The objective of this study was to compare the prevalence of human papilloma virus (HPV) in Spanish and foreign women in a cervical cancer screening programme of Castilla y León and foreign women living in the community who participated in the programme.
MethodsThis was an observational, descriptive, cross-sectional, retrospective study of period prevalence.
The sample consisted of all the women included in the cervical cancer prevention programme of the Regional Ministry of Health of the Junta de Castilla y León who were screened for cervical cancer during the period from 2012 to 2014, aged between 25 and 64 years of age.
ResultsOf the 190,203 cervical smear samples collected, 10.2% were foreign (n=19,329). The prevalence of HPV in the foreign women was 23.51%, significantly higher than in the Spanish women (p<.001). The presence of morphological and microbiological changes in the foreign women was also greater.
ConclusionsThis study makes an important contribution, since it comprised a voluminous population screening sample. The prevalence of HPV in the foreign women was significantly higher than in the women born in Spain. It is important to continue studying this type of population, who are difficult to recruit for cultural reasons.
El objetivo propuesto ha sido comparar la prevalencia de virus de papiloma Humano (VPH) en las mujeres españolas y extranjeras pertenecientes al programa de cribado de cáncer de cérvix de Castilla y León, y las mujeres extranjeras residentes en la comunidad que han participado en el programa.
MétodosSe trata de un estudio observacional descriptivo transversal, retrospectivo, de prevalencia de periodo.
La muestra consta de todas las mujeres incluidas en el programa de prevención de cáncer de cérvix de la Consejería de Sanidad de la Junta de Castilla y León a quienes se realizó una prueba de cribado de cáncer de cérvix, durante el periodo de 2012 a 2014, con edades comprendidas entre los 25 y los 64 años de edad.
ResultadosDe las 190.203 muestras de frotis de cérvix recopiladas el 10,2% fueron extranjeras (n=19.329). La prevalencia de VPH en mujeres extranjeras fue del 23,51%, significativamente mayor que en las mujeres españolas (p<0,001). También resultó ser mayor la presencia de alteraciones morfológicas y microbiológicas en las mujeres extranjeras.
ConclusionesEl presente estudio realiza una importante aportación, al tratarse de una voluminosa muestra proveniente de un screening de tipo poblacional. Evidenciando, significativamente, la mayor prevalencia de VPH en mujeres extranjeras que en las mujeres nacidas en España. Siendo importante continuar estudiando este tipo de población que por motivos culturales no es fácil su captación.
Human papilloma virus (HPV) infection is the most common sexually transmitted infection, with it being estimated that at least 50% of the sexually active population may develop it at some point in their lives.1
The prevalence of HPV in the female population ranges between 5 and 10% in developed countries, with figures just above 15% in developing countries.2
The emergence of new HPV vaccines with more genotypes included in their composition, such as the nonavalent vaccine, an adjuvant, non-infectious recombinant vaccine which protects against genotypes 6, 11, 16, 18, 31, 33, 45, 52 and 58, is intended to protect against the types of HPV that cause approximately 90% of cervical cancers,3 and requires a prior analysis of the baseline situation of the population in which the prevention programmes are going to be implemented.
The objective proposed in this study was to compare the prevalence of HPV infection in Spanish and foreign women who form part of the Ministry of Health of the Regional Government of Castile and León's prevention and early detection programme for cervical cancer (PPDCx).
Materials and methodsThis paper concerns an observational, descriptive, cross-sectional, retrospective, period prevalence study.
All women between the ages of 25 and 64, in whom a cervical cancer screening test was performed and who were registered with the Castile and León Health System (at 255 basic health zone centres belonging to the region's 11 health areas) and included in the PPDCx, were enrolled.
The period of study was three years, between 1 January 2012 and 31 December 2014. In this period, 190,203 samples from the cervical smear tests of women taking part in the programme were included.
