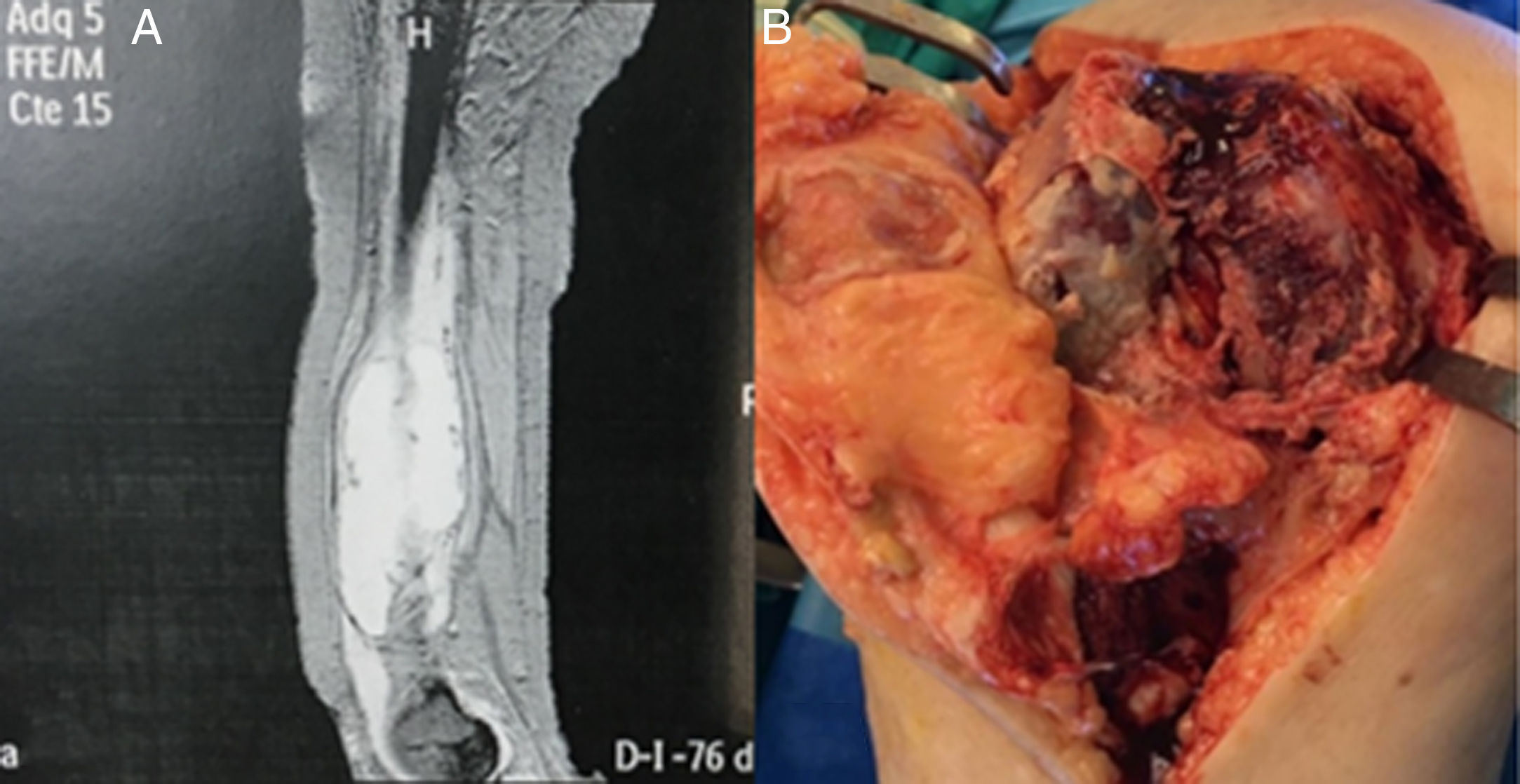
A 63-year-old patient who went to the Emergency Department for severe pain in the right thigh. She had no fever, flu-like syndrome, or weight loss. The blood tests were normal. Haematoma was observed in the crura due to fibrillar rupture with extension to the mid-thigh. After a month, the patient went to the emergency department due to pain and sudden locking of the right knee. Given the persistence of the symptoms, she was assessed by the Traumatology Department and a bone scintigraphy study and SPECT-CT scan of the knee were performed. The images show an acute knee joint effusion. A haematoma was observed, without apparent resolution for five months. The CT scan showed the presence of a collection attached to the femur, without solid structures inside (Fig. 1A).
