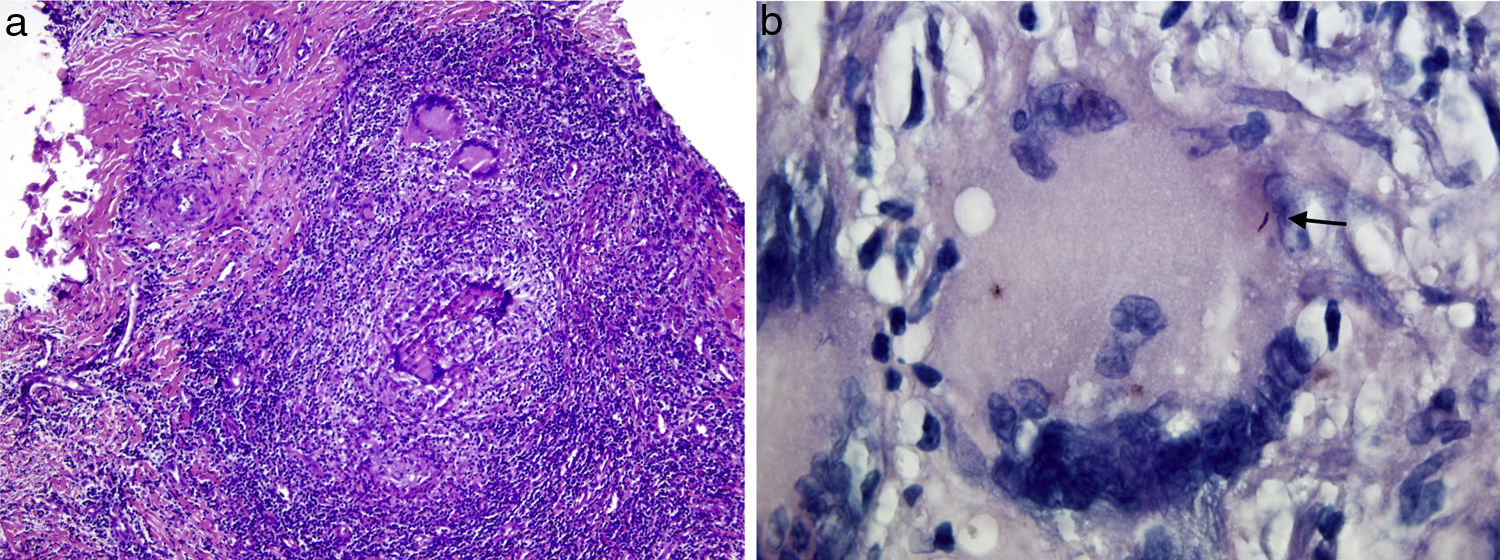
An 86-year-old woman came in due to a nail lesion for the past 4 months linked to trauma she had suffered 6 months before she started having signs and symptoms. An examination revealed a hyperkeratotic plaque compromising the entire nail bed of her index finger on her right hand (Fig. 1). She had no associated local or regional lymphadenopathy and no systemic symptoms. A plain X-ray of the finger, a complete blood count, clinical chemistry and an immunity study were ordered. The X-ray showed no bone impairment. The results of all the other tests were normal.
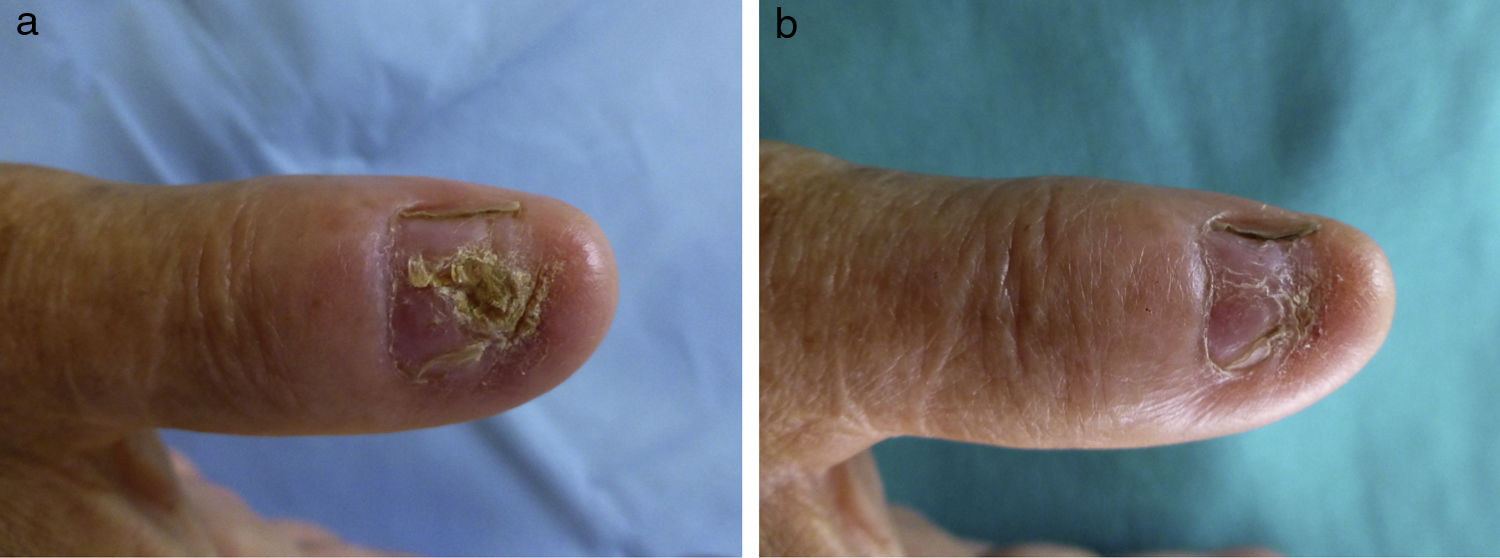
Clinical diagnosis and courseAs onychomycosis was initially suspected, a sample was taken for mycological study. This showed a discrepancy between direct examination, in which filaments were seen, and culture, which was negative. Treatment was started with itraconazole, but no clinical response was achieved. As a result, spinocellular carcinoma was suspected and a biopsy was done. A histopathology study revealed granulomatous inflammation, raising a differential diagnosis with a mycobacterial infection and sarcoidosis. A second biopsy was done to obtain material for microbiological study, part of which was re-sent for histopathological study. It showed necrotising granulomas with AAFB using Ziehl–Neelsen staining (Fig. 2). Mycobacterium tuberculosis sensitive to streptomycin, rifampicin, isoniazid, pyrazinamide and ethambutol was isolated in the culture.
The patient was in good general condition with no respiratory signs or symptoms. One of the complementary tests ordered was a Mantoux skin test, which was positive with an area of induration measuring 20mm. Another was a chest X-ray, which showed no abnormalities. Consequently, bacilloscopy and sputum culture were considered unnecessary. Although the patient had no urinary or gastrointestinal signs or symptoms, the study was completed with determinations of AAFB in faeces and urine. Their results were negative. In light of these findings, the patient was diagnosed with cutaneous tuberculosis and tuberculostatic treatment was started with an excellent response (Fig. 3).