The PPDCx outlines a screening strategy defining the target population, tests and test intervals, and has an information system which helps to manage the population, the tests and the screening process evaluation.4 The patients were recruited in primary care, where appointments were held to include them in the programme. Based on the results obtained in the screening tests, the date on which the next study was to be carried out was communicated by letter. The target population of the 2012 Programme amounted to 755,843 women. The rate of participation of women aged between 25 and 34 was 30.23%, and for those aged between 35 and 64, 69.77%.4
The Programme's inclusion criteria required the women to be living in Castile and León, to be aged between 25 and 64, to be sexually active and to not have gynaecological symptoms.
Women with a total hysterectomy met the permanent exclusion criterion, while those who were not sexually active or who saw a physician due to gynaecological symptoms met the temporary exclusion criteria.
The screening tests and intervals were performed in:
- •
Women aged 25–34: conventional cervical cytology, every three years (first two cytological studies with a 12-month interval).
- •
Women aged 35–64: conventional cervical cytology and a HPV test, every five years. In women aged 35–64, the screening results were classified as:
- •
Negative (followed programme): if both tests were negative.
- •
Non-deterministic (test repeated at 12 months; if not negative, patients referred to specialist care): Cytology (−) and non-16/18 HR HPV (+)/cytology ASCUS, L-SIL and HPV (−) in menopausal women.
- •
Positive (referred to specialist care): cytology with any morphological alteration and HPV (+/−) in non-menopausal women/cytology ASCUS, L-SIL and HPV (+) in menopausal women/cytology H-SIL and HPV (+/−) in menopausal women/cytology (−) and HPV 16/18 (+).
The conventional cervical cytology results were based on the 2001 Bethesda System classification.4 The cytological specimens were processed based on the Papanicolaou staining technique, allowing them to be observed under a microscope.
The HPV test was carried out by collecting a second endocervical sample using another swab which was kept in a transport medium. HPV infection was detected by means of polymerase chain reaction molecular diagnostic technology using the Clart® HPV2 technique (GENOMICA, SAU).5 This assay includes 35 probes, corresponding to 35 HPV genotypes with a different oncogenic risk (6, 11, 16, 18, 26, 31, 33, 35, 39, 40, 42, 43, 44, 45, 51, 52, 53, 54, 56, 58, 59, 61, 62, 66, 68, 70, 71, 72, 73, 81, 82, 83, 84, 85 and 89).5
The following were included as variables in the study: age of the woman, nationality, geographical area of origin, HPV genotype, HPV genotype risk profile, presence of morphological and microbiological abnormalities in the samples collected.
For data collection, a database was created in Excel. The data were reviewed by the cervical cancer programme. After they had been cleansed, they were analysed using the SPSS v. 15.0 statistics programme.
The level of significance for all the tests was considered to be a p value of ≤0.05. The data were obtained from the Directorate-General of Public Health of the Regional Government of Castile and León's Ministry of Health, who, on opening an administrative channel, proceeded to transfer the data from the file called Programa de prevención de cánceres e infecciones ginecológicas [Prevention programme for cancers and gynaecological infections], which belonged to the Regional Government of Castile and León's Health Promotion Service. The data subject to the request complied with Organic Law 15/1999, of 13 December, on personal data protection.
ResultsA total of 177,377 cervical smear samples were obtained from the PPDCx, for which the women's ages ranged from 25 to 64 years (MA=40, SD±11.35).
89.9% of the smears corresponded to Spanish women (n=159,445) and 10.1% to foreign women (n=17,932).
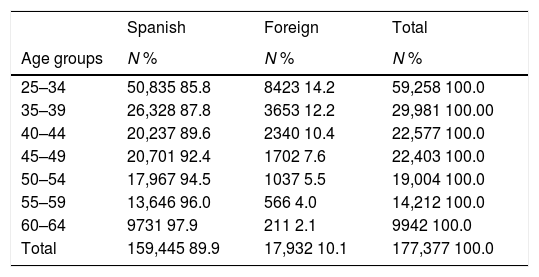
The ages of the Spanish and foreign women included in the PPDCx were studied and compared. It was observed that as the age range increased, foreign women were less represented (Table 1). Thus, in the 25–34 age group, foreign women accounted for 14.2%, while in the 55–59 age group they accounted for 4%.
