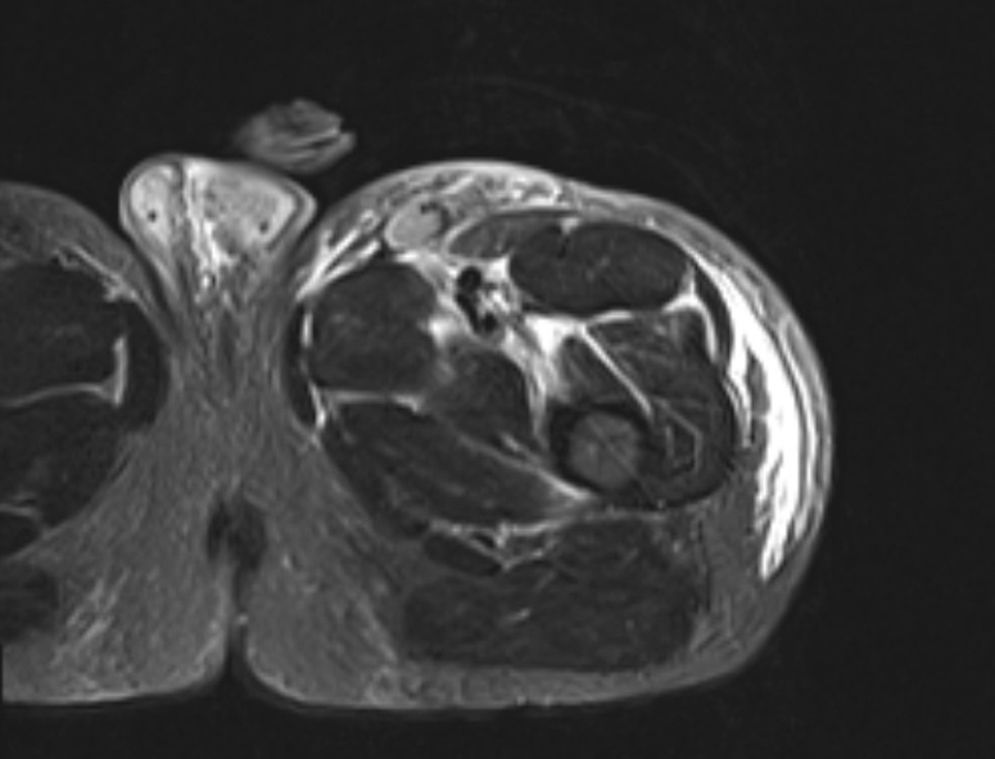
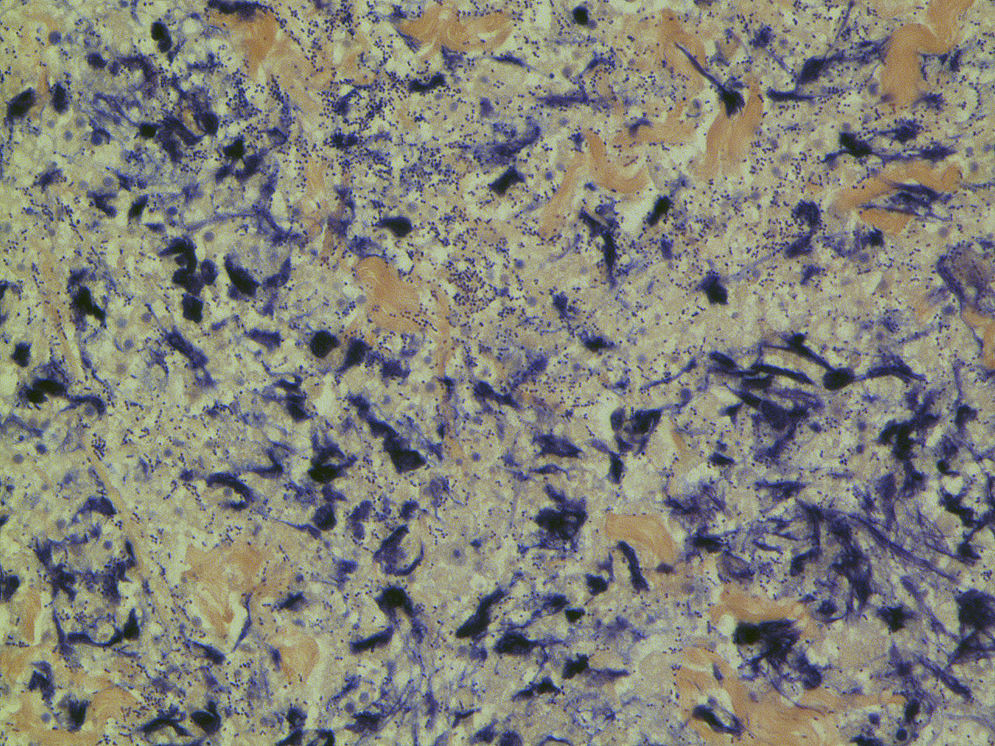
A 27-year-old Ecuadorian male who arrived in Spain three weeks earlier to attend a family celebration visited our hospital due to painful swelling of his left foot for the past two days (he attributed this to the use of compressive footwear) plus, in recent hours, a 38°C fever. A physical examination revealed: temperature 35°C, blood pressure 94/53mmHg, heart rate 111bpm and respiratory rate 30breaths per minute. It also revealed serosanguineous exudate at the lateral malleolus of the left foot. Samples were taken for bacteriological culture and two blood cultures. Laboratory testing results included: glucose 107mg/dl, GOT 54IU/l, GPT 143IU/l, CRP 3.30mg/dl and leukocytes 25,000ml−1 (neutrophils 92.3%). The patient was admitted to the intensive care unit with a diagnosis of sepsis of cutaneous origin. Treatment was started with linezolid, amikacin, meropenem, analgesics and intravenous (IV) fluids. One day later, the patient developed livedo reticularis on the dorsum of his left foot (Fig. 1). Consequently, an interdisciplinary consultation with the dermatology department was requested. Tinea pedis was suspected, and a sample was taken from the sole of his foot for fungal culture. The patient was transferred to another centre for magnetic resonance imaging. This showed interfascial oedema between the muscle bellies that comprise the quadriceps muscle, the tensor fasciae latae muscle and the femoral vascular bundle (Fig. 2), as well as in the popliteal fossa, plus an isolated focus of myositis. As these images were consistent with necrotising fasciitis, a fasciotomy was performed in which a corrugated rubber drain was placed with apical fixation in the anterior compartment of the left thigh, medial compartment of the left leg and dorsum of the left foot. Samples for pathology and microbiology studies were taken during surgery. The pathology study confirmed a diagnosis of necrotising fasciitis, showing coccoid forms with diffuse tissue infiltration and a relative lack of leukocytes (Fig. 3). Streptococcus pyogenes (S. pyogenes) was isolated in the samples from the lateral malleolus as well as the samples