Cardiac complications in dengue patients are not uncommon and are not diagnosed, since they are usually mild and self-limiting.
ObjectivesTo characterize the cardiovascular manifestations in hospitalized patients with dengue infection.
MethodsWe conducted an observational, analytical, longitudinal, prospective epidemiological study, which included 427 patients treated at Manuel Fajardo Clinical-Surgical Teaching Hospital with diagnosis of dengue infection since April 2017 to April 2018.
ResultsCardiovascular manifestations (19.7%), mainly heart rate disorders (sinus bradycardia [13.8%], atrial [4.9%] and ventricular [4.0%] extrasystoles) were frequent in dengue infection patients. Pericarditis and myocarditis were diagnosed in 1.6% and 0.2% respectively. These disorders were self-limiting in 83.3% of cases and occurred in the first days of the onset of fever in 75.0%. Advanced age (OR=1.70), male sex (OR=1.94), decreased platelet count (OR=1.13) and dengue with warning signs (OR=3.29) were related to a higher probability of presenting cardiovascular disorders in the course of a dengue infection.
ConclusionsCardiovascular manifestations in dengue patients are frequent, and are related to advanced age, male sex, as well as severe forms of the disease.
Las complicaciones cardiacas en pacientes con dengue no son infrecuentes y no son diagnosticadas, ya que usualmente son leves y autolimitadas.
ObjetivosCaracterizar las manifestaciones cardiovasculares en pacientes hospitalizados con infección por dengue.
MétodosSe realizó un estudio epidemiológico observacional, analítico, de corte longitudinal, prospectivo, que incluyó 427 pacientes atendidos en el Hospital Docente Clínico-Quirúrgico Comandante Manuel Fajardo con diagnóstico de infección por dengue durante el periodo comprendido desde abril de 2017 hasta abril de 2018.
ResultadosLas manifestaciones cardiovasculares (19,7%), principalmente los trastornos del ritmo (bradicardia sinusal [13,8%], extrasístoles auriculares [4,9%] y ventriculares [4,0%]) fueron frecuentes en pacientes con infección por dengue. La pericarditis y miocarditis se identificó en el 1,6% y 0,2%, respectivamente. Estas manifestaciones fueron autolimitadas en el 83,3% y se presentaron en los primeros días de inicio del cuadro febril en el 75,0%. La edad avanzada (OR=1,70), el sexo masculino (OR=1,94), el recuento de plaquetas disminuido (OR=1,13) y el dengue con signos de alarma (OR=3,29) se relacionaron con una mayor probabilidad de presentar manifestaciones cardiovasculares en el curso de una infección por dengue.
ConclusionesLas manifestaciones cardiovasculares en pacientes con dengue son frecuentes, y se relacionan con la edad avanzada, el sexo masculino, así como las formas severas de la enfermedad.
Dengue has the highest rates of morbidity and mortality of any arthropod-borne viral disease in the world.1 In recent decades, the Americas have recorded the most drastic increase in dengue activity, in particular in Brazil, Colombia, Ecuador, Peru, Venezuela and Paraguay,2 with an incidence in this region for 2019 of 289.8 cases per 105 inhabitants.3 In Cuba, dengue outbreaks have come to occur closer and closer together and involve larger numbers of people, with an incidence of 0.6–22.5 cases per 105 inhabitants from 2009 to 2019.3
Cardiac compromise in dengue was first reported in 1943 by Hyman, in American soldiers fighting in the South Pacific during World War II.4 However, a great deal remains unknown about this disease, and articles in the global literature on the subject are scarce.
Cardiac signs include arrhythmias (relative bradycardia, transient first- and second-degree atrioventricular block, atrial and ventricular extrasystoles, and/or isolated episodes of tachyarrhythmias such as atrial fibrillation) and other electrocardiographic findings such as T wave inversion and ST segment depression, as well as pericarditis, pericardial effusion and, far less commonly, variable degrees of myocardial dysfunction which may lead to pulmonary oedema, cardiogenic shock or severe myocarditis.1
The incidence of cardiac impairment in the general population with dengue infection reported in articles is highly variable, ranging from 11.4% to 62.5%,5–7 whereas in China, the reported incidence of myocarditis is up to 11.3%.8 Bradyarrhythmias are the most common rhythm disorders. They are self-limiting and generally asymptomatic (relative bradycardia in infectious diseases).7 These disorders may be due to autonomic system abnormalities, abnormalities in Ca2+ storage in infected cells, direct viral invasion of myocytes or cytokine-mediated immune damage, leading to myocardial oedema or subclinical myocarditis.9
Cardiovascular signs, their prevalence and their characterisation, linked to viral diseases, specifically dengue, have never been studied in Cuba. They are only seen in the literature in the form of isolated case reports.10 Despite the low frequency reported in international studies, the consequences of these signs for the patient's prognosis and chances of sequelae are significant. For this reason, it was decided to conduct this study, with the objective of characterising cardiovascular signs in patients hospitalised with dengue infection.
