The epidemiological surveillance data for tuberculosis in Spain in 2015 is analysed in this report. This information was gathered through cases reported to the Red Nacional de Vigilancia Epidemiológica [National Epidemiological Surveillance Network]. In addition, the update of the treatment of the cases reported in 2014 is included. The incidence rate of tuberculosis in 2015 was 10.59 cases per 100,000 inhabitants, 10% less than in 2014. This decrease was mainly due to the sustained decreased trend of pulmonary tuberculosis rates, from other locations and in adults, while for cases of tuberculous meningitis and in children the decrease is less marked, with a tendency to stabilisation. The percentage of cases born in other countries remains stable (approximately 30% of the total). Information on HIV status is available in 63% of cases, of which 7% were HIV-positive. Regarding the treatment results, 77% of the new lung cases confirmed by culture reported in 2014 had a satisfactory result, 6% died, and 11% did not have this information.
Se presentan los resultados de la vigilancia epidemiológica de la tuberculosis en España en 2015 a partir de los casos notificados a la Red Nacional de Vigilancia Epidemiológica, así como la actualización del tratamiento de los casos declarados en 2014. La tasa de incidencia de tuberculosis en 2015 fue de 10,59 casos por 100.000 habitantes, un 10% inferior a la del año 2014. Este descenso se debió, fundamentalmente, a la tendencia descendente y sostenida de las tasas de tuberculosis pulmonar, de otras localizaciones y en los adultos, mientras que en los casos de meningitis tuberculosa y en niños el descenso es menos acusado, con tendencia a la estabilización. El porcentaje de casos nacidos en otros países se mantiene estable (aproximadamente 30% del total). Se dispone de información sobre el estatus VIH del 63% de los casos, de los que el 7% fueron VIH positivos. Respecto a los resultados de tratamiento, el 77% de los casos nuevos pulmonares confirmados por cultivo declarados en 2014 tuvieron un resultado satisfactorio, 6% fallecieron, y del 11% no se disponía de información.
Tuberculosis (TB) continues to be one of the world's biggest threats to the health and prosperity of many communities. According to World Health Organization (WHO) estimates, in 2015, 10.4 million people worldwide fell ill with TB, and 1.4 million people died from TB.1 At the World Health Assembly in May 2014, the WHO adopted the End TB Strategy, a new global strategy for the fight against TB for the period 2016–2035. Its aims for 2035 are to reduce the number of deaths by 95%, and cut the number of new cases by 90% (compared to 2015 levels). Therefore, 2015 is a key year both for evaluating whether or not the aims of the previous strategy have been met, and as a transition period between the old and new strategies.1
The WHO report for 2015 reports an overall fall in the absolute number of deaths (excluding deaths of individuals with HIV) and in the incidence rate since 2000. However, the reduction in the incidence rate between 2014 and 2015 was only 1.5%, and the death rate in 2015 was 17%. To reach the End TB Strategy milestones for 2020, the incidence rate will have to decrease by 4–5% per year worldwide, and the mortality rate will have to be cut by 10%.1
Tuberculosis surveillance in the countries of the European Union/European Economic Area (EU/EEA) is the responsibility of the European Centre for Disease Prevention and Control (ECDC).2 The ECDC compiles the data sent in each year individually by the different countries in the EU/EEA in coordination with the WHO Regional Office for Europe, which collects data from the rest of the non-EU/EEA countries in Europe, and they produce a joint report.
Spain is considered to be among the countries with a low incidence according to the ECDC, with low incidence defined as fewer than 20 cases per 100,000 population. According to the data in the last joint ECDC/WHO report from 2015, published in 2017, the notification rate in Spain was slightly lower than the EU average (11.7), with values similar to those of Hungary (9.2) and the United Kingdom (9.6). The EU/EEA country with the highest rate was Romania, with 76.5 cases per 100,000 population, followed by Latvia at 36.3. Iceland and Greece had the lowest rates with 2.1 and 4.4 cases per 100,000 population, respectively. The average rate for the European Region as a whole was 36 cases per 100,000 population.2
Although the overall incidence in Europe has undergone an average annual decline of 3% since 2009, that decline needs to accelerate if we are to achieve the targets set by the new global strategy. Moreover, Europe is the most affected region in terms of proportion of cases of multidrug-resistant TB. Another challenge facing Europe is to improve treatment outcomes, with current success rates at 76% across the region and below 52% in multidrug-resistant cases. The global strategy is being adapted to a regional level for that reason through the development of a specific action plan.