CommentsSkin impairment is seen in 1–2% of cases of M. tuberculosis infection, although its incidence is lower in developed countries.1 The type of lesion depends on the route of infection and the immune status of the host.2 The skin and mucosa constitute an unusual pathway for entry. Exogenous inoculation with this infectious agent occurs through a point where the skin barrier has been broken and may take one of the following clinical forms: tuberculous chancre, tuberculosis verrucosa cutis or, in some cases, lupus vulgaris.3–5 Tuberculosis verrucosa cutis, a paucibacillary form, typically manifests as hyperkeratotic plaques in the area of inoculation of previously infected individuals with a good immune response against M. tuberculosis.6 These plaques usually develop in places exposed to trauma, such as the backs of the hands and fingers in adults and the legs in children.7,8 Although the nails are exposed to frequent trauma, reports of tuberculous onychopathy with no impairment of underlying bone, as in our patient, are rare. The therapeutic approach is similar to that taken in pulmonary tuberculosis.5,9,10
Identification of the microorganism constitutes an absolute diagnostic criterion; however, it has low sensitivity under paucibacillary conditions and is negative in 50% of cases.5
The differential diagnosis includes spinocellular carcinoma, viral warts, deep mycoses, verrucous lupus vulgaris and sarcoidosis. Infections with atypical mycobacteria may cause similar signs and symptoms, and a microbiological study is essential for their diagnosis. Identification techniques based on molecular biology have gained ground previously occupied by traditional culture.
In our case, they supported a diagnosis of tuberculosis verrucosa cutis, as did a positive Mantoux skin test, isolation of the bacillus in the nail bed, a history of trauma in the same location with no impairment of underlying bone, lymph node impairment and systemic signs and symptoms. Treatment response represents a key retrospective parameter in the diagnosis of the disease.
In conclusion, nail infection caused by M. tuberculosis is uncommon, probably thanks to the protective role played by the lamina over the nail bed. This condition may present a diagnostic challenge in view of the limited expressiveness of diseases in nails and the low sensitivity of culture under paucibacillary conditions. It should be borne in mind in cases of severe onychopathy that does not respond to oral antifungals and a histopathological study that rules out malignancy.
Please cite this article as: Sainz-Gaspar L, Rosón E, Suárez-Peñaranda JM, Vázquez-Veiga H. Distrofia ungueal hiperqueratósica. Enferm Infecc Microbiol Clin. 2018;36:664–665.