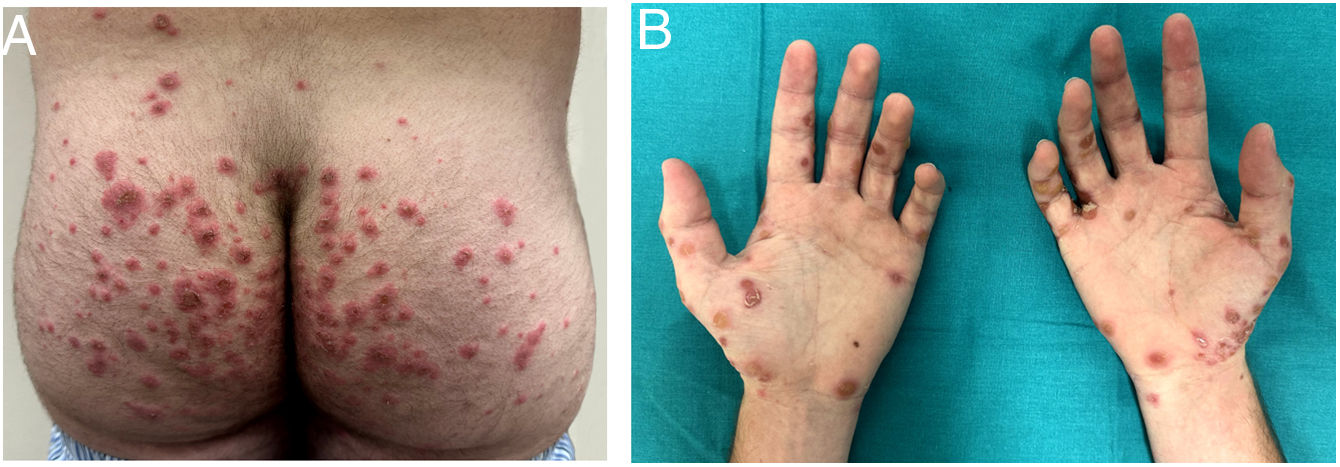
A 20-year-old man presented with a 1-month history of pruritus in trunk and extremities. Pruritus was recalcitrant to oral antihistamines and worsened during night. Since the last ten days, the patient had developed painful plaques in hands, abdomen, buttocks, and thighs. Physical examination revealed atypical bullous plaques in upper extremities, predominantly in dorsal side of hands and palms, buttocks, and proximal lower extremities (Fig. 1A, B). These plaques were formed by a central bulla and a peripheral purple-brown circle. Moreover, the patient had eroded nodules in scrotum, penis, and abdomen. There were not lesions in oral mucosa. The patient denied starting any new drugs or having any recent infectious diseases. In a similar matter, the patient denied any systemic clinic.
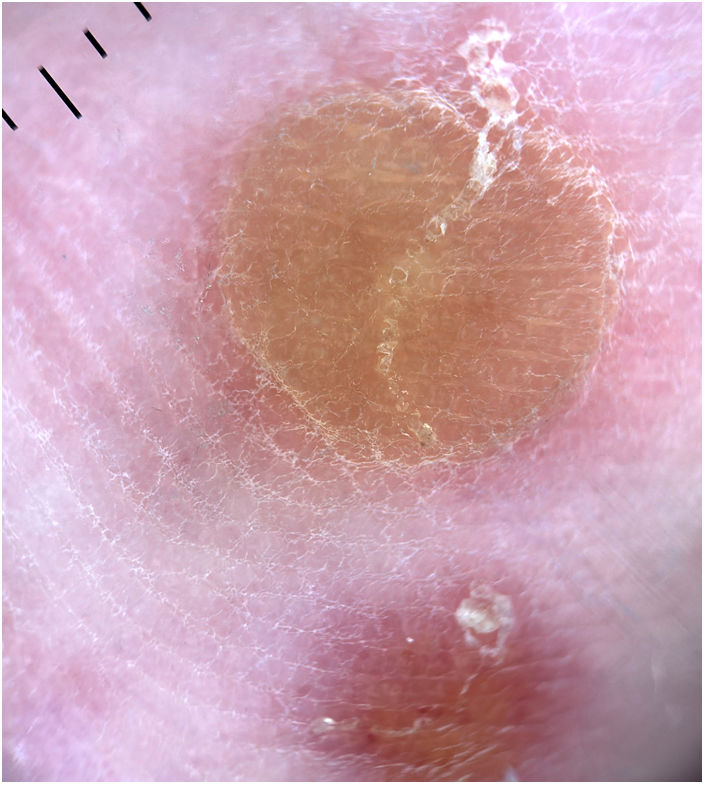
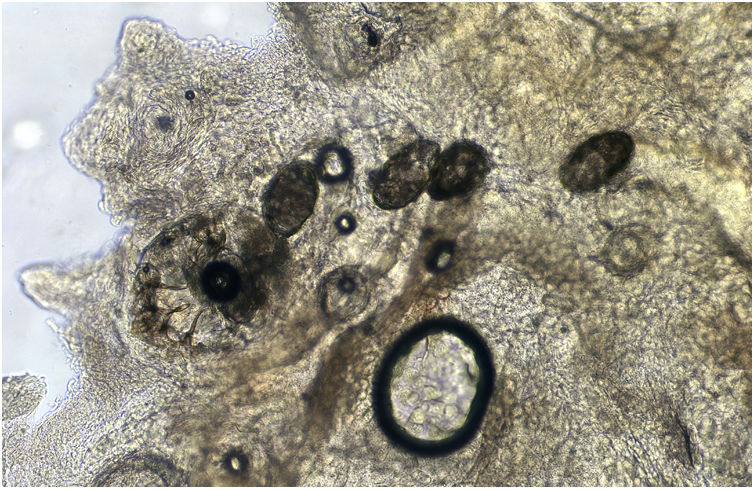
Diagnosis and evolutionAt first impression, we considered diseases that might present with painful bullae in palms, as well as, pruritic plaques widespread. Closed examination by dermoscopy of a bullous plaque revealed a reddish macule with a central bulla filled with clear liquid. Some bullae showed a central or peripheric furrow with a brown triangular end (Fig. 2). A skin scraping from the ceiling of a bulla showed a Sarcoptes scabeii mite and eggs, following a furrow-like distribution (Fig. 3). Thus, given the clinical presentation, the patient was diagnosed with bullous scabies infestation. The patient was treated with oral ivermectin and a short course of oral corticosteroids. We recommended hygiene measures and treatment of close-contact partners as well.
Human scabies is a neglected global disease caused by Sarcoptes scabiei var. hominis mite.1 Classic scabies is characterized by erythematous papules, burrows and generalized pruritus that tends to worse at nights.1 However, several rare scabies variants, such as crusted, nodular, bullous and nail scabies, have been described.1 On the other hand, cutaneous adverse reaction to antiscabies treatment, including irritant and allergic contact dermatitis, have also been reported.2 Target erythema multiforme-like lesions have been reported in a case of irritant contact dermatitis due to 5% permethrin cream for treatment of scabies infestation.2
Mechanisms of blister formation in bullous scabies are not completely elucidated. Superinfection, friction due to pruritus, eczema, direct injury from lytic enzymes of scabies mites or cross-reactivity of scabies protein with basal membrane zone antigens have been proposed as possible explanations.3 Despite the clinical variants, pruritus is still the dominant symptom of scabies.1 Given the current trend of increasing incidence of scabies, when facing patients with recalcitrant pruritus, a high suspicious of atypical presentations should prompt searching for clinical and dermoscopy signs of scabies.
AuthorshipAll authors had access to the data and played a role in writing this manuscript.
We confirm that this manuscript contains original, unpublished work that is not being considered for publication elsewhere at the same time.
Informed consentThe patient in this manuscript has given written informed consent to publication of his case details.
FundingThis article has no funding source.
Conflicts of interestNone of the authors have any conflicts of interest to declare.