biopsied from soft tissue. Blood cultures were negative. Trichophyton mentagrophytes grew in the sample obtained for fungal culture. Given the microbiological findings, the patient's antibiotic treatment was modified and a regimen with IV penicillin+IV linezolid was established. IV human immunoglobulin was administered, then stopped after three days due to poor tolerance. No further surgical procedures were needed. The patient followed a good clinical course and was discharged from the hospital 16 days after he had been admitted.
We present the case of a pyogenic superinfection (S. pyogenes) on top of a pre-existing lesion (Tinea pedis), which ended up causing a necrotising infection of the deep fascia. Our case shows that necrotising fasciitis may occur in cases of minor alterations of the mucocutaneous barrier,1 like those originating in infections with dermatophytes, and is not uncommon in cases of closed trauma. Trauma increases expression of vimentin, thereby promoting adhesion of S. pyogenes to muscle cells.2 Clinical presentation is non-specific, and often the clinical entity suspected on admission is not the one that is ultimately diagnosed. This is particularly important because surgery, the most important part of treatment, should not be delayed by more than 12–24h.3 Wong et al. developed a tool for calculating the risk of necrotising fasciitis based on various laboratory variables.4 On this scale, our patient had a score of 1 (low risk of necrotising fasciitis). The fact that both linezolid and immunoglobulin were used might explain why our patient followed a favourable clinical course which required no further fasciotomies, as is usually the case. In cases of serious S. pyogenes infection, a combination of penicillin and clindamycin should be administered intravenously; however, the development of new treatments against Gram-positive bacteria raises the possibility of using these in cases of serious infection by this type of microorganism,5 including necrotising fasciitis.
Please cite this article as: Lopez-Alonso B, Irigoyen-von-Sierakowski A, Beltran-Rosel A. Dolor y tumefacción del pie izquierdo en varón ecuatoriano de 27 años. Enferm Infecc Microbiol Clin. 2018;36:523–524.