TB surveillance and monitoring in SpainIn Spain, pulmonary tuberculosis has been a notifiable disease since the beginning of the 20th century. However, until 1995, it was only mandatory to notify the total number of cases of pulmonary TB at state level. Notifications were made based on clinical suspicion, which meant that it was not possible to classify the cases as suspected or confirmed, or break down the data by basic epidemiological variables, such as age or gender. After the creation of the Red Nacional de Vigilancia Epidemiológica (RENAVE) [National Epidemiological Surveillance Network] in 1995, tuberculous meningitis also became notifiable, and individualised notification was established by means of an epidemiological survey of the cases.3 In 2004, the case definition was expanded to include all forms of tuberculosis to comply with European recommendations.4,5 Since then, cases of TB affecting any site have been reported according to three notifiable categories: pulmonary TB; tuberculous meningitis; and other TB. The new RENAVE protocols, approved in 2013 by the Spanish Ministry of Health's Inter-regional Council, have already led to an improvement in TB notification. New sections were added to the individual notification survey form for laboratory tests, sensitivity tests and risk factors.6 The changes have required a certain degree of adaptation on the part of the Autonomous Regions, but they are gradually being introduced.
Results of the surveillance and monitoringThe epidemiological situation of TB in Spain is known from the notification of individual cases to RENAVE. Information on treatment outcomes is updated in the database once the data from the previous year are consolidated.
