The aim of this study was to evaluate a cut-off point of the titration of IgG by ELISA in the diagnosis of mumps.
MethodsA study was made of serum samples from 85 mumps cases (confirmed by PCR in saliva) and 2351 controls of the general population of the Region of Madrid.
ResultsThe IgM detection was positive in 21 cases (sensitivity of 24.7%). The best cut-off point corresponded to IgG titres≥4900 (sensitivity of 64.7% and specificity of 86.1%). Among 42 patients immunised with at least one dose of measles mumps, rubella vaccine IgM was detected in 4 cases. However, the detection of IgG≥4900 was positive in 29 (sensitivity of 69.0%).
ConclusionsAn IgG result of ≥4900 was almost 5 times more probable in a patient with mumps than in a non-infected patient. The detection of high titres of IgG against mumps could improve the IgM results in vaccinated people.
El objetivo del estudio fue determinar un punto de corte de la titulación de IgG mediante ELISA en el diagnóstico de parotiditis.
MétodosSe estudiaron sueros de 85 casos de parotiditis (confirmados por PCR en saliva) y de 2.351 controles de la población de la Comunidad de Madrid.
ResultadosLa detección de IgM fue positiva en 21 casos (sensibilidad del 24,7). El mejor punto de corte de IgG correspondía a títulos ≥4.900 (sensibilidad del 64,7% y especificidad del 86,1%). De 42 pacientes vacunados con ≥1 dosis de triple vírica se detectó IgM en 4, mientras que la detección de IgG ≥4.900 fue positiva en 29 (sensibilidad del 69,0%).
ConclusionesUn resultado de IgG ≥4.900 fue casi 5 veces más probable en un paciente con parotiditis que en otro sujeto no infectado. La detección de títulos elevados de IgG frente a parotiditis puede mejorar el rendimiento diagnóstico de la IgM en vacunados.
Since routine immunisation with the triple vaccine for the measles, mumps and rubella (MMR) viruses was introduced in Spain, vaccination coverage has improved.1 However, despite that, there continue to be outbreaks of mumps, especially among young adults.2 The use of vaccines with low immunogenicity, such as the one that included the Rubini strain, has been suggested as a possible cause.3 However, the administration of two doses of vaccine with strains considered more immunogenic, such as Jeryl Lynn, does not guarantee total protection.3 Re-infection by the mumps virus is not a rare phenomenon. Vaccination failures in young adults4 may, in part, be caused by the decrease in the level of protective antibodies over time.5
The clinical definition of mumps provided in the Red Nacional de Vigilancia Epidemiológica [National Epidemiological Surveillance Network] protocol refers to any person with fever and at least one of the following signs: sudden onset of swelling of the parotid (or other salivary) glands and/or orchitis.6 Confirmation criteria include: positive IgM or seroconversion of IgG; or nucleic acid detection or isolation of the virus in saliva, urine or cerebrospinal fluid.6 Culture is very laborious and has fallen into disuse. The identification of viral RNA by reverse transcription-polymerase chain reaction (RT-PCR), is considered the procedure of choice.7 However, the sensitivity of RT-PCR decreases with the time since onset of symptoms.8
In previously vaccinated subjects, the infection can cause a secondary immune response with absence of IgM7 and high IgG titres.9 For that reason, it has been proposed that in cases with negative IgM, the presence of high titres of IgG in a sample of serum extracted very close to the onset of symptoms could be useful.6 However, the concept of “high IgG titres” needs to be defined for specific methods (because of the variability between ELISA techniques) and in epidemiological contexts, delimited in time and place. The aim of this study was to evaluate the cut-off point for IgG quantification using an ELISA technique in the diagnosis of mumps.
MethodsAs the reference population, we used a group of 85 cases (age range: 2–58 years; mean: 23.8; standard deviation: 9.6; 50 males) of mumps infection confirmed by identification of viral RNA in saliva by RT-PCR. In all the cases, the qualitative serological determination of IgM and the titration of IgG specific to the virus were performed by ELISA (Enzygnost, Siemens, Germany). IgG titration was calculated using a standardised one-step procedure (alpha method). The technique's range of IgG values corresponded to titres of 230–8000. Negative sera were assigned an arbitrary titre of 115. Samples with titres greater than 8000 were considered as 16,000. The serum samples were taken at the same time as the saliva samples within 0–8 days of the onset of symptoms (mean: 2.7; standard deviation: 2.2). All samples from the cases were obtained between January 2013 and August 2016 in the Autonomous Region of Madrid. When it was possible to obtain information regarding the immune status of the cases, the number of doses and the type of MMR vaccine administered were evaluated.
