A retrospective study was conducted by collecting microbiological tuberculosis (TB) data in Castile and León during the year 2013 in order to determine the incidence and distribution of TB, and resistance to the tuberculostatic drug, and compare them with the epidemiological data provided by the Department of Epidemiological Surveillance (SIVE).
Material and methodsMicrobiologists of the 14 hospitals of the Castile and León public health network (GRUMICALE) collected epidemiological, microbiological, and management data from the Microbiology laboratories in the community during the year 2013. A single isolate of Mycobacterium tuberculosis complex (MTC) per patient was considered.
ResultsThe study included a total of 270 MTC isolates (an incidence rate of 11.63 cases/100,000inhab./year). A total of 288 cases of TB (11.43 cases/100,000inhab. year) were recovered using epidemiological data, which included 243 confirmed, 29 suspected, and 16 as probable cases. Pulmonary TB was predominant, followed a long way off by the pleural TB and the remaining locations. A total of 27,620 samples were processed for mycobacterial detection. Mycobacterial growth was observed in 3.46% of automated fluid cultures, and 50.37% were positive by direct staining of the smear. Resistance to one tuberculostatic drug, mostly to isoniazid, was observed in 16 (5.92%) isolates of M. tuberculosis (MT). The province with greater incidence and number of isolates was León (24.23 cases/100,000inhab./year), with the highest being observed in El Bierzo health area (30.46 cases/100,000inhab./year).
ConclusionsAn adequate collection of microbiological information is essential to determine the epidemiology of TB in our region.
Estudio retrospectivo que recoge datos microbiológicos de tuberculosis (TB) en Castilla y León durante el año 2013 para conocer los datos microbiológicos de incidencia y distribución de TB, resistencias a los fármacos antituberculosos y compararlos con los datos epidemiológicos ofrecidos por los servicios de vigilancia epidemiológica (SIVE).
Material y métodosMicrobiólogos de los 14 hospitales de la red sanitaria pública de Castilla y León (GRUMICALE) han recogido datos epidemiológicos, microbiológicos y de funcionamiento de los laboratorios de microbiología de la comunidad durante el año 2013. Se consideró un solo aislamiento de Mycobacterium tuberculosis complex (MTC) por paciente.
ResultadosSe obtuvieron 270 aislamientos de MTC (tasa de incidencia de 11,63 casos/100.000 hab./año). Según datos epidemiológicos, se recogieron un total de 288 casos de TB (11,43 casos/100.000 hab./año), 243 confirmados, 29 sospechosos y 16 probables. Predomina la localización pulmonar, seguida de lejos por la pleural y por el resto. Se procesaron un total de 27.620 muestras para micobacterias. En un 3,46% de los medios de cultivos líquidos se obtuvo crecimiento de micobacterias, y en un 50,37% la tinción directa (baciloscopia) fue positiva. Dieciséis aislamientos de Mycobacterium tuberculosis (MT) presentaron resistencia a algún fármaco antituberculoso, predominando la resistencia a isoniazida (5,92%). La provincia con mayor incidencia y número de aislamientos fue León (24,23 casos/100.000 hab./año), siendo la máxima en el área sanitaria de El Bierzo (30,46 casos/100.000 hab./año).
ConclusionesUna adecuada recogida de la información microbiológica es fundamental para el conocimiento de la epidemiologia de la TB en nuestra comunidad.
According to the data published by the epidemiology services of Castile-León, the overall incidence of tuberculosis (TB) in the region in 2013 was 11.43 cases per 100,000 population per year, 8.29 of which corresponded to pulmonary tuberculosis (PTB). According to the data of the Red Nacional de Vigilancia Epidemiológica (RENAVE) [Spanish National Epidemiological Surveillance Network] project, in 2013 the incidence in Spain was 10.42 cases per 100,000 population per year,1,2 with Spain occupying ninth place in Europe behind Hungary (17.7 cases/100,000 population/year). The Castile-León region occupied sixth place in 2011 for the number of TB cases (354 cases), behind Galicia (432 cases); Catalonia topped the list with 929 TB cases registered that year. In 2013, if we include the autonomous cities of Ceuta and Melilla, which have the highest incidence rates, Castile-León ranked tenth behind Asturias. The notification of TB cases is a priority for public health and microbiology laboratories play a crucial role in this complex process. It is the laboratories that process the clinical samples and issue the reports which are sent not only to the clinician, but also to the epidemiology services in the autonomous regions. This helps generate important statistical data, such as the total number of cases of TB, the percentage and the smear-positive rate. The process of collecting that data carried out by the epidemiology services is a key factor in being able to provide epidemiological data (ED) which corresponds with the actual situation. However, it is the work of the microbiology laboratories that makes it possible to provide final results on identification and sensitivity to anti-TB drugs with which to complete the process.