For this study, TB cases were defined as per the surveillance protocols.6 Any patient with pulmonary or extrapulmonary TB, diagnosed in 2015, was considered a case. In addition, the protocol establishes that all cases of TB diagnosed over the course of the year, whether confirmed bacteriologically or not, should be notified to RENAVE.
A descriptive analysis was carried out for the relevant variables included when the cases were notified. The incidence rates for 2015 were calculated, both for the total for Spain and by autonomous region (raw and adjusted for the Spanish population), and broken down into the three notification categories and the specific rates by age group and gender. To study the incidence according to geographic distribution, the rates were calculated according to the autonomous region where the case resided, and imported cases were not included. Estimates of the population of Spain from the Instituto Nacional de Estadística [National Institute of Statistics] for 2015 were used to calculate incidence rates. Linear regression models were used to calculate trends in the period 2007–2015. The indicators are those proposed by the ECDC to assess control of TB in the countries of the EU/EEA.7
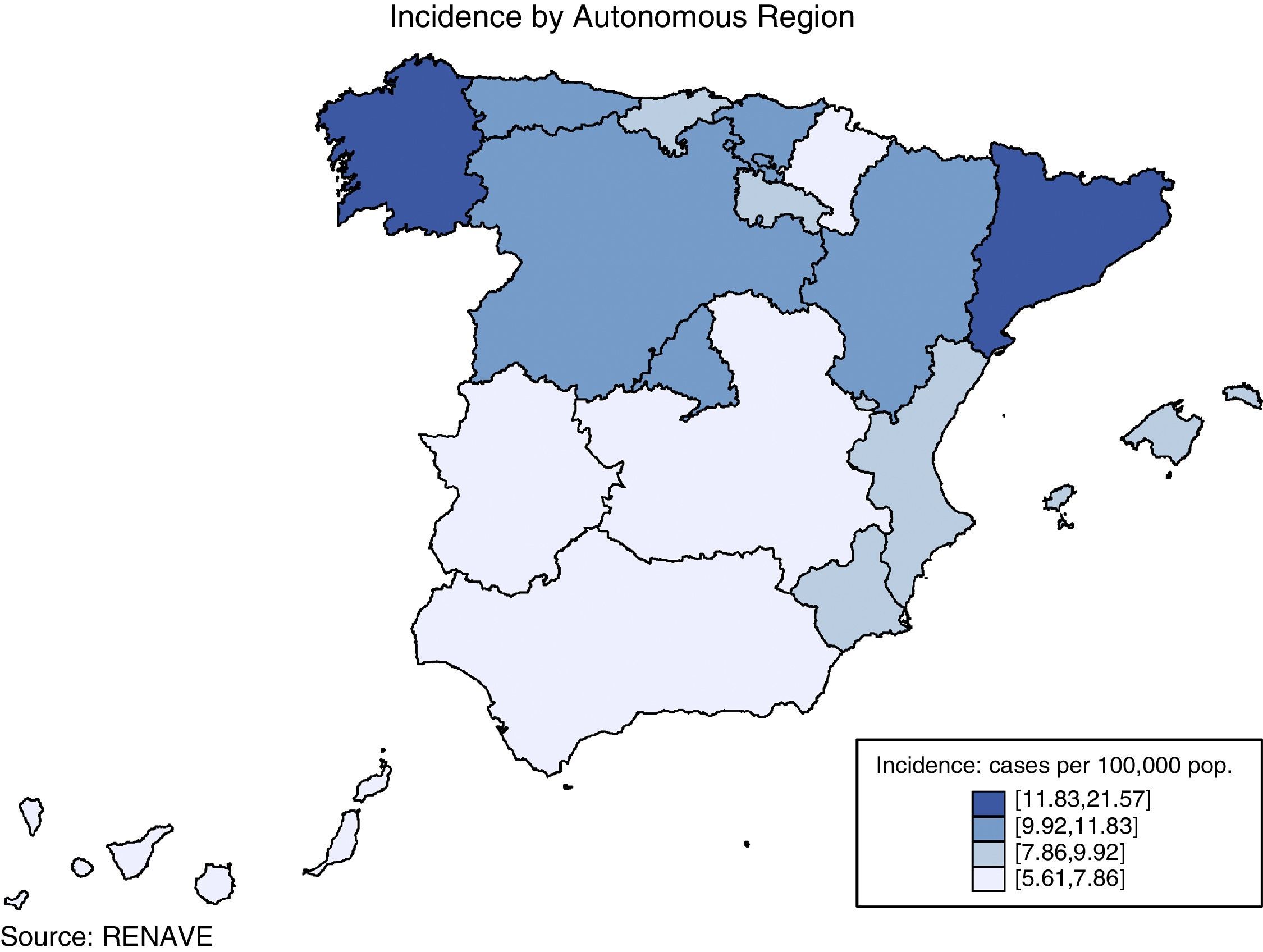
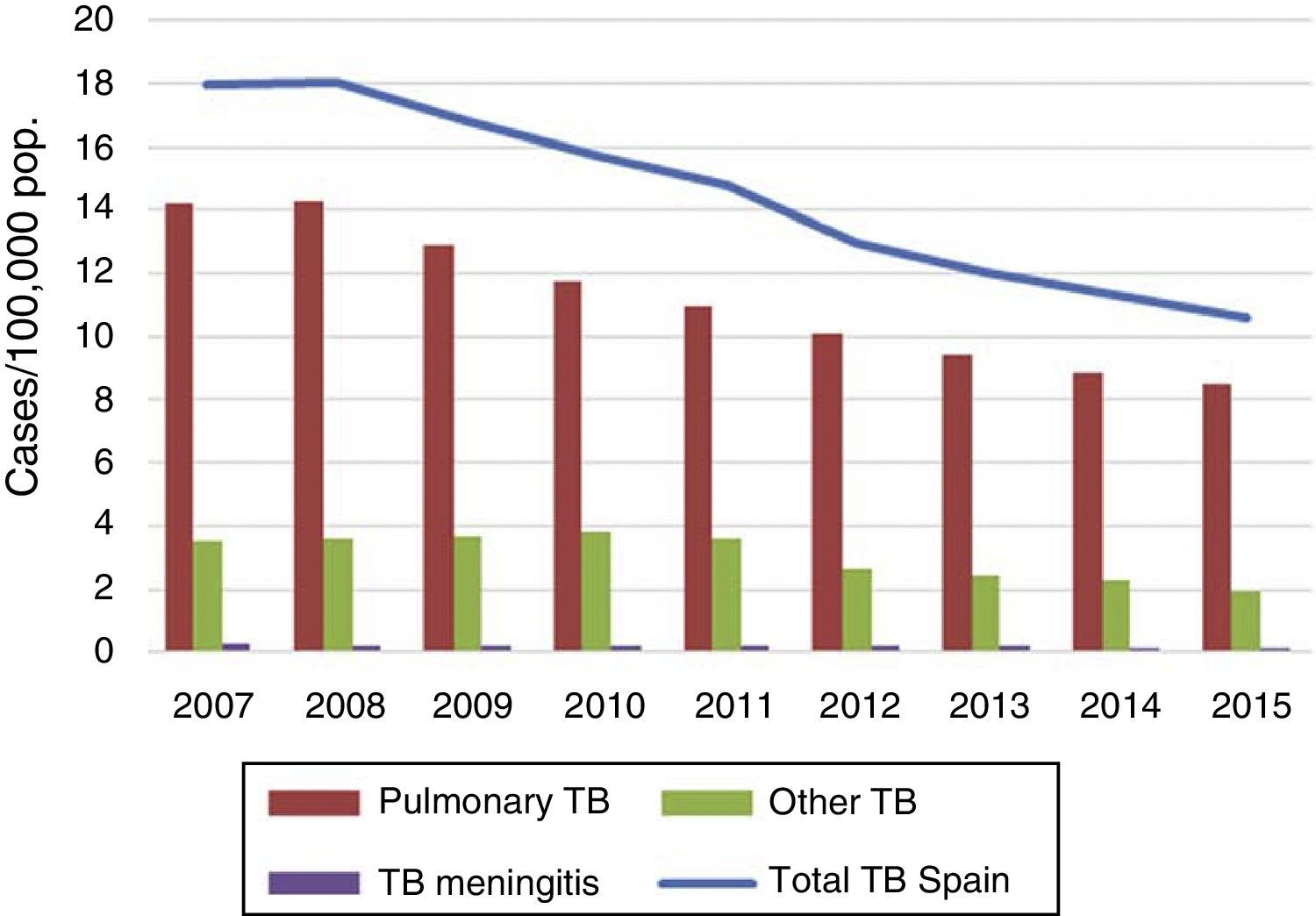
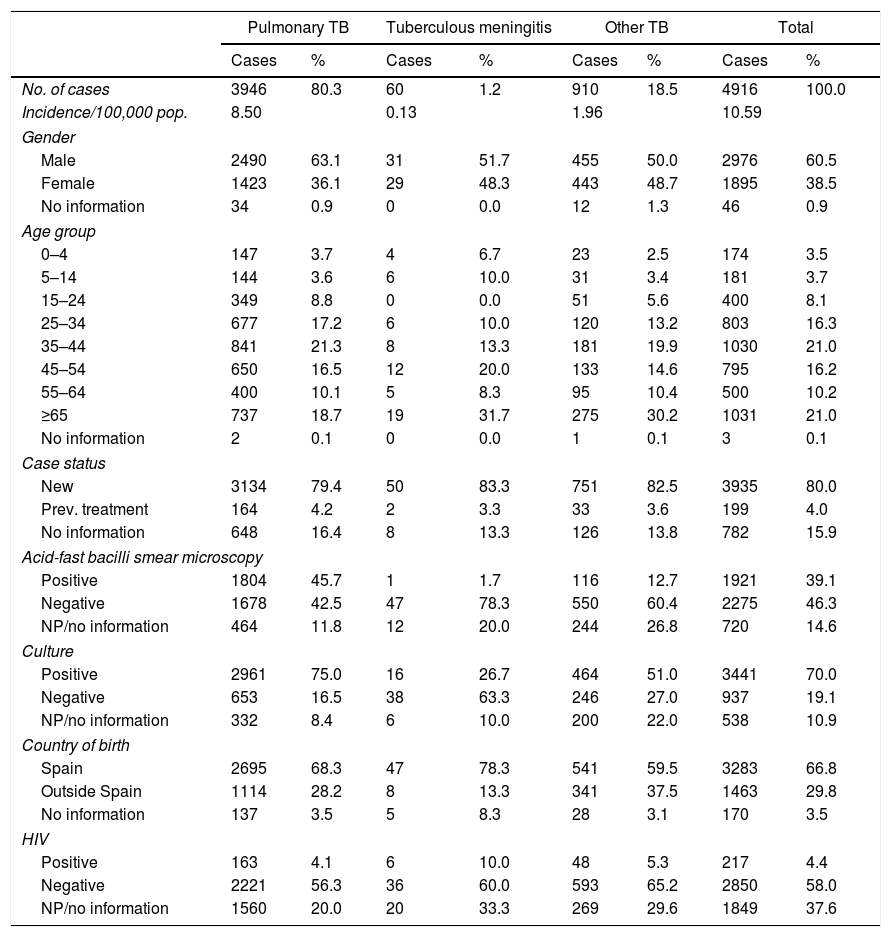
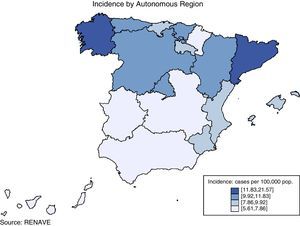
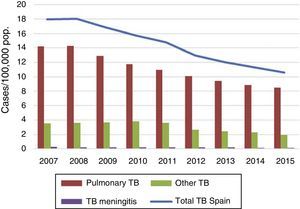
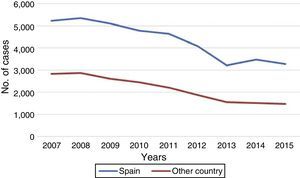
