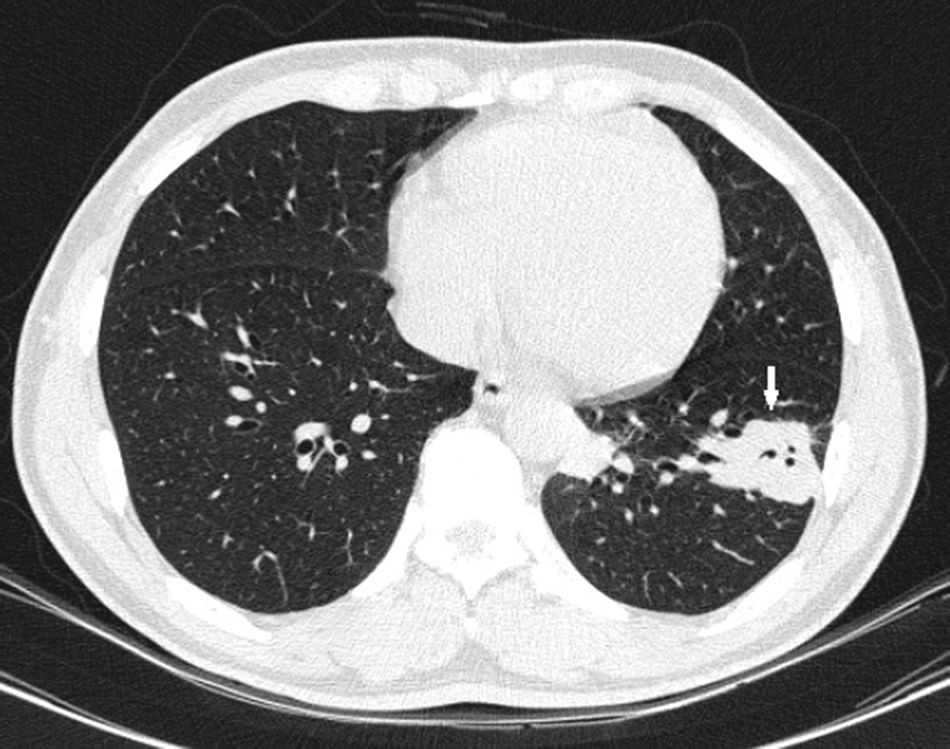
A 45-year-old Colombian male patient, resident of the rural area of southern Colombia (Department of Huila), working in agriculture, with no relevant previous medical history and no known travel abroad, consulted with a two-month history of intermittent left-sided chest pain, of mild-to-moderate intensity, associated with occasional dry cough. The symptoms had worsened in the previous week, with intensification of the pain and unquantified fever. On physical examination, the patient was afebrile, with no evidence of significant abnormalities in the general examination. No abnormalities were found on chest X-ray. In view of the persistence of the patient's pain, a simple and contrasted chest computed tomography (CT) scan was performed, which showed nodular opacity of diffuse distribution in the left lower lobe (Fig. 1).
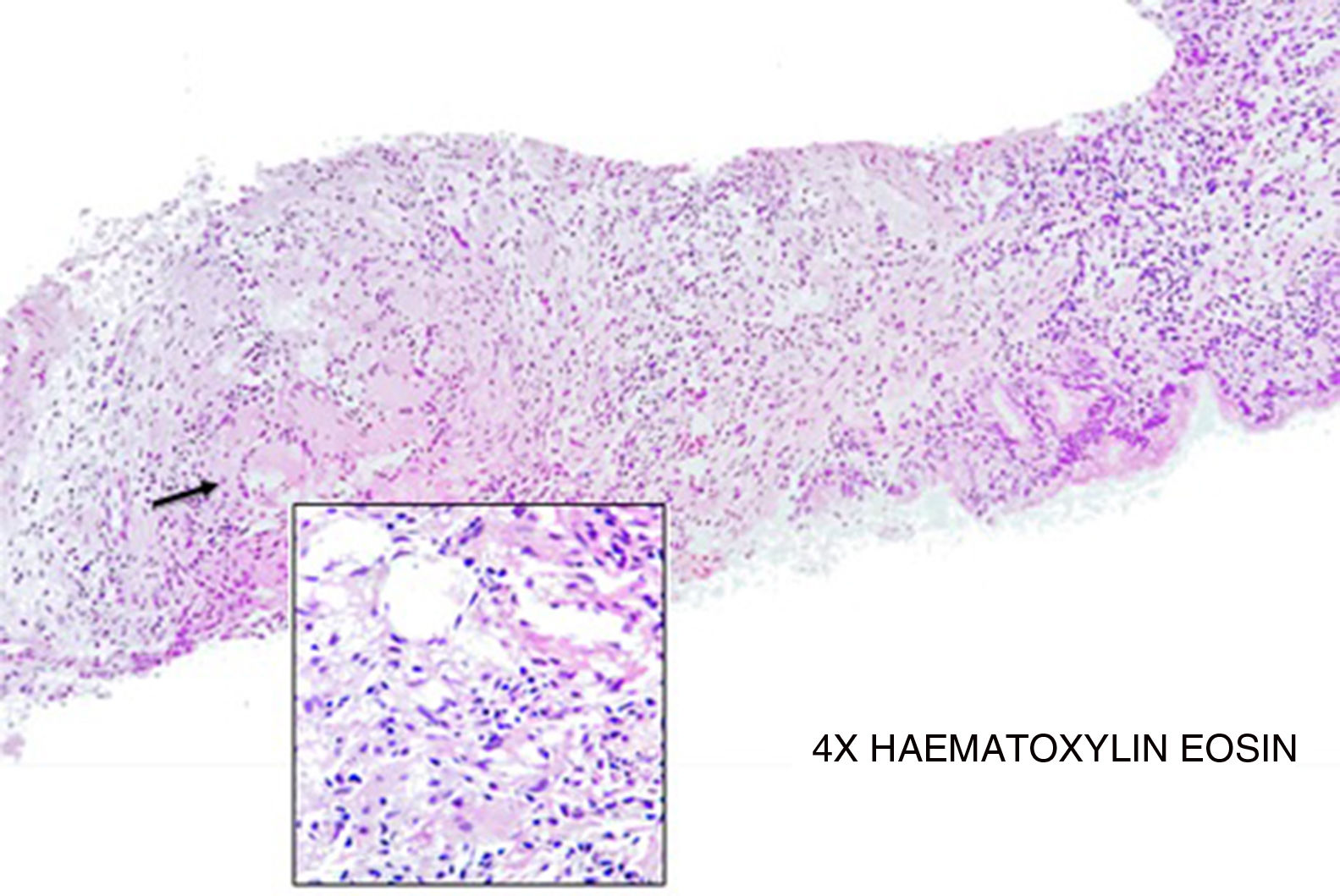
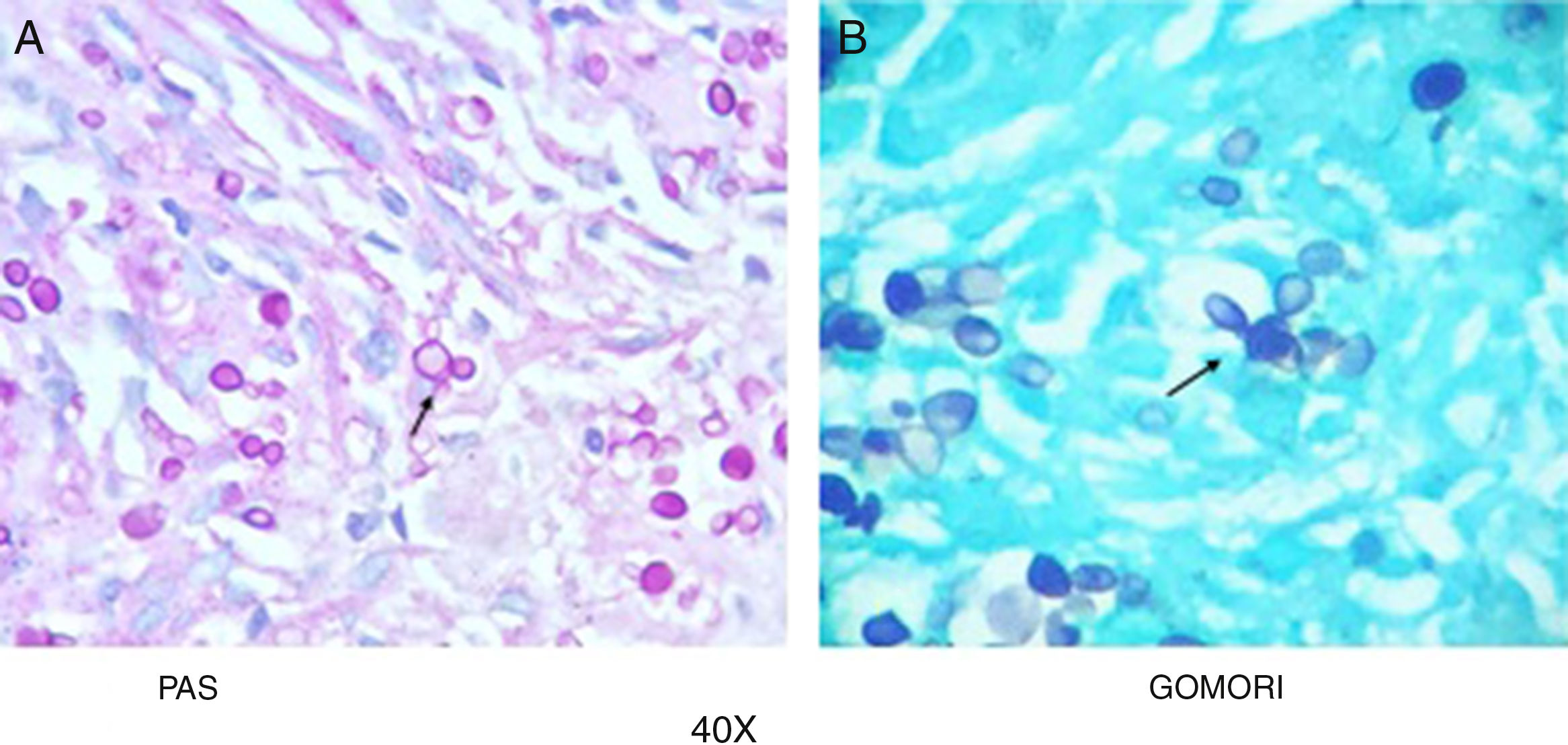
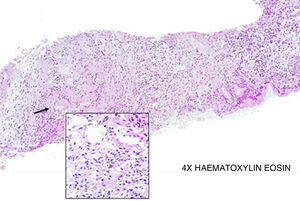
Clinical courseIn view of the CT findings, fiberoptic bronchoscopy with lavage (BAL) and bronchoalveolar aspiration (BAS) was performed, with no macroscopic evidence of abnormalities; samples