ObjectivesThe first objective of this study is to determine the incidence of TB in the region of Castile-León over a full year (2013) by collecting the available microbiological data (MD) and comparing them with the same type of data, but obtained and published by the Autonomous Region of Castile-León epidemiology services (ED). The second objective is to analyse certain parameters on how the samples are processed for the detection and culture of mycobacteria in the region's public network of microbiology laboratories over the same period. The third objective is to study the distribution of TB in the region: the number of Mycobacterium tuberculosis complex (MTC) isolates; the incidence by provinces and healthcare areas; and the incidence and distribution of resistance to anti-TB drugs.
Material and methodsCriteria used by the epidemiology services of the Castile-León region to define TB casesThe region's Sistema de Vigilancia Epidemiológica (SIVE) [epidemiological surveillance system] follows the criteria of the European Centre for Disease Prevention and Control (ECDC). This classification divides TB cases by applying clinical and laboratory criteria. It considers three types of cases. The first, suspected case, is when there are signs, symptoms and radiological evidence of active TB leading to anti-TB treatment or a pathology or post-mortem result compatible with TB which has required anti-TB treatment. A confirmed case is when there is positive culture for MTC, or detection by PCR on direct sample and acid–alcohol-fast bacilli (AAFB) staining both positive. A probable case is when there is positive AAFB or positive direct detection by PCR, or histopathological and/or post-mortem studies are positive. The table of anatomical TB sites, and the calculation of incidence and smear-positive rates, are available for consultation on the Internet, both in the same document.3 The sources of information make up the SIVE, and it is the primary care and specialised physicians who report the cases they come across in their clinics through the Notifiable Disease Notification System of Castile-León. Other sources are the microbiology laboratories, the regional registry of AIDS cases, prisons, and others which are unspecified.
Criteria of the Grupo de trabajo de Microbiología de Castilla y León (GRUMICALE) [Castile-León Microbiology Working Group]This group is made up of microbiologists from all the Salud Castilla y León (SACYL) [Castile-León Health Service] public hospitals, consisting of ten provincial hospital complexes, one regional hospital and three local hospitals. A data collection form was drawn up for all MTC isolates registered in the autonomous region in 2013, which extended well into 2014, because the region's epidemiology statistics were published in July 2014. Only one MTC isolate was included per patient, meaning that the number of isolates corresponded to the number of TB cases. Any strain of MTC isolated in solid and/or liquid culture media and identified by biochemical and/or molecular techniques in each laboratory was considered an isolate. Differentiation within the TB complex was performed, depending on each centre, using commercial molecular techniques such as GenoType-MTBC and GenoType-MTBDR (Hain Lifescience®), or in the corresponding reference centres. The analysis of resistance was carried out by means of the above techniques or by sending the strain to the reference centre. The study of each case was completed by reviewing the patient's medical records. Annual TB rates per 100,000 inhabitants per year were calculated as follows: cases of MTC according to MD or ED (numerator) and arithmetic mean of the census data corresponding to 01/01/2013 and 01/01/2014, which shows an average population of 2,507,790 in the Castile-León region. In addition, a second form was added to collect TB anatomical sites using the same classification as that used to collect ED.
