A 72-year-old woman undergoing haemodialysis through a central jugular venous catheter, presented arterial hypotension during a dialysis session (80/40 mmHg), fever (38.4 °C) and shivering, for which she was admitted to our centre. In her history, a left nephrectomy performed nine months earlier for papillary renal cell carcinoma type 1 with locoregional invasion (TNM pT2aN0M0) stood out.
In our assessment, we observed a patient in poor general condition, obtunded, eupnoeic at rest, with an O2 saturation of 97%, arterial hypotension that went up after serum therapy, arrhythmia, slight bibasal crackles and mild oedema in the lower limbs. There were no signs of inflammation in the area where the central venous catheter was implanted. Laboratory tests revealed normochromic normocytic anaemia and thrombocytopenia, both new, as well as leukocytes 7.87 × 109/l, TnI 3880 ng/l, NT-proNBP 242,000 pg/ml, CRP 245 mg/l and procalcitonin 46 ng/ml. The electrocardiogram showed de novo atrial fibrillation. In order to find the origin of the sepsis, a CT scan of the chest and abdomen was performed, revealing a moderate pericardial effusion, right prevascular and paratracheal adenopathies, and bilateral ground-glass pulmonary infiltrate. Given the results of the previous tests, anticoagulation was started with heparin at therapeutic doses and empirical antibiotic therapy with meropenem and vancomycin, removing the jugular central venous catheter and channelling a femoral venous line. Methicillin-sensitive Staphylococcus aureus grew in both peripheral blood and catheter tip blood cultures, so antibiotic therapy was de-escalated to cefazolin.
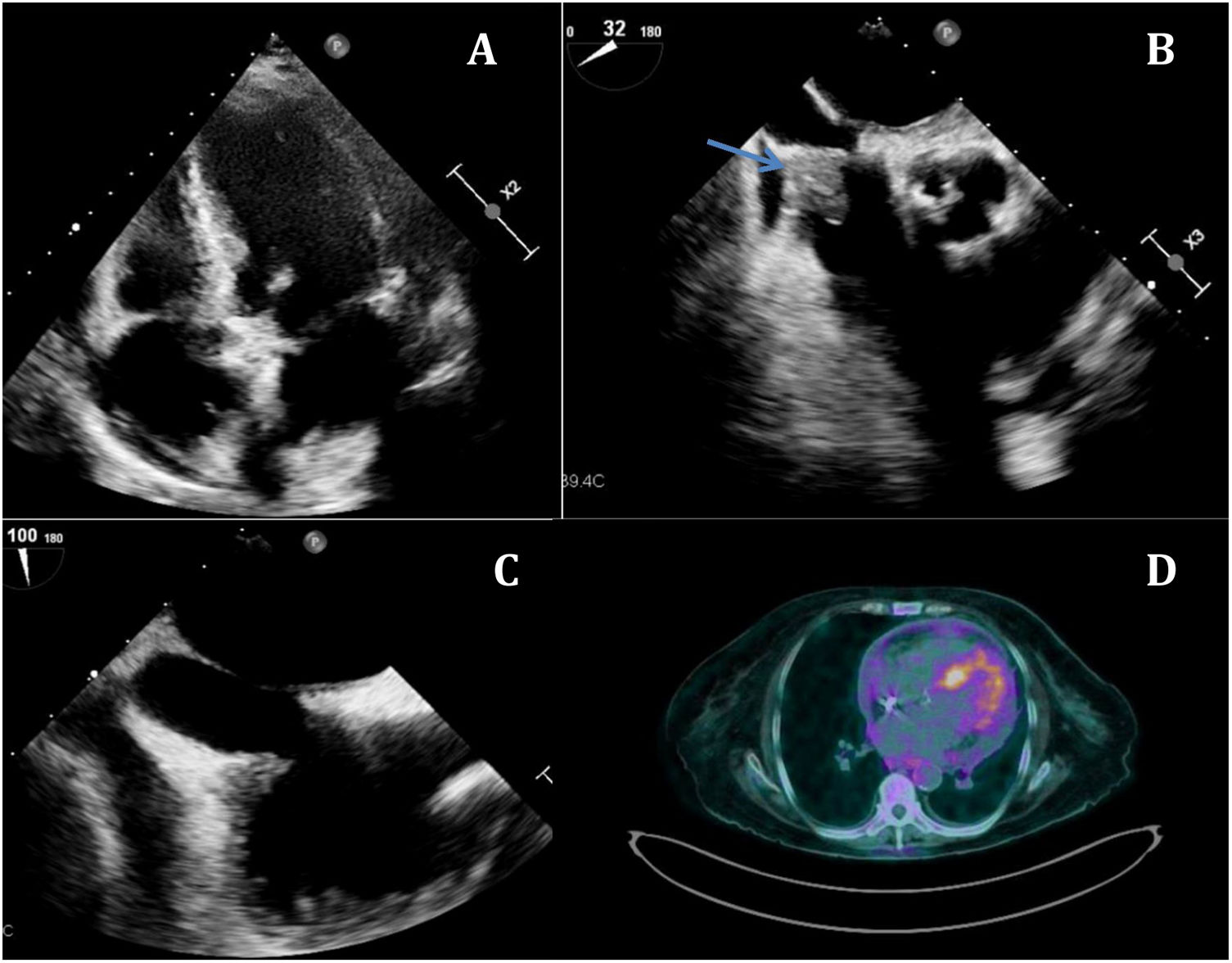
Given the positive blood cultures and pulmonary infiltrates on CT, a transthoracic echocardiogram was requested (Fig. 1A) in which moderate pericardial effusion with intrapericardial masses could be observed and, given the history, tumour implants versus nodular pericardial fat could be ruled out. In the subcostal plane, a moving nodular image appeared at the level of the entrance of the inferior vena cava in the right atrium. Given the clinical suspicion, a transoesophageal echocardiogram was performed (Fig. 1B) in which a moving image with an area of 1.83 cm2 and diameter of 1.97 cm on the compatible Eustachian valve with vegetation stands out. Other options in the differential diagnosis include tumour implant or thrombus.
A) Transthoracic echocardiogram in which a thickened Eustachian valve can be observed. B) Transoesophageal echocardiogram showing a mobile mass adhered to the valve (arrow). C) After antibiotic treatment, the mass has almost completely disappeared. D) PET/CT, slight pericardial uptake suggestive of an inflammatory process.