OutcomesThe patient was admitted to search for the cause of the chronification. The blood tests revealed slight leukocytosis and a mild elevation of acute phase reactants (CRP: 0.94mg/dl), without any other anomaly. Debridement of the abscess and arthrolysis of the affected knee was performed (Fig. 1B), showing the release of a purulent material, which was sent to the Microbiology Laboratory. After nine days, the patient was discharged with a regimen of levofloxacin and rifampin, pending the microbiological results.
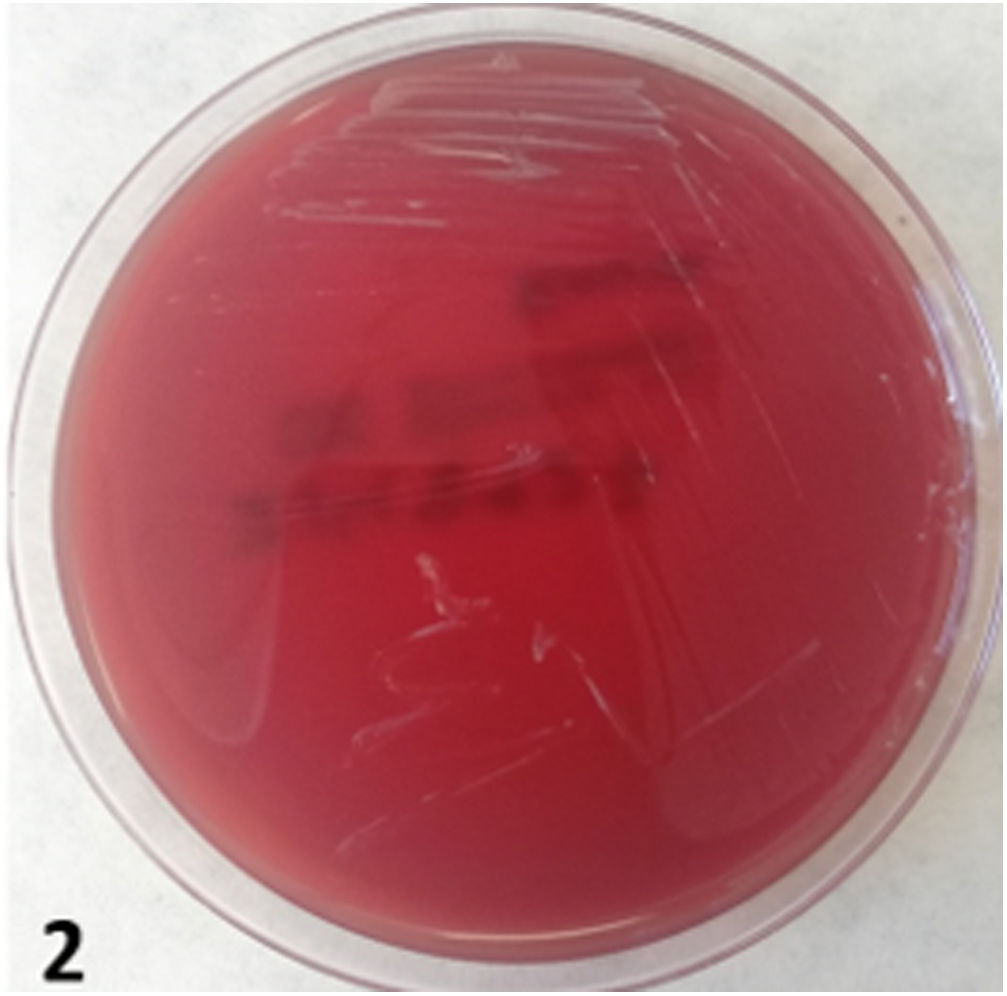
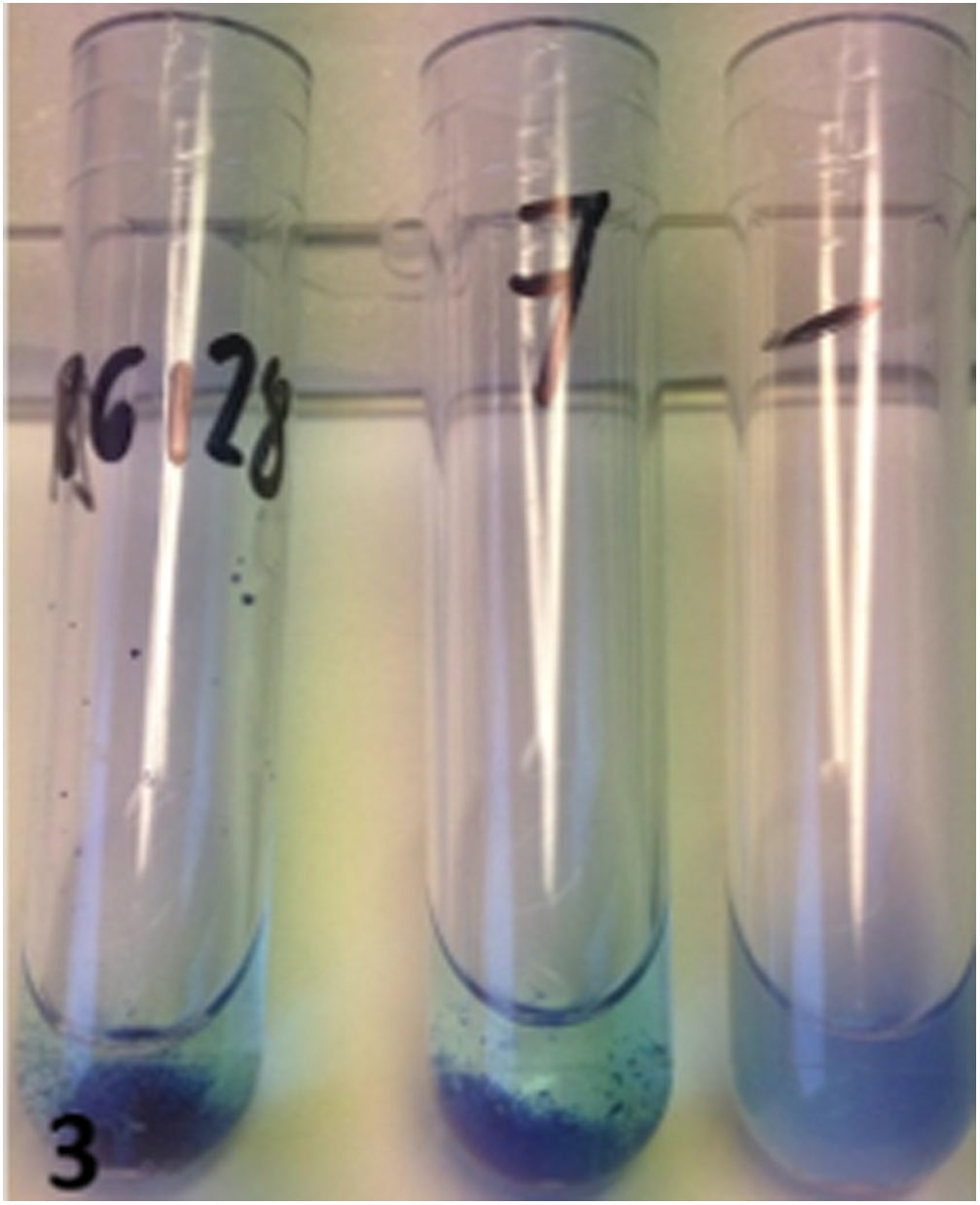
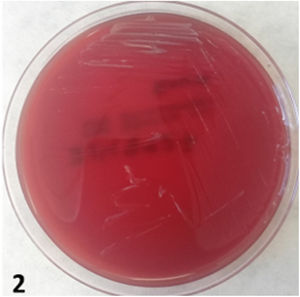
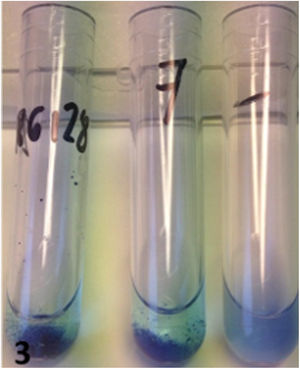
A bacteriological, mycological and mycobacterial culture was performed in the usual media. In the Gram stain, abundant leukocytes of mononuclear origin and absence of microorganisms were observed. PCR of Mycobacterium spp. was negative. Due to the peculiarity of the case, the incubation time was prolonged. After 15 days, the growth of a greyish-looking colony was observed (Fig. 2). The Gram stain showed gram-variable coccobacilli. The catalase, oxidase and urease tests were strongly positive. In light of the suspicion of Brucella spp., she was referred to isolation in a reference centre for identification. The result of the Maldi-Tof Vitek MS was Brucella spp., with