MethodsStudy population and study typeAn observational, analytical, longitudinal, prospective epidemiological study was conducted that enrolled patients over 18 years of age with classic symptoms of dengue infection and detection of positive IgM on the sixth day of febrile signs and symptoms, having been diagnosed with dengue infection between 1 April 2017 and 30 April 2018 and being treated at Hospital Docente Clínico-Quirúrgico Manuel Fajardo [Manuel Fajardo Medical–Surgical Teaching Hospital] in Plaza, a municipality of Havana. Patients with underlying cardiovascular disease (hypertensive cardiomyopathy, ischaemic cardiomyopathy or non-infectious heart valve disease) were excluded.
Of 1,083 individuals cared for during the study period, 427 patients who met the inclusion criteria and none of the exclusion criteria for the study were enrolled. A total of 656 patients were excluded as follows: 301 patients whose medical record lacked a routine electrocardiogram; 206 patients who had incomplete data in their medical record; 109 patients with a diagnosis of hypertensive cardiomyopathy; 27 patients with a history of ischaemic cardiomyopathy; and 13 patients with a diagnosis of non-infectious heart valve disease. Electrocardiogram records were taken from the patients' first day of admission to their discharge.
Sociodemographic variables (age, sex and skin colour), clinical variables (onset and duration of cardiovascular signs [including rhythm disorders, repolarisation disorders, pericarditis, pericardial effusion and myocarditis] and dengue classification) and laboratory values (haemoglobin, haematocrit, leukocyte count and platelet count) were included. The dengue classification of the World Health Organization (WHO) was used.11
Cardiovascular signsThe following rhythm disorders were included: sinus bradycardia, atrioventricular block, atrial and/or ventricular extrasystoles, atrial fibrillation, atrial flutter and ventricular tachycardia. Repolarisation disorders were defined as the presence of T wave inversion or flattening and/or ST segment depression ≥0.5mV in at least two contiguous leads. Pericarditis was diagnosed in the presence of the following characteristics: 1) precordial pain typical of pericarditis; 2) pericardial friction rub; 3) widespread ST segment depression, accompanied or not accompanied by PR segment depression. Pericardial effusion was defined as the presence of an echolucent area in the pericardial space reported in the echocardiogram. Myocarditis was diagnosed in a context of clinical suspicion in a patient with no cardiovascular history when dilated cardiomyopathy or ventricular systolic dysfunction was detected by echocardiogram.
Statistical analysisQualitative variables are expressed in terms of absolute values and percentages. Quantitative variables are expressed in terms of mean and standard deviation. To identify potential difference between the variables included in the study and the presence or absence of cardiovascular signs, the chi-squared test was used. The level of statistical significance was set for p values <0.05. In addition, relative risk (RR) was calculated with a 95% confidence interval. The SPSS version 21.0 statistical software package (Chicago, Inc. United States) was used.
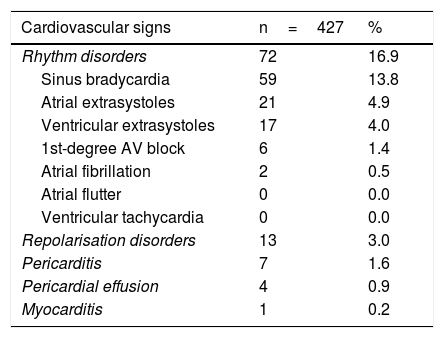
ResultsOf a total of 427 enrolled patients, cardiovascular signs were detected in 84 patients, corresponding to a frequency of 19.7%. The main electrocardiographic signs found were rhythm disorders (16.9%). Of these, the most common disorders were sinus bradycardia, followed by atrial and ventricular extrasystoles. Table 1 lists other less common electrocardiographic findings.