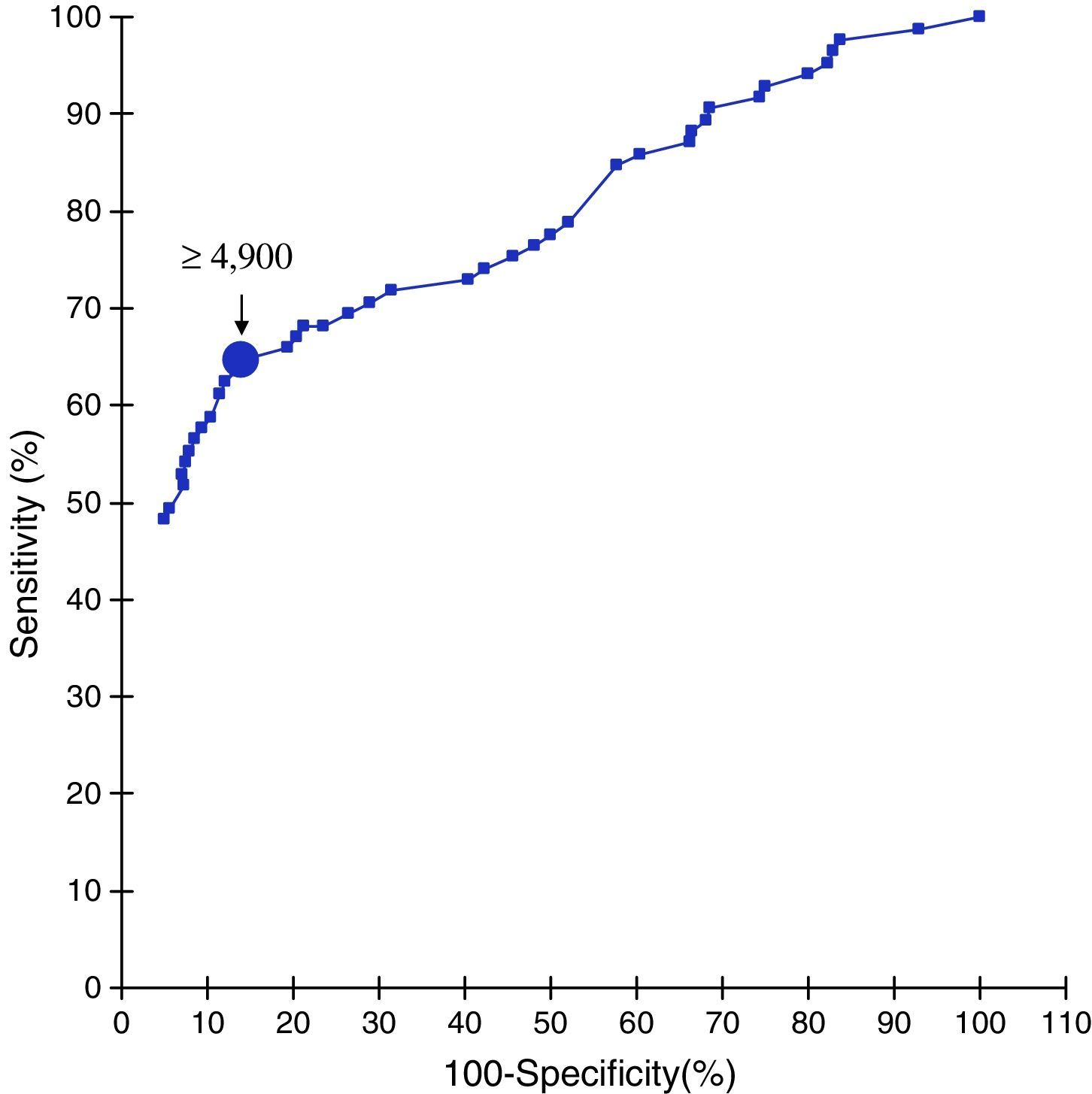
As the reference population, we used a group of 2351 individuals representative of the population of the Autonomous Region of Madrid (age range: 2–60 years; mean: 21.1; standard deviation: 15.3; 1204 males). Serum samples for this group were obtained within the framework of the Autonomous Region of Madrid's Fifth Sero-surveillance Survey from January to July 2015. IgG titres against mumps virus were determined using the same technique as for the cases. The levels of sensitivity and specificity were calculated for different IgG titres, and were represented by receiver operating characteristic (ROC) curves. In order to estimate the probability of obtaining a specific IgG result (positive or negative), according to the presence or absence of disease and in relation to the best cut-off point identified by the ROC curve, we determined the positive coefficient of probability and the negative coefficient of probability of the diagnostic technique.
ResultsThe age of the cases (range: 2–58 years; mean: 23.8; standard deviation: 9.6) was comparable to that of the controls (range: 2–60 years; mean: 21.1; standard deviation: 15.3).
The detection of specific IgM was positive in 21 cases (sensitivity of 24.7%; 95% CI: 16.3–35.5). ROC curve analysis (Fig. 1) showed that the cut-off point for IgG that provided the greatest sensitivity and specificity (largest area under the curve) was titres ≥4900 ([55 of 85 cases] sensitivity of 64.7%; 50% CI: 53.5–74.6 and [2025 of 2351 controls] specificity of 86.1%; 95% CI: 84.7–87.5). The positive and negative coefficients of probability for this cut-off point were 4.7 and 0.4, respectively. In 47 of the 64 PCR-positive but IgM-negative cases (73.4%; 50% CI: 60.7–83.3) specific IgG titres ≥4900 were detected.