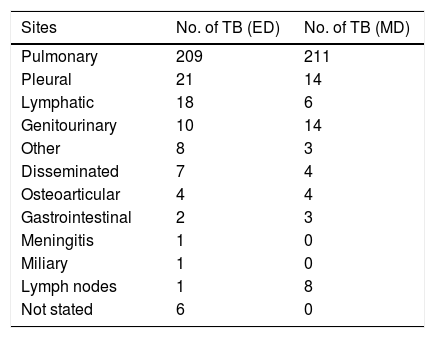
ResultsEpidemiological dataThe total number of MTC isolates/TB cases according to ED was 288, 243 of which were confirmed cases, 29 suspected cases and 16 probable cases. According to the MD collected in this study and derived from culture, 270 isolates of MTC/TB cases were obtained in this same period. Maintaining the total number of 288 TB cases (ED), if the MD had been taken into account, the rate of confirmed cases would have gone from 84.6% (ED) to 93.75% (MD) in 2013. The incidence of TB in general, calculated for the entire region in this period by ED, was 11.43 cases/100,000pop./year, while that obtained by MD was 11.63 cases/100,000pop./year, all confirmed by culture. In the case of PTB, the number of MTC isolates/PTB cases according to ED was 209 (8.29 cases/100,000pop./year), and according to MD was 211 (8.41 cases/100,000pop./year). Much less common were pleural TB (21 cases vs 14) and genitourinary TB (10 cases vs 14), with differences in all the other sites (Table 1).