Distribution of patients by type and by time of onset and duration of cardiovascular signs.
| Cardiovascular signs | n=427 | % |
|---|---|---|
| Rhythm disorders | 72 | 16.9 |
| Sinus bradycardia | 59 | 13.8 |
| Atrial extrasystoles | 21 | 4.9 |
| Ventricular extrasystoles | 17 | 4.0 |
| 1st-degree AV block | 6 | 1.4 |
| Atrial fibrillation | 2 | 0.5 |
| Atrial flutter | 0 | 0.0 |
| Ventricular tachycardia | 0 | 0.0 |
| Repolarisation disorders | 13 | 3.0 |
| Pericarditis | 7 | 1.6 |
| Pericardial effusion | 4 | 0.9 |
| Myocarditis | 1 | 0.2 |
| Time of onset | n=84 | % |
|---|---|---|
| <7 days | 63 | 75.0 |
| 7−30 days | 17 | 20.2 |
| >30 days | 4 | 4.8 |
| Duration | n=84 | % |
|---|---|---|
| <24h | 21 | 25.0 |
| 24−72h | 49 | 58.3 |
| >72h | 14 | 16.7 |
Pericarditis was diagnosed in seven patients (1.9%), and pericardial effusion was identified in four patients (0.6%); all cases were mild in severity and resolved spontaneously with rest, analgesics and colchicine in two cases.
In 75.0% of cases, the cardiovascular signs detected started within seven days of the onset of symptoms, while in 58.3% of patients the cardiovascular signs lasted 24−72h (Table 1).
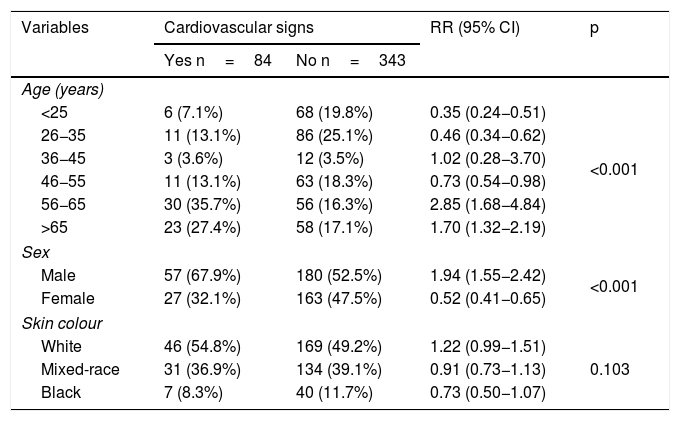
The group with cardiovascular signs had a significantly higher percentage of patients 56−65 years of age (RR=2.85) and patients over 65 years of age (RR=1.70) compared to those without cardiovascular compromise. In addition, the percentage of male patients was significantly higher in the group with cardiovascular signs (RR=1.94). On the other hand, skin colour showed no significant relationship (Table 2).
Distribution of patients by age, sex, skin colour and presence or absence of cardiovascular signs.
| Variables | Cardiovascular signs | RR (95% CI) | p | |
|---|---|---|---|---|
| Yes n=84 | No n=343 | |||
| Age (years) | ||||
| <25 | 6 (7.1%) | 68 (19.8%) | 0.35 (0.24−0.51) | <0.001 |
| 26−35 | 11 (13.1%) | 86 (25.1%) | 0.46 (0.34−0.62) | |
| 36−45 | 3 (3.6%) | 12 (3.5%) | 1.02 (0.28−3.70) | |
| 46−55 | 11 (13.1%) | 63 (18.3%) | 0.73 (0.54−0.98) | |
| 56−65 | 30 (35.7%) | 56 (16.3%) | 2.85 (1.68−4.84) | |
| >65 | 23 (27.4%) | 58 (17.1%) | 1.70 (1.32−2.19) | |
| Sex | ||||
| Male | 57 (67.9%) | 180 (52.5%) | 1.94 (1.55−2.42) | <0.001 |
| Female | 27 (32.1%) | 163 (47.5%) | 0.52 (0.41−0.65) | |
| Skin colour | ||||
| White | 46 (54.8%) | 169 (49.2%) | 1.22 (0.99−1.51) | 0.103 |