TB situation in SpainNotified cases, national incidence rate and incidence rate by autonomous regionIn 2015, 5007 cases of tuberculosis were notified in Spain, 91 of which were notified as imported cases and not therefore used for the analysis. The notification rate for the 4916 non-imported cases residing in Spain was 10.59 cases per 100,000 population; 10% lower than the 11.31 cases/100,000 population in 2014. The distribution of TB cases and rates, and by autonomous region, is shown in Fig. 1. The incidence exceeded the national rate in seven autonomous regions and the two autonomous cities. Out of the total number of cases, 3946 were pulmonary TB, 60 tuberculous meningitis, and 910 other TB (rates of 8.50, 0.13 and 1.96 cases per 100,000 population, respectively). This represents a reduction of 4% in pulmonary TB compared to the previous year (decrease from 8.87 to 8.80). In tuberculous meningitis, the rate decreased from 0.14 to 0.13, and in other TB the rate fell by 14% (from 2.29 to 1.96) (Fig. 2). The incidence of all forms of TB in Spain fell by an average of 7% annually in the period from 2008 to 2015. By disease site, the largest fall was in other TB (non-pulmonary and non-meningitis), followed by pulmonary TB. The decrease in the number of cases of tuberculous meningitis was smaller, as there have been years in which the rate remained unchanged.
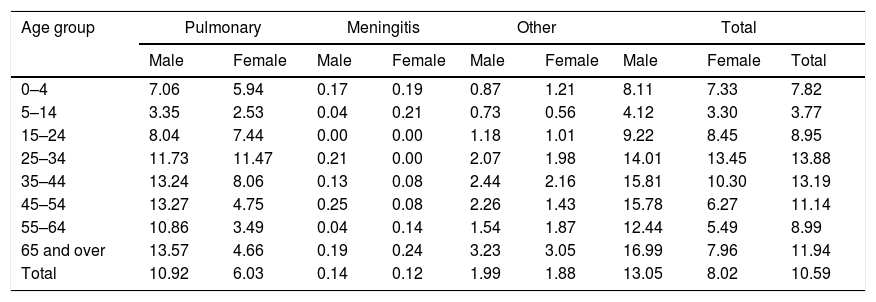
Characteristics of TB cases declared in 2015Gender, age and siteThe largest number of cases of TB occurred in males (2976, 60%), with a male/female ratio of 1.6. The mean age was 46.6±21.0 years for males and 43.5±22.5 for females (p<0.001). In 46 cases, gender was not reported. Regarding specific rates for age and gender, among males, the age groups with the highest rates were over 