Distribution of tuberculosis (TB) according to the anatomical site obtained by epidemiological (ED) or microbiological (MD) procedures.
| Sites | No. of TB (ED) | No. of TB (MD) |
|---|---|---|
| Pulmonary | 209 | 211 |
| Pleural | 21 | 14 |
| Lymphatic | 18 | 6 |
| Genitourinary | 10 | 14 |
| Other | 8 | 3 |
| Disseminated | 7 | 4 |
| Osteoarticular | 4 | 4 |
| Gastrointestinal | 2 | 3 |
| Meningitis | 1 | 0 |
| Miliary | 1 | 0 |
| Lymph nodes | 1 | 8 |
| Not stated | 6 | 0 |
A total of 27,620 samples were processed for mycobacteria in 2013, with a total of 26,476 direct staining (470 of them positive; 1.77%). Direct PCR was performed on 413 (56 of them positive; 13.55%) and 25,895 cultures in liquid medium (898 positive; 3.46%) compared to 9337 in solid medium (244 positive; 2.61%). A total of 270 MTC isolates were computed; 136 (50.37%) had direct positive staining. Furthermore, 259 isolates of atypical mycobacteria were counted, 18 of which had positive direct staining (6.94%).
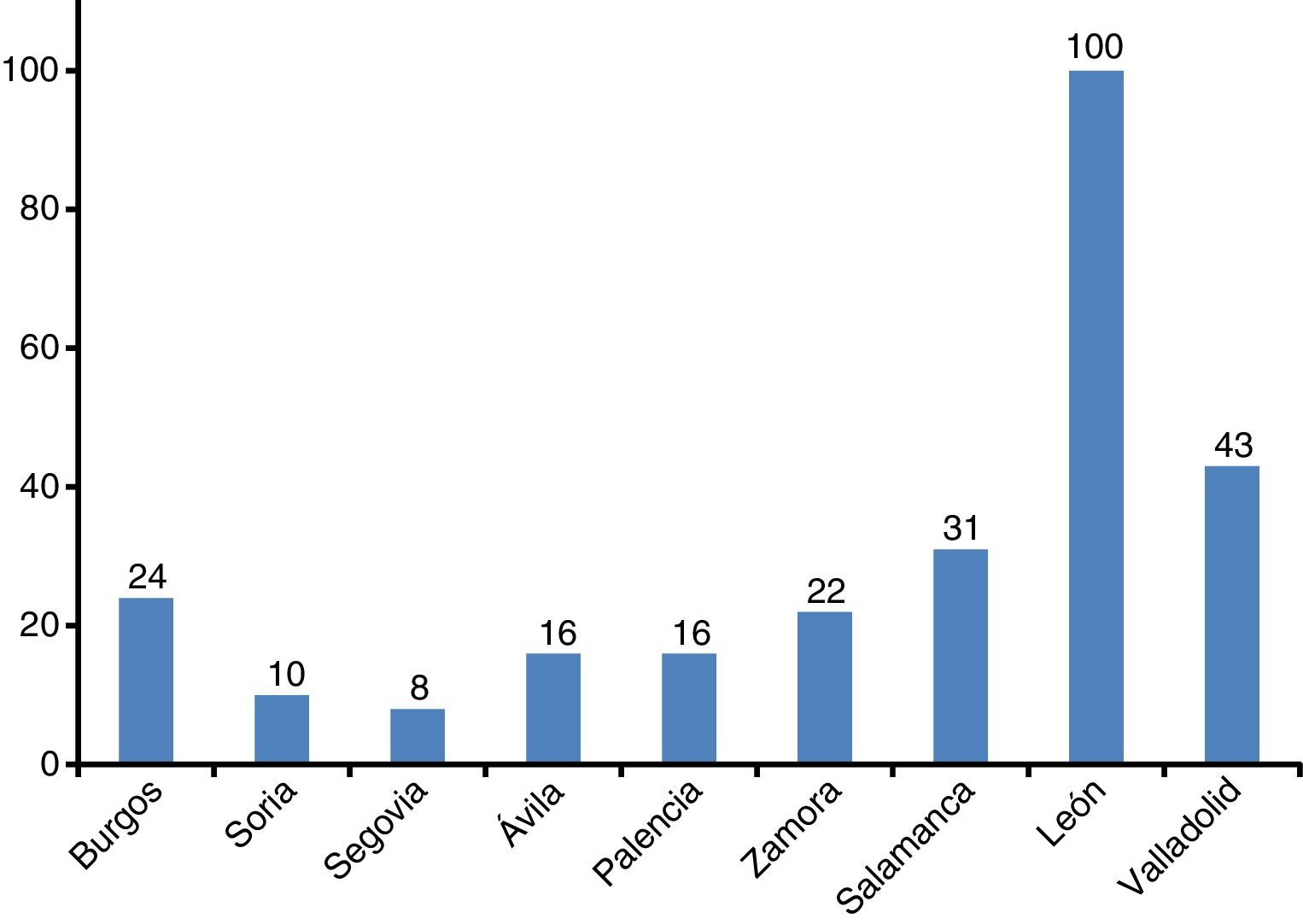
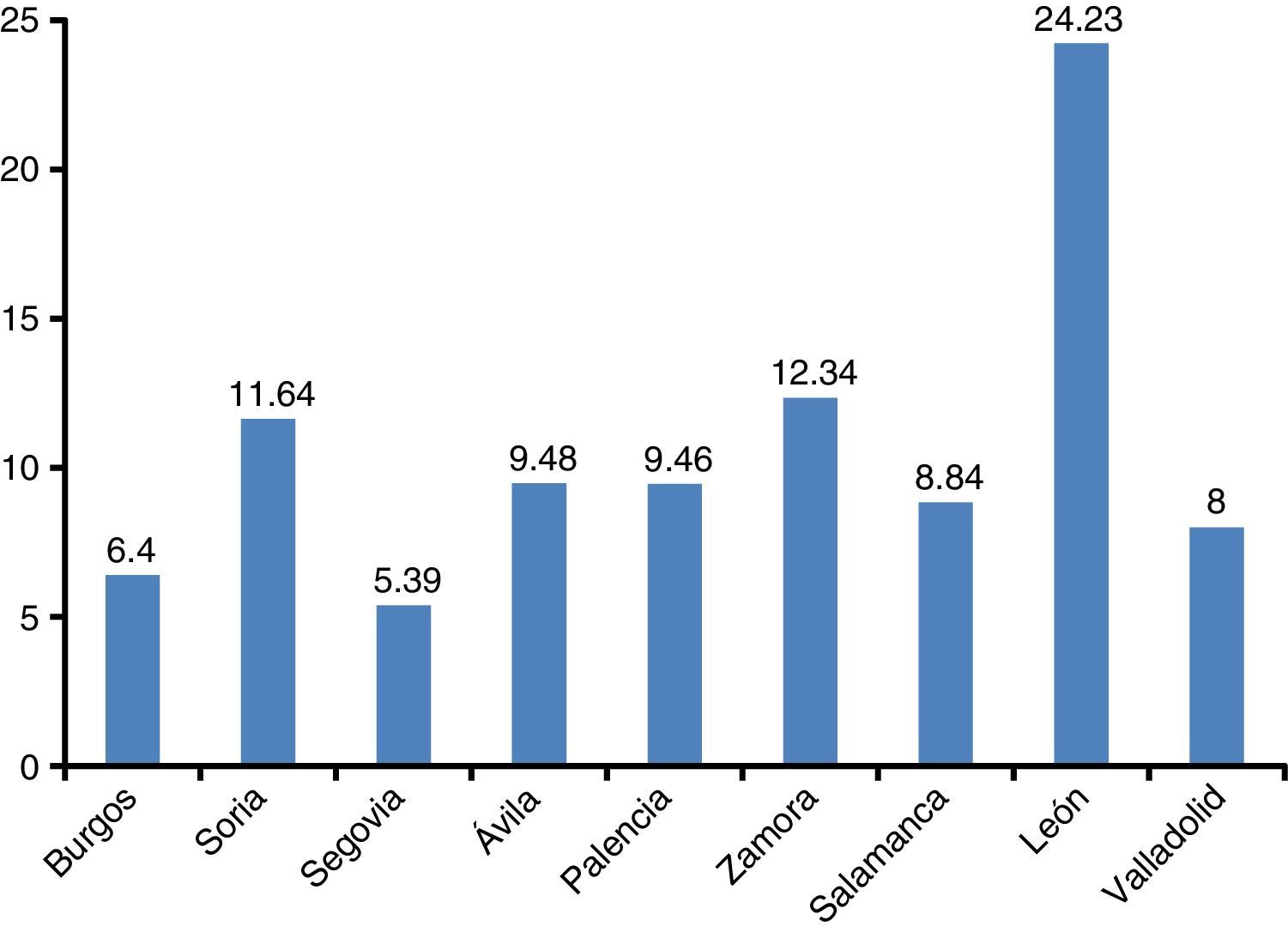
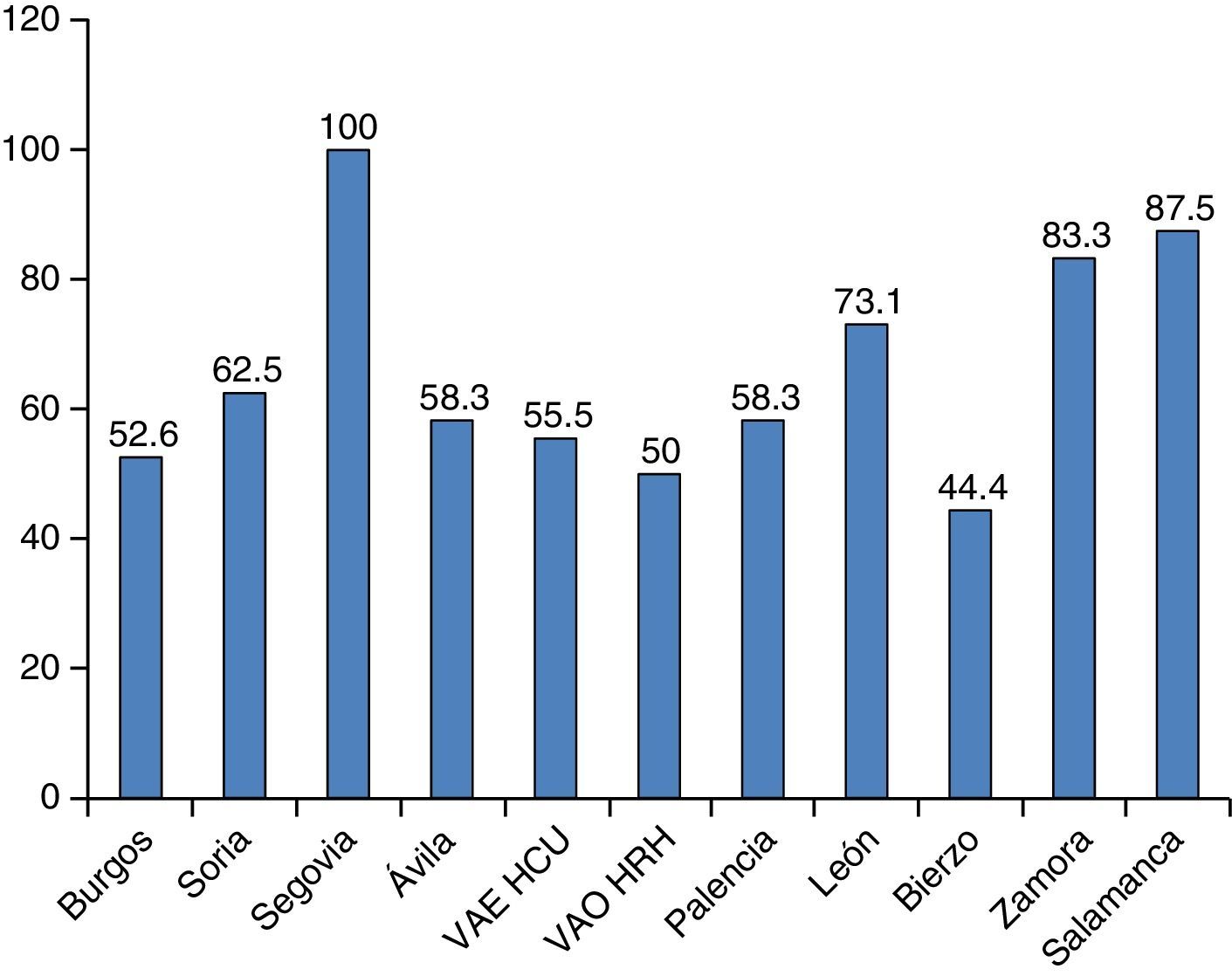
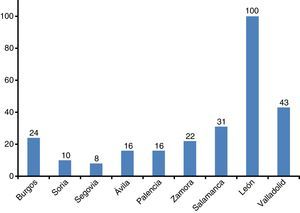
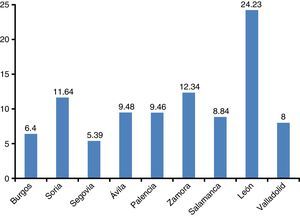
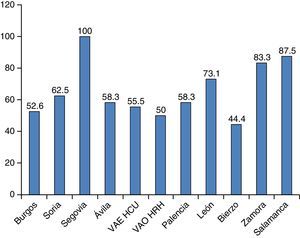
Distribution of isolates of M. tuberculosis and of resistance by province and health areaThe province with the most cases (Fig. 1) was León (100 cases), followed by Valladolid (43 cases), Salamanca (31 cases), Burgos (24 cases), Zamora (22 cases), Ávila and Palencia (16 cases each), Soria (10 cases) and Segovia (8 cases). In the province of León, 59 cases corresponded to the León health area and 41 to the El Bierzo health area. León was the province with the highest incidence (24.23), and it was much higher in El Bierzo (30.46) than in the rest of the province (18). In the province of Valladolid, the largest number of cases was registered in the area of Valladolid East (Hospital Clínico Universitario) with 31 cases, while in Valladolid West (Hospital Río Hortega) only 12 cases were registered. When corrected for the size of the population (Fig. 2), the province with the highest incidence is León (24.23), followed by Zamora (12.34), Soria (11.54) and then the remaining provinces. In terms of smear-positive cases, the percentage was highest in the Segovia health area, where 100% of MTC isolates had positive direct staining (Fig. 3), followed by Salamanca (87.5%), Zamora (83.3%), León health area (73.1%) and then the rest. There were no great differences in the percentage of smear-positive cases between the two Valladolid health areas (55.5% for Hospital Clínico vs 50% for Hospital Río Hortega). However, in the El Bierzo health area, the percentage of smear-positive cases was significantly lower (44.4%) than in the rest of the province of León (73.1%).