| Mixed-race | 31 (36.9%) | 134 (39.1%) | 0.91 (0.73−1.13) | |
| Black | 7 (8.3%) | 40 (11.7%) | 0.73 (0.50−1.07) | |
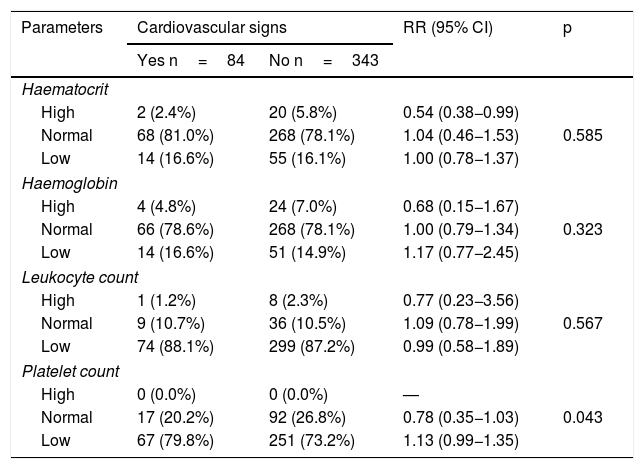
Regarding laboratory parameters, only low platelet count was significantly higher in the group with cardiovascular signs (79.8% versus 73.2%); the relative risk of presenting these signs was 1.13 times higher in patients with a decreased platelet count (p=0.043) (Table 3).
Distribution of patients by haematological parameters and presence or absence of cardiovascular signs.
| Parameters | Cardiovascular signs | RR (95% CI) | p | |
|---|---|---|---|---|
| Yes n=84 | No n=343 | |||
| Haematocrit | ||||
| High | 2 (2.4%) | 20 (5.8%) | 0.54 (0.38−0.99) | 0.585 |
| Normal | 68 (81.0%) | 268 (78.1%) | 1.04 (0.46−1.53) | |
| Low | 14 (16.6%) | 55 (16.1%) | 1.00 (0.78−1.37) | |
| Haemoglobin | ||||
| High | 4 (4.8%) | 24 (7.0%) | 0.68 (0.15−1.67) | 0.323 |
| Normal | 66 (78.6%) | 268 (78.1%) | 1.00 (0.79−1.34) | |
| Low | 14 (16.6%) | 51 (14.9%) | 1.17 (0.77−2.45) | |
| Leukocyte count | ||||
| High | 1 (1.2%) | 8 (2.3%) | 0.77 (0.23−3.56) | 0.567 |
| Normal | 9 (10.7%) | 36 (10.5%) | 1.09 (0.78−1.99) | |
| Low | 74 (88.1%) | 299 (87.2%) | 0.99 (0.58−1.89) | |
| Platelet count | ||||
| High | 0 (0.0%) | 0 (0.0%) | — | 0.043 |
| Normal | 17 (20.2%) | 92 (26.8%) | 0.78 (0.35−1.03) | |
| Low | 67 (79.8%) | 251 (73.2%) | 1.13 (0.99−1.35) | |
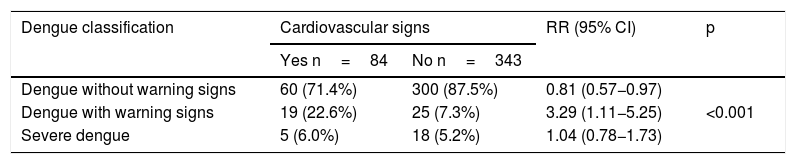
Moreover, the percentage of patients who had dengue with warning signs was significantly higher in the group with cardiovascular signs (22.6% versus 7.3%), with a 3.29 times higher relative risk (p<0.001) (Table 4).
Distribution of patients by disease severity and presence or absence of cardiovascular signs.
| Dengue classification | Cardiovascular signs | RR (95% CI) | p | |
|---|---|---|---|---|
| Yes n=84 | No n=343 | |||
| Dengue without warning signs | 60 (71.4%) | 300 (87.5%) | 0.81 (0.57−0.97) | <0.001 |
| Dengue with warning signs | 19 (22.6%) | 25 (7.3%) | 3.29 (1.11−5.25) | |
| Severe dengue | 5 (6.0%) | 18 (5.2%) | 1.04 (0.78−1.73) | |
In this study, approximately one-fifth of patients had cardiovascular signs during dengue infection. These primarily consisted of electrocardiographic abnormalities related to rhythm disorders. By contrast, structural cardiac abnormalities such as pericarditis and pericardial effusion were less common, and functional abnormalities such as myocarditis had a low incidence.