65, 35–44 and 45–54 (with 16.99, 15.81 and 15.78 cases per 100,000 population, respectively). Among females, the highest rate was in the 25–34 age group (13.45). The overall rate for males was 13.05 cases per 100,000 population, and, for females, 8.02 cases per 100,000 population. By age group and site (Tables 1 and 2), the age groups with the highest rates for pulmonary TB were 25–34, 35–44 and 45–54 (11.71, 10.71 and 9.11 cases per 100,000 population, respectively), whereas for tuberculous meningitis, the highest rates were in the age groups at either extreme, i.e. 65 and over (0.22) and under 4 years of age (0.18). In other TB, the highest incidence was among the over-65 age group (3.19 cases per 100,000).
TB rates according to site, age group and gender. Spain, 2015.
| Age group | Pulmonary | Meningitis | Other | Total | |||||
|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Male | Female | Male | Female | Male | Female | Total | |
| 0–4 | 7.06 | 5.94 | 0.17 | 0.19 | 0.87 | 1.21 | 8.11 | 7.33 | 7.82 |
| 5–14 | 3.35 | 2.53 | 0.04 | 0.21 | 0.73 | 0.56 | 4.12 | 3.30 | 3.77 |
| 15–24 | 8.04 | 7.44 | 0.00 | 0.00 | 1.18 | 1.01 | 9.22 | 8.45 | 8.95 |
| 25–34 | 11.73 | 11.47 | 0.21 | 0.00 | 2.07 | 1.98 | 14.01 | 13.45 | 13.88 |
| 35–44 | 13.24 | 8.06 | 0.13 | 0.08 | 2.44 | 2.16 | 15.81 | 10.30 | 13.19 |
| 45–54 | 13.27 | 4.75 | 0.25 | 0.08 | 2.26 | 1.43 | 15.78 | 6.27 | 11.14 |
| 55–64 | 10.86 | 3.49 | 0.04 | 0.14 | 1.54 | 1.87 | 12.44 | 5.49 | 8.99 |
| 65 and over | 13.57 | 4.66 | 0.19 | 0.24 | 3.23 | 3.05 | 16.99 | 7.96 | 11.94 |
| Total | 10.92 | 6.03 | 0.14 | 0.12 | 1.99 | 1.88 | 13.05 | 8.02 | 10.59 |
In 46 cases gender was unknown.
Source: RENAVE.
Characteristics of the TB cases notified individually. Spain, 2015.
| Pulmonary TB | Tuberculous meningitis | Other TB | Total | |||||
|---|---|---|---|---|---|---|---|---|
| Cases | % | Cases | % | Cases | % | Cases | % | |
| No. of cases | 3946 | 80.3 | 60 | 1.2 | 910 | 18.5 | 4916 | 100.0 |
| Incidence/100,000 pop. | 8.50 | 0.13 | 1.96 | 10.59 | ||||
| Gender | ||||||||
| Male | 2490 | 63.1 | 31 | 51.7 | 455 | 50.0 | 2976 | 60.5 |
| Female | 1423 | 36.1 | 29 | 48.3 | 443 | 48.7 | 1895 | 38.5 |
| No information | 34 | 0.9 | 0 | 0.0 | 12 | 1.3 | 46 | 0.9 |
| Age group | ||||||||
| 0–4 | 147 | 3.7 | 4 | 6.7 | 23 | 2.5 | 174 | 3.5 |
| 5–14 | 144 | 3.6 | 6 | 10.0 | 31 | 3.4 | 181 | 3.7 |
| 15–24 | 349 | 8.8 | 0 | 0.0 | 51 | 5.6 | 400 | 8.1 |
| 25–34 | 677 | 17.2 | 6 | 10.0 | 120 | 13.2 | 803 | 16.3 |
| 35–44 | 841 | 21.3 | 8 | 13.3 | 181 | 19.9 | 1030 | 21.0 |
| 45–54 | 650 | 16.5 | 12 | 20.0 | 133 | 14.6 | 795 | 16.2 |
| 55–64 | 400 | 10.1 | 5 | 8.3 | 95 | 10.4 | 500 | 10.2 |
| ≥65 | 737 | 18.7 | 19 | 31.7 | 275 | 30.2 | 1031 | 21.0 |
| No information | 2 | 0.1 | 0 | 0.0 | 1 | 0.1 | 3 | 0.1 |
| Case status | ||||||||
| New | 3134 | 79.4 | 50 | 83.3 | 751 | 82.5 | 3935 | 80.0 |
| Prev. treatment | 164 | 4.2 | 2 | 3.3 | 33 | 3.6 | 199 | 4.0 |
| No information | 648 | 16.4 | 8 | 13.3 | 126 | 13.8 | 782 | 15.9 |
| Acid-fast bacilli smear microscopy | ||||||||
| Positive | 1804 | 45.7 | 1 | 1.7 | 116 | 12.7 | 1921 | 39.1 |
| Negative | 1678 | 42.5 | 47 | 78.3 | 550 | 60.4 | 2275 | 46.3 |
| NP/no information | 464 | 11.8 | 12 | 20.0 | 244 | 26.8 | 720 | 14.6 |
| Culture | ||||||||
| Positive | 2961 | 75.0 | 16 | 26.7 | 464 | 51.0 | 3441 | 70.0 |
| Negative | 653 | 16.5 | 38 | 63.3 | 246 | 27.0 | 937 | 19.1 |
| NP/no information | 332 | 8.4 | 6 | 10.0 | 200 | 22.0 | 538 | 10.9 |
| Country of birth | ||||||||
| Spain | 2695 | 68.3 | 47 | 78.3 | 541 | 59.5 | 3283 | 66.8 |
| Outside Spain | 1114 | 28.2 | 8 | 13.3 | 341 | 37.5 | 1463 | 29.8 |
| No information | 137 | 3.5 | 5 | 8.3 | 28 | 3.1 | 170 | 3.5 |
| HIV | ||||||||
| Positive | 163 | 4.1 | 6 | 10.0 | 48 | 5.3 | 217 | 4.4 |
| Negative | 2221 | 56.3 | 36 | 60.0 | 593 | 65.2 | 2850 | 58.0 |
| NP/no information | 1560 | 20.0 | 20 | 33.3 | 269 | 29.6 | 1849 | 37.6 |
NP: not performed.
Source: RENAVE.