Age distribution of the Spanish and foreign women included in the PPDCx (2012–2014) of the Regional Government of Castile and León.
| Spanish | Foreign | Total | |
|---|---|---|---|
| Age groups | N % | N % | N % |
| 25–34 | 50,835 85.8 | 8423 14.2 | 59,258 100.0 |
| 35–39 | 26,328 87.8 | 3653 12.2 | 29,981 100.00 |
| 40–44 | 20,237 89.6 | 2340 10.4 | 22,577 100.0 |
| 45–49 | 20,701 92.4 | 1702 7.6 | 22,403 100.0 |
| 50–54 | 17,967 94.5 | 1037 5.5 | 19,004 100.0 |
| 55–59 | 13,646 96.0 | 566 4.0 | 14,212 100.0 |
| 60–64 | 9731 97.9 | 211 2.1 | 9942 100.0 |
| Total | 159,445 89.9 | 17,932 10.1 | 177,377 100.0 |
PPDCx: Castile and León's prevention and early detection programme for cervical cancer.
p<0.001.
A reduction in the percentage of foreign women of approximately 2% was observed for each age range.
For the detection of HPV, 117,774 samples were processed from the 35 to 64 age group. An HPV prevalence of 9.6‰ was obtained (95% CI between 9.48 and 9.82), with genotype 53 being the most common in the programme.
Of the 159,445 cervical smear samples from Spanish women, 108,328 samples were processed in the study for the detection of HPV in Spanish women aged between 35 and 64, with 10,161 HPV-positive samples obtained. Of the 17,932 cervical smear samples from foreign women, 9456 samples were processed for HPV detection in foreign women aged between 35 and 64, from Castile and León, with 1621 HPV-positive samples obtained (p<0.001).
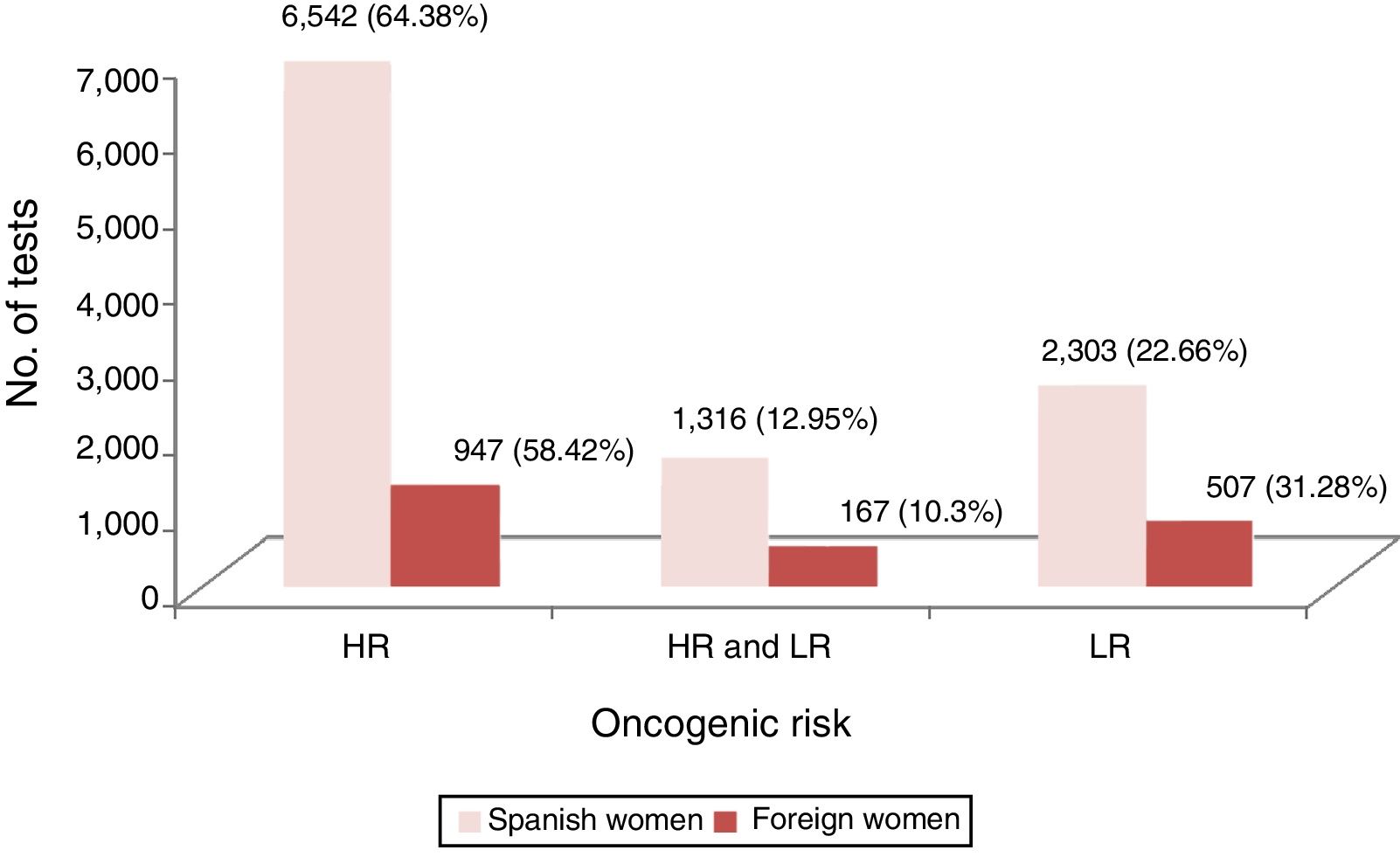
On studying the oncogenic risk profile, we were able to observe that, among foreign women, higher percentages were obtained in the HPV samples positive for low oncogenic risk genotypes than for high oncogenic risk genotypes, with this relationship being reversed in Spanish women (p<0.001) (Fig. 1).
The distribution of genotypes was compared among Spanish and foreign women. It was observed that 15 HPV genotypes had a statistically significant difference in their prevalence (p<0.05), with them being more common in foreign women than in Spanish women.
The genotypes with statistically significant differences (p<0.001) were as follows: HPV 35, with a percentage of 0.41% in Spanish women and 0.84% in foreign women; HPV 58, 0.84% in Spanish women and 1.71% in foreign women; HPV 70, 0.49% in Spanish women and 1.12% in foreign women; HPV 71 0.09% in Spanish women and 0.51% in foreign women; HPV 72, 0.17% in Spanish women and 0.60% in foreign women; HPV 81, 0.32% in Spanish women and 0.91% in foreign women; HPV 83, 0.24% in Spanish women and 1% in foreign women; and HPV 85, 0.02% in Spanish women and 0.27% in foreign women.
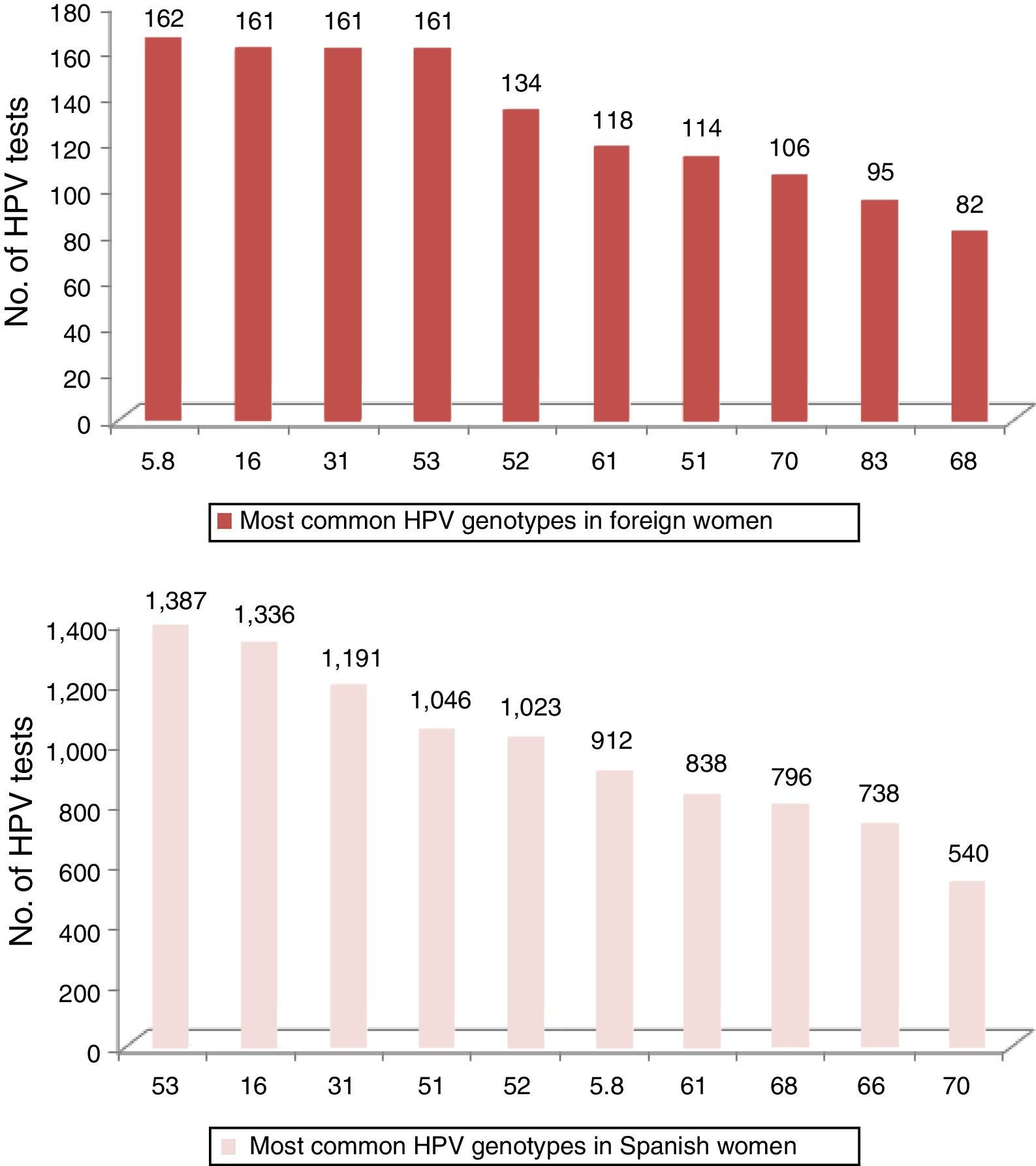
In Fig. 2, the 10 most common HPV genotypes in Spanish and foreign women can be compared.
The results of the study on morphological changes revealed that there were more samples without morphological changes in the Spanish women than the foreign women (66.5% versus 65.3%), just as there were higher rates of vaginal atrophy in the Spanish women compared to the foreign women (10.9% versus 2.7%), as the Spanish women were older.
Cervical cell inflammation was more common in foreign women, being present in 23% versus 15.7% of the samples from Spanish women. Metaplasia was present in 4.6% of the samples from foreign women and in 3.6% of those from Spanish women. The presence of atypical squamous cells of undetermined significance (ASCUS) was more common in foreign women, in 1.8% of samples, while the presence of atypical squamous cells in samples from Spanish women was 1.5%. Low-grade squamous intraepithelial lesions (L-SIL) were also more common in foreign women than in Spanish women, with rates of 0.6% and 0.4%, respectively, as were high-grade squamous intraepithelial lesions (H-SIL) and cancerous lesions, where there was a greater difference, with the percentage tripling, from 0.1% in Spanish women to 0.3% in foreign women, and doubling, from 0.1% to 0.2% in malignant lesions (p<0.001).
DiscussionIn Spain, there are limited data on prevalence from structural population programmes. There are several works published in recent years using population bases which are more or less representative of the population but do not come from structural screening programmes, which are yet to be implemented in many Spanish autonomous regions.
The prevalence of HPV in the female population is a figure which is difficult to determine. The challenge is even greater where the prevalence in foreign women is concerned.
Castile and León is the only autonomous community in Spain with cervical cancer population screening where cytology and HPV detection are performed jointly as a screening test, without the need for a prior pathological finding. This highlights the importance of our study, as it includes both women with and without cytological abnormalities, recruited in a structured manner through the PPDCx.
The results obtained in our study show how foreign women living in the autonomous region of Castile and León have significantly higher prevalence figures than Spanish women, a fact that contrasts with the study published in Italy by Paba et al., whose findings reveal higher rates in Italian women, although these are not significant.6 Another study published by Visioli et al., also in Italy, based on population screening, obtained results showing high-grade cervical lesions to be more common in Italian women than in foreign women; the prevalence of HPV was not studied.7
Mention should also be made of the study carried out by Tornesello et al., who did obtain notably higher prevalences in foreign women, particularly in women from Central and South America,8 in whom high rates are also observed in our study. The study published by González, which reflects very similar prevalences in Spanish and foreign women to those of our study,9 and the study carried out in the city of Valencia by J. López-Olmos,10 should also be mentioned.
The work published by Del Amo shows foreign women to have a high risk HPV, particularly women from South America,11 who had a prevalence that was three times higher than that of Spanish women.
If we detail the HPV genotypes found, we can recall how, in our sample of foreign women living in Spain, the most frequently obtained genotype was HPV 16, as most studies worldwide show.8,12 This was not the case in women from Castile and León. The most prevalent genotype in different European series is genotype 318, 12, which is among the three most common genotypes. It is greater among foreign women than Spanish women.
The absence of genotype 18 amongst the 10 most common genotypes in foreign women in our study should be highlighted.
The difference in prevalence among both groups of women cannot be attributed in this study to the introduction of routine vaccination in our region, since the programme focuses on women aged between 25 and 64, and HPV vaccination in Castile and León began in 2011, in 14-year-old girls. It could be attributed to genetic aspects or race-based susceptibility, which have not been studied in our paper.
ConclusionsThis study provides significant evidence of HPV being more prevalent in foreign women than in women born in Spain. It is very important for more studies to be carried out in the population of foreign women living in Spain.
Limitations of the studyThe main limitation of this study was that the women were not identified, meaning that there may be a small number of cases where several samples belong to the same woman, as well as the voluntary nature of the programme. Even though it was a population programme, some women in the population did not take part in the study.
No economic evaluation has been carried out to affirm the benefit of the programme and the fact that it was not possible to study the socio-economic behaviour of the patients, which may prove to be an influential factor on the study.
AuthorshipS. García Villanueva, M. Domíngez-Gil González, J. Gayete Martínez, J.L. Muñoz Bellido, J.S. Salas Valien, C. Echevarria Iturbe, M. González Sagrado, J.M. Jiménez Pérez, A. Curiel de Arcaute López and S. Rojo Rello took part in designing the study and in the data analysis.
J.M. Eiros Bouza and R. Ortiz de Lejarazu Leonardo took part in drafting the article and in the approval of the final version.
Conflicts of interestThe authors declare that they have no conflicts of interest.
We would like to give thanks to the Health Promotion Service of the Regional Government of Castile and León's Ministry of Health for providing authorisation and access to the data, in particular to Dr. Pedro Ángel Redondo Cerdeña and Dr. María Mercedes Sánchez Jacob, who facilitated the entire process.
Please cite this article as: García-Villanueva S, Domínguez-Gil González M, Gayete Martínez J, Muñoz Bellido JL, Salas Valien JS, Echevarria Iturbe C, et al. Estudio comparativo de la prevalencia de virus de papiloma humano en las mujeres españolas y extranjeras, participantes en un programa de cribado poblacional en Castilla y León. Enferm Infecc Microbiol Clin. 2019;37:314–318.