After two weeks of treatment with cefazolin, the blood cultures were repeated with a negative result, as well as the transoesophageal echocardiogram (Fig. 1C) which showed said mass had considerably decreased, leaving only a slight covering over the Eustachian valve. Given the good clinical course, the patient was discharged, and a week later an outpatient PET/CT was performed (Fig. 1D) where peripheral ground-glass pseudonodular opacities were observed in the right lung, suggestive of an inflammatory/infectious process in the right lung in the resolution phase, and slight uptake at the pericardial level compatible with an inflammatory process. Given the clinical context, the results of the tests and the response to treatment, tumour disease was ruled out, supporting the diagnosis of Eustachian valve endocarditis in resolution after antibiotic therapy.
CommentsThe Eustachian valve is an embryonic remnant of the right portion of the coronary sinus that in the foetal stage is responsible for directing oxygenated blood from the inferior vena cava to the left atrium through the foramen ovale. Persistent Eustachian valve in adults is a rare congenital anomaly, which in certain situations can pose a challenge as a differential diagnosis: obstruction of the inferior vena cava, intracavitary thrombosis, tumour or vegetation due to infective endocarditis.
After an extensive literature review, we can report that 40 cases of Eustachian valve endocarditis have been documented, in 38 adults and two neonates.1 The most frequent predisposing factors were electrocatheters and a central venous catheter, parenteral drug users and HIV patients, although one case without such history has been described.2 The most frequently associated microorganism was Staphylococcus aureus (18 cases), although endocarditis caused by other species of Staphylococcus, enterobacteria, fungi and Mycobacterium abscessus have also been described. In the majority, a transoesophageal echocardiogram was required for the diagnosis of endocarditis. Regarding the clinical course, five patients died, nine required surgery, one underwent percutaneous vegetectomy3 and the rest responded favourably to antibiotic therapy.
As conclusions, we can state that Eustachian valve endocarditis is a very rare disease, probably underdiagnosed,4 and that we should suspect it in those patients with predisposing factors, compatible clinical symptoms, positive blood cultures and suggestive transthoracic/transoesophageal echocardiogram.
Ethical responsibilitiesThe usual protocols have been followed on the publication of patient data, for which we received the patients' consent, thus respecting their privacy.
FundingThe authors declare that this case has not received any funding.
Please cite this article as: Gorriño Marin S, Lara García C, Gaitán Román D. Masa adherida a la válvula de Eustaquio. Enferm Infecc Microbiol Clin. 2022;40:204–205.