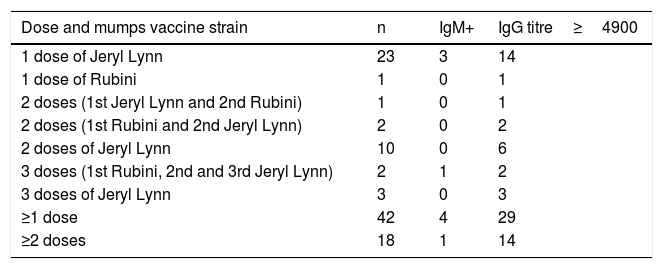
In 42 cases, a history of vaccination status was available. The distribution of serological results according to their vaccination status is shown in Table 1. IgM was only found in four of the 42 patients immunised with ≥1 dose of MMR vaccine. However, IgM was positive in 17 of the 43 patients with no documented vaccination (p<0.01). IgG titres ≥4900 were detected in 29 of the 42 patients with ≥1 dose (sensitivity of 69.0%; 95% CI: 52.8–81.9) and 26 of the 43 patients with no known history of vaccination (sensitivity of 60.5%; 95% CI: 44.4–74.6). IgM was detected in one of the 18 patients with ≥2 doses, while IgG titres ≥4900 were found in 14 (sensitivity of 77.8%; 95% CI: 51.9–92.6).
Distribution of serological results according to immunisation history with MMR vaccine.
| Dose and mumps vaccine strain | n | IgM+ | IgG titre≥4900 |
|---|---|---|---|
| 1 dose of Jeryl Lynn | 23 | 3 | 14 |
| 1 dose of Rubini | 1 | 0 | 1 |
| 2 doses (1st Jeryl Lynn and 2nd Rubini) | 1 | 0 | 1 |
| 2 doses (1st Rubini and 2nd Jeryl Lynn) | 2 | 0 | 2 |
| 2 doses of Jeryl Lynn | 10 | 0 | 6 |
| 3 doses (1st Rubini, 2nd and 3rd Jeryl Lynn) | 2 | 1 | 2 |
| 3 doses of Jeryl Lynn | 3 | 0 | 3 |
| ≥1 dose | 42 | 4 | 29 |
| ≥2 doses | 18 | 1 | 14 |
The presence of non-protective antibodies in vaccinated individuals hinders the serological diagnosis of mumps. Detection of IgM is considered a marker of acute infection. However, the sensitivity of this test in vaccinated patients is poor.7,8 Serological confirmation can be obtained from seroconversion.10 However, that confirmation is hampered by the difficulty in obtaining a second serum sample. Considering that the cases with vaccine failure are characterised by a secondary immune response with high IgG levels, the IgG titre can add a certain degree of value to the diagnosis.9 Although in this study information on vaccine status was only available in 42 cases, it is possible that, in view of the high level of coverage of the MMR vaccine in our environment,1 and the emergence of previous epidemic waves,2 many patients could have been exposed to virus antigens beforehand. The detection of elevated levels of IgG supports clinical suspicion, and should be interpreted in terms of “serological result suggestive of mumps”. This information can be important for monitoring the circulation of the virus, and thus adopting the relevant public health measures, especially in population centres which are not completely protected, and when molecular diagnostic procedures are not available. In this study, a positive coefficient of probability of 4.7 was obtained with the cut-off point established. This indicates that an IgG result ≥4900 is almost five times more likely in a patient with mumps than in another non-infected subject. Almost three-quarters of the patients infected with the mumps virus, but with negative IgM results, had IgG titres above this cut-off point. The results of this study indicate that, in our environment and especially in the context of outbreaks, the detection of high titres of anti-mumps IgG with the serological technique used can improve the performance of IgM, maintaining acceptable levels of specificity. At present, unlike with measles, rubella or varicella, there are no international units of measurement for the quantification of anti-mumps IgG that allow good inter-comparability between serological techniques. What we need are comparative studies, both inter-laboratory and between different serological procedures, in order to examine both the specificity of IgM detection (and not only its sensitivity) and the diagnostic performance of anti-mumps IgG quantification.
Conflicts of interestThe authors declare that they have no conflicts of interest.
To Mariluz Álvarez, Isabel Vadillo and Marisa Fernández for their excellent technical assistance. The study was partially funded by the ISCIII PI12/02006 project.
Please cite this article as: Sanz JC, Ramos B, Fernández A, García-Comas L, Echevarría JE, de Ory F. Diagnóstico serológico de parotiditis epidémica: valor de la titulación de IgG específica. Enferm Infecc Microbiol Clin. 2018;36:172–174.