a confidence level of 99.9%. To complete the case, the Rose Bengal, tube agglutination and Coombs serological tests were performed, the latter only being positive with a titre of 1/1280 (Fig. 3). The isolate showed sensitivity to rifampin, doxycycline, aminoglycosides and fluoroquinolones. The final diagnosis was chronic septic arthritis due to Brucella spp. Treatment was adjusted to doxycycline 100mg/12h and rifampin 600mg/24h. Clinical follow-up of the patient showed reports of improvement and disappearance of pain.
CommentsThe genus Brucella is made up of small, immobile, gram-negative coccobacilli that act as slow-growing facultative intracellular pathogens. It produces zoonoses by ingestion or direct contact with infected animals or their fluids.1 It requires a low infectious dose for its transmission and shows that it can be easily transmitted by aerosols. For this reason, it has been classified as a Category B bioterrorism agent by the United States CDC.2–4
Brucellosis is a multisystemic disease that covers a wide clinical spectrum, characterised by high fever that manifests itself cyclically. However, in most cases, the acute phase is subclinical and tends to be chronic, producing complications such as arthritis, osteomyelitis, endocarditis and a wide range of symptoms that could be confused with other nosological entities.5 Lack of epidemiological history, difficult isolation in culture, asymptomatic infections, and chronic infections with atypical symptoms are common causes of underdiagnosis.6,7
Its isolation in clinical samples is considered a definitive diagnosis, limited by its low profitability and long growth time. The MALDI-TOF technique has shown good results for the identification of Brucella spp., from plate cultures or blood cultures.8 PCR is a fast and safe alternative, since it allows non-viable bacteria to be worked with.9 Serology provides a presumptive diagnosis; however, the main drawback is cross-reactions and, in chronic infections, false negatives.10 In our case, only the Coombs test was positive, given the chronic nature of the infection.
The patient was diagnosed with septic arthritis in the context of chronic brucellosis. The therapeutic approach was adequate, after identification of the microorganism. In Spain, cases of brucellosis unrelated to occupational exposure continue to be registered, despite health controls. That is why, in endemic areas, this entity should be taken into account in patients with nonspecific symptoms and without an epidemiological history.
Please cite this article as: Corrales I, Oro-Camps J, García-Aguayo JM, Palomar-Schopf M. Artritis séptica: a propósito de un caso. Enferm Infecc Microbiol Clin. 2020;38:289–290.