Distribution of smear-positive cases by healthcare area in the Castile-León region in 2013. The figure represents the percentage of isolates of Mycobacterium tuberculosis complex that had positive direct staining. VAE HCU: Valladolid East Health Area (Hospital Clínico Universitario); VAO HRH: Valladolid West Health Area (Hospital Río Hortega).
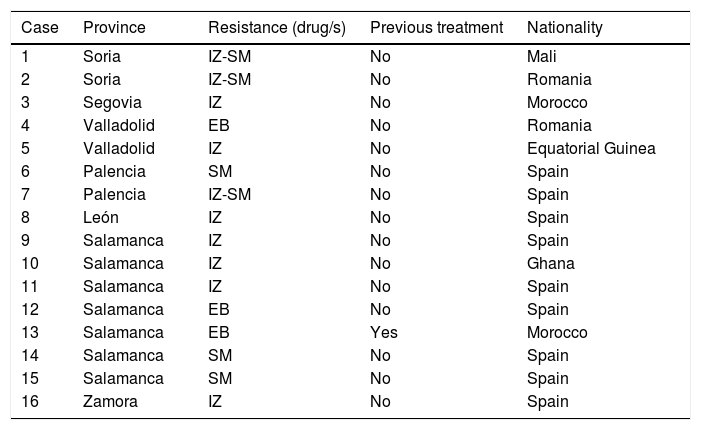
A total of 24 strains were isolated with some type of resistance to anti-TB drugs, eight of which were resistant to pyrazinamide (PZ), all corresponding to Mycobacterium bovis. Sixteen strains of M. tuberculosis (MT) were counted with some type of resistance (5.92%), distributed as follows: seven resistant to isoniazid (IZ); three to ethambutol (EB); three to streptomycin (SM); and three to IZ+SM. No multidrug-resistant strains were detected in this period. Overall resistance to IZ in 2013 was 3.7%. As shown in Table 2, in 15 of the 16 patients with some type of resistance, no previous anti-TB treatment could be proven, making the primary resistance rate 5.5%. In seven of the cases of resistance (43.7%), the patients were immigrants of different origins. The geographical distribution of resistance was fairly uniform throughout the region, with a higher concentration of cases in the province of Salamanca (7 cases), followed by Valladolid, Palencia and Soria (2 cases each). One case each was registered in Segovia, León and Zamora.
Type and geographic distribution of resistance to the anti-TB drugs in Mycobacterium tuberculosis in the Castile-León region in 2013. Nationality is stated in each case.
| Case | Province | Resistance (drug/s) | Previous treatment | Nationality |
|---|---|---|---|---|
| 1 | Soria | IZ-SM | No | Mali |
| 2 | Soria | IZ-SM | No | Romania |
| 3 | Segovia | IZ | No | Morocco |
| 4 | Valladolid | EB | No | Romania |
| 5 | Valladolid | IZ | No | Equatorial Guinea |
| 6 | Palencia | SM | No | Spain |
| 7 | Palencia | IZ-SM | No | Spain |
| 8 | León | IZ | No | Spain |
| 9 | Salamanca | IZ | No | Spain |
| 10 | Salamanca | IZ | No | Ghana |
| 11 | Salamanca | IZ | No | Spain |
| 12 | Salamanca | EB | No | Spain |
| 13 | Salamanca | EB | Yes | Morocco |
| 14 | Salamanca | SM | No | Spain |
| 15 | Salamanca | SM | No | Spain |
| 16 | Zamora | IZ | No | Spain |
EB: ethambutol; IZ: isoniazid; SM: streptomycin.