The frequency of electrocardiographic abnormalities in patients with dengue infection was confirmed in a study by Yadav and Kumar,12 in which the incidence of electrocardiographic signs was 27.0%. Among them, the most common were sinus bradycardia and T wave inversion, with 9.6% each, while ST segment depression was found in 8.7%. For their part, Arora and Patil,13 in India, reported that 36.7% of their patients had cardiovascular signs, essentially sinus bradycardia (8.8%), as well as repolarisation disorders (3.5%) and first-degree atrioventricular block (also 3.5%).
The pericardium was also seen to be affected by dengue, but with a lower frequency than the myocardium, with very few reports of isolated pericarditis due to dengue.13 However, pericardial effusions are seen occasionally, especially in severe dengue, and are likely related to the severity of capillary plasma leakage.
In this study, patients with dengue and warning signs had a 3.29 higher likelihood of having some sort of cardiovascular sign. A decreased platelet count was also linked to a higher rate of onset of such signs. Similarly, in the study by Papalkar et al.14, conducted in India, it was shown that a platelet count below 100,000/mm3 and a high haematocrit were associated with a 4.31 and 3.43 times higher likelihood, respectively, of cardiovascular signs. Meanwhile, in a case series, Kularatne et al.,7 divided patients into two groups — cardiac and non-cardiac — based on the presence or absence of ECG abnormalities (T wave inversion, ST segment depression or bundle branch block). ECG changes were seen in 62.5% of patients in the cardiac group, who were more prone to fatigue, dyspnoea, low peripheral oxygen saturation (p=0.001), chest pain (p=0.001) and skin redness (p=0.05) compared to patients with normal electrocardiograms (non-cardiac group). This points to a higher likelihood of cardiovascular signs in patients with more severe infection. Other recent studies13,15,16 have also demonstrated a higher likelihood of cardiovascular signs in patients with warning signs and severe dengue.
It has also been reported that myocardial dysfunction is more severe in patients with dengue shock syndrome compared to those with classic dengue or dengue haemorrhagic fever without shock.17,18 Similarly, in the study by Arora and Patil,13 electrocardiographic signs were more common in patients with dengue haemorrhagic fever or dengue shock syndrome, though the differences were not significant.
The effects of ageing (≥65 years of age) on cardiac impairment were not studied, but elderly patients with dengue were more likely to be hospitalised and to have a worse prognosis than younger patients.19 Consequently, more careful evaluation and follow-up might be called for in patients over 65 years of age, owing to the higher frequency of comorbidities (such as hypertension, diabetes mellitus and ischaemic cardiomyopathy) in this group. In fact, in this study, older age, specifically the 55–65 age group, was significantly linked to a higher likelihood of cardiovascular signs.
This study found that the cardiovascular signs identified, which largely consisted of rhythm disorders, were self-limiting and most often presented within a few days of the onset of febrile signs and symptoms. Similarly, most studies conducted in these patients with cardiovascular signs11,13,20,21 reported a higher frequency of presentation within five days of the onset of febrile signs and symptoms, lasting no longer than a week.
It is concluded that cardiovascular signs in patients with dengue are common and self-limiting, with a higher likelihood of occurrence in patients of advanced age, male patients and patients with severe forms of the disease. It is important to take these findings into account not only in endemic regions, but also in European countries (such as Spain) where cases of autochthonous dengue have already been reported.22
As limitations of the study, it is important to note that echocardiography was not routinely indicated in all patients with dengue infection. It was only indicated in those with some sort of cardiovascular symptoms and/or specific electrocardiographic abnormality. This might have led to underestimation of cases with an asymptomatic course of pericarditis or myocarditis, though this is uncommon.
In addition, it would have been ideal to have data on specific cardiac markers, as well as data from MRI scans or endomyocardial biopsies for more definitive diagnosis in cases with dengue infection and suspected myocarditis. However, these data are not available at the centre.
Conflicts of interestNone.
Please cite this article as: Cabrera-Rego JO, Rojas-Quiroz AF, Vidal-Turruelles Y, Yanes-Quintana AA. Manifestaciones cardiovasculares en pacientes hospitalizados con dengue. Enferm Infecc Microbiol Clin. 2021;39:115–118.