were sent for mycobacterial culture, KOH and bacterial culture. No transbronchial biopsies were taken. The bacterial and mycobacterial cultures were negative. The KOH from the BAL was positive for yeast, so the interventional radiology team were asked to obtain an ultrasound-guided biopsy. The pathology report stated lymphohistiocytic inflammatory infiltrate with presence of giant cells and formation of granulomas (Fig. 2). In the PAS (Fig. 3A) and methenamine silver staining (Gomori, Fig. 3B) there are abundant yeast cells with multiple budding (in “ship's wheel” pattern) compatible with Paracoccidioides sp. The Ziehl–Neelsen stain was negative. HIV serology and immunoglobulin study were performed to rule out immunodeficiencies, with all being normal. With the above, we made the diagnosis of pulmonary paracoccidioidomycosis.
Paracoccidioidomycosis is a chronic granulomatous infectious disease caused by the fungus Paracoccidioides brasiliensis.1 It is a common disease in Latin America, with multiple cases found primarily in Brazil. In Europe, cases are usually imported due to the large migratory flow of people from countries where the infection is endemic.
The microorganism is acquired by inhalation of aerosols or through direct contact with skin lesions. Only 2% of infected patients develop symptoms typical of the disease,2 mostly patients with a certain degree of susceptibility to these types of microorganisms (smokers, patients with immunosuppression, chronic alcoholism, etc.).
With regard to clinical presentation, chronic forms, mainly located in lung tissue, tend to be the most common in adults (90% of cases), but it can spread to oropharyngeal mucosa and lymph nodes, particularly in immunosuppressed patients.3
Itraconazole is the treatment of choice for paracoccidioidomycosis (mainly in deep infections, such as those with pulmonary involvement), although there are other less effective treatment options, such as amphotericin B and co-trimoxazole.4
FundingThe study did not receive any type of funding.
Conflicts of interestThe authors declare that they have no conflicts of interest with respect to the writing of this manuscript.
Please cite this article as: Gómez-Cerquera JM, Monroy-Tovar L, Silva-Morera C, Salinas-Cortés DF. Una extraña causa de dolor torácico. Enferm Infecc Microbiol Clin. 2019;37:203–204.