One of the problems that arises when conducting epidemiological studies on TB is under-reporting. This is evident in our study, where only in a small number of cases was growth of bacilli not documented. A case of special interest is the overall performance of pleural fluid samples, which was very high, with the bacillus being isolated in 2/3 of them. However, in a retrospective study of 17 years carried out in Castile-León in the county of El Bierzo,4 poor performance was found in this type of sample (2.5%). These data seem to indicate that a significant number of cases of pleural TB were not reported in Castile-León. In neighbouring regions, such as Asturias, the percentage of under-reporting of this type of TB was close to 50% in the same period. In contrast, with regard to PTB in Castile-León, there was only a small difference between the two systems in the number of cases, suggesting that notification of this type of TB is better. When the overall TB rates were compared by both data collection systems, hardly any differences were found, although the total figure obtained by culture corresponded to confirmed cases. In other neighbouring regions, again Asturias, through the system for notification of notifiable diseases, TB was found to be under-reported by 27.8%. In this case, the Sistema de Información Microbiológica (SIM) [Microbiological Information System] enabled the recovery of 17.9% of TB cases, with 14.6% being smear-positive.5 Similar results were detected in the neighbouring region of Galicia, where the registering of TB cases is centralised in the tuberculosis units (TBU), allowing better collection of the MD on TB. The proportion attributed to the incomplete declaration of microbiology results is estimated at 29.6% of TB cases in 2013.6
The overall incidence rate for Castile-León was similar to that of the whole of Spain in 2013, and somewhat lower than the European average (13.5 cases/100,000 population/year) obtained in 2012. According to the Centro Nacional de Epidemiología [National Epidemiology Centre] report for 2013, the average incidence rate of TB in Spain was 11.88 cases per 100,000 population per year, so the MD-based registering in this study brings the Castile-León incidence figures closer to the national average for that year. Similar results were obtained in the case of the smear-positive rate. Unlike other regions with higher incidence rates, in Castile-León the immigrant population is smaller and accounted for 15.9% of TB cases during the period studied. In previous studies conducted in the province of León7 in the period 1992–1999, the incidence rates in the León health area were high (38.6%), only exceeded in the region by the El Bierzo health area (44.4%), with the difference attributed to the impact of mining, with a large mass of the services sector employed in coal extraction and slate mining in the area of El Bierzo. With the passing of the years, by 2013 there was a marked decrease in the rates in both areas (of 18% and 30.4%, respectively), but with a greater difference between the two. This difference could be due to the higher incidence of TB in sectors of the population dedicated to mining where, after leaving such activity, they can end up developing TB once they reach a certain age. In 2013, the Spanish region with the highest incidence was Galicia, with 21.8 cases for every 100,000 population per year, and Asturias ranked sixth with 12.13 cases per 100,000 population per year. As these are neighbouring regions with a higher incidence in the case of Galicia, this could also explain the higher incidence rate in the province of León and in the El Bierzo area in particular. In a national study carried out by Jiménez and Casal8 in 2006, and published in 2008, in which data were collected for two months, a primary resistance rate of 8.3% was obtained, with a resistance to IZ of 4.9% and a multi-drug resistance (MDR) rate of 1.3%. In the same period in the autonomous region of Madrid, with a rate of 10.8 cases per 100,000 population, resistance to IZ was 8.2%, with a primary resistance rate of 8%.9 For Castile-León, in previous studies the resistance figures were already low.10,11 In the last of these multicentre studies (2001–2005),12 the primary resistance rate was 4.2%, with resistance to IZ of 3.2% and an MDR rate of 0.1%. By way of comparison, in the neighbouring region of Asturias, the rate of resistance to IZ in the same period was 2.6%, and 4.7% in the Galicia region.
Starting in 2013 and then in 2014 and 2015, new GRUMICALE studies were carried out with the aim of working on improvement and expansion of the data collection system. The first estimates reveal a downward trend in the total number of registered TB cases, reaching a total of 210 in 2015, without large variations in geographical distribution. Such surveillance seems appropriate from the point of view of detecting multidrug-resistant strains or atypical resistance patterns, which appear from time to time and circulate through Castile-León within a general context of low levels of resistance.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: López-Medrano R, Nebreda-Mayoral T, Brezmes-Valdivieso MF, García-de Cruz S, Nogueira-González B, Sánchez-Arroyo R, et al. Contribución de la microbiología al diagnóstico de la tuberculosis en Castilla y León: conclusiones del estudio GRUMICALE 2013. Enferm Infecc Microbiol Clin. 2018;36:152–156.