for this condition is poor, with a mortality of 75% per year even with treatment, and 100% if surgery is not performed.1,3,5
Aortitis caused by C. septicum is an infrequent condition, but if it is suspected, intensive and early treatment is necessary due to its high mortality. In our patient, the absence of symptoms and signs suggestive of aortitis and the epidemiological situation made diagnosis difficult. The pandemic situation should not divert our attention from other potentially lethal processes6, both infections with lung involvement such as influenza7 and other non-infectious diseases (acute coronary syndromes, neoplasms, etc.)8 that during the last year have remained hidden under the shadow of SARS-CoV-2.
Please cite this article as: Dueña L, Varona J, Bereciartua E, López L. A la sombra de la pandemia. Enferm Infecc Microbiol Clin. 2022;40:39–41.