Acute respiratory infections are one of the main causes of morbidity in children.1 In recent years, thanks to progress with molecular diagnostics technologies, new viruses implicated in these infections have been described, one being the human metapneumovirus (hMPV).2
Although it causes 6–14% of respiratory tract infection admissions in children,3,4 less often than the main causes of hospitalisation (RSV, parainfluenza), up to 20% of these viral infections in children have been attributed to it.5,6
There are few papers that evaluate the epidemiology of hMPV infection in our area, therefore in this scientific letter, we wish to highlight different epidemiological, clinical, diagnostic and therapeutic aspects among the hospitalised children in whom hMPV infection has been demonstrated, and to present the differences encountered between infections in infants under the age of 2 years and older children. This cut-off point was chosen under a hypothesis of greater obstructive symptomatology and severity in infants versus older children.7,8
In a retrospective study conducted in our hospital between April 2009 and May 2014, 192 cases of hMPV isolated in nasopharyngeal aspirates were included, corresponding to 190 patients between the ages of 0 and 14 years (in 2 patients, hMPV was isolated in 2 admissions in different years). All the samples were sent to the hospital laboratory's virology department in viral transport media (VTM), and they were studied using direct immunofluorescence with specific monoclonal antibodies (D3 Duet® DFA RSV/Respiratory Virus Screening Kit, Diagnostic Hybrids).
Patients under the age of 2 accounted for 77.6% of the cases. Of the patients in our series, 10.4% presented an underlying condition (neurological, heart, oncological, prematurity), with no statistically significant differences between the two groups (<2 years 7%; >2 years 11.6%; p=0.542). Eight point nine percent (8.9%) of the patients required admission to the intensive care unit, again with no differences between the two groups (<2 years 10.1%; >2 years 4.7%; p=0.370). One patient died with a congenital cytomegalovirus infection and respiratory exacerbation in the context of the infection.
The under-2 patients more frequently presented cough, rhinitis, apnoea and difficulty breathing, with statistically significant differences found (p<0.001); meanwhile those over 2 more frequently presented seizures and fever (p=0.005). There were 20 patients in whom other germs were simultaneously isolated in the nasopharyngeal aspirate. The isolated germs were H. influenzae (n=10), M. catarrhalis (n=4), S. aureus (n=2), P. aeruginosa (n=2), Candida (n=1) and Parainfluenza 3 (n=1). No statistically significant differences were found between the two groups.
Regarding supplementary tests, more laboratory tests were performed in the over 2 group (82.1% vs. 58.2%; p=0.006), as well as more chest X-rays (81.4% vs. 59.1%; p=0.007). There were no differences in the infection marker levels (C-reactive protein and procalcitonin) or white blood cells. Differences were found in the presence of parenchymal consolidations on X-rays, which were more common in the older group (65.7% vs. 40.9%; p=0.013).
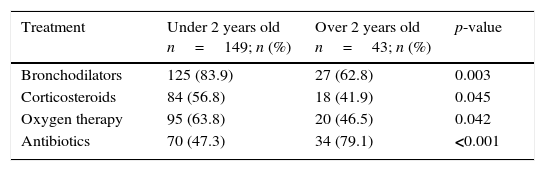
The differences in treatment are shown in Table 1.
This study provides data based on a broad patient sample that exclusively corresponds to children under 14. With the hypothesis that there is greater obstructive symptomatology and severity from hMPV infection in infants,7,8 it was decided to divide the sample into patients over and under 2 years of age. It was found that the latter had greater lower tract involvement and, therefore, a higher need for corticosteroid bronchodilator treatment and oxygen therapy.9
Contrary to what was expected, it was observed that more supplementary tests were used in the older patients, which may be explained by more underlying conditions and fever symptoms.9 Moreover, by presenting more parenchymal condensations, we assume a higher use of antibiotic therapy, despite there being no differences in the infection parameters, supporting the viral origin.
Performing direct immunofluorescence enables a definitive diagnosis to be reached in under 24h, however, there is no rapid diagnostic test as used in other infections, such as those caused by the flu virus or group A streptococcus, that enable decisions to be made in the emergency department or at the time of admission to the hospital. If such tests existed, they could decrease the use of diagnostic techniques and unnecessary treatments, as we have seen happen.
Admission to the intensive care unit was required for a significant number of patients in both groups, therefore hMPV should be considered in the aetiological diagnosis of respiratory infections in patients requiring admission to the hospital.
Please cite this article as: Montaner Ramón A, Martínez Faci C, Martínez de Zabarte Fernández JM, Ros Arnal I. Características de la infección por metapneumovirus humano, ¿es importante la edad?. Enferm Infecc Microbiol Clin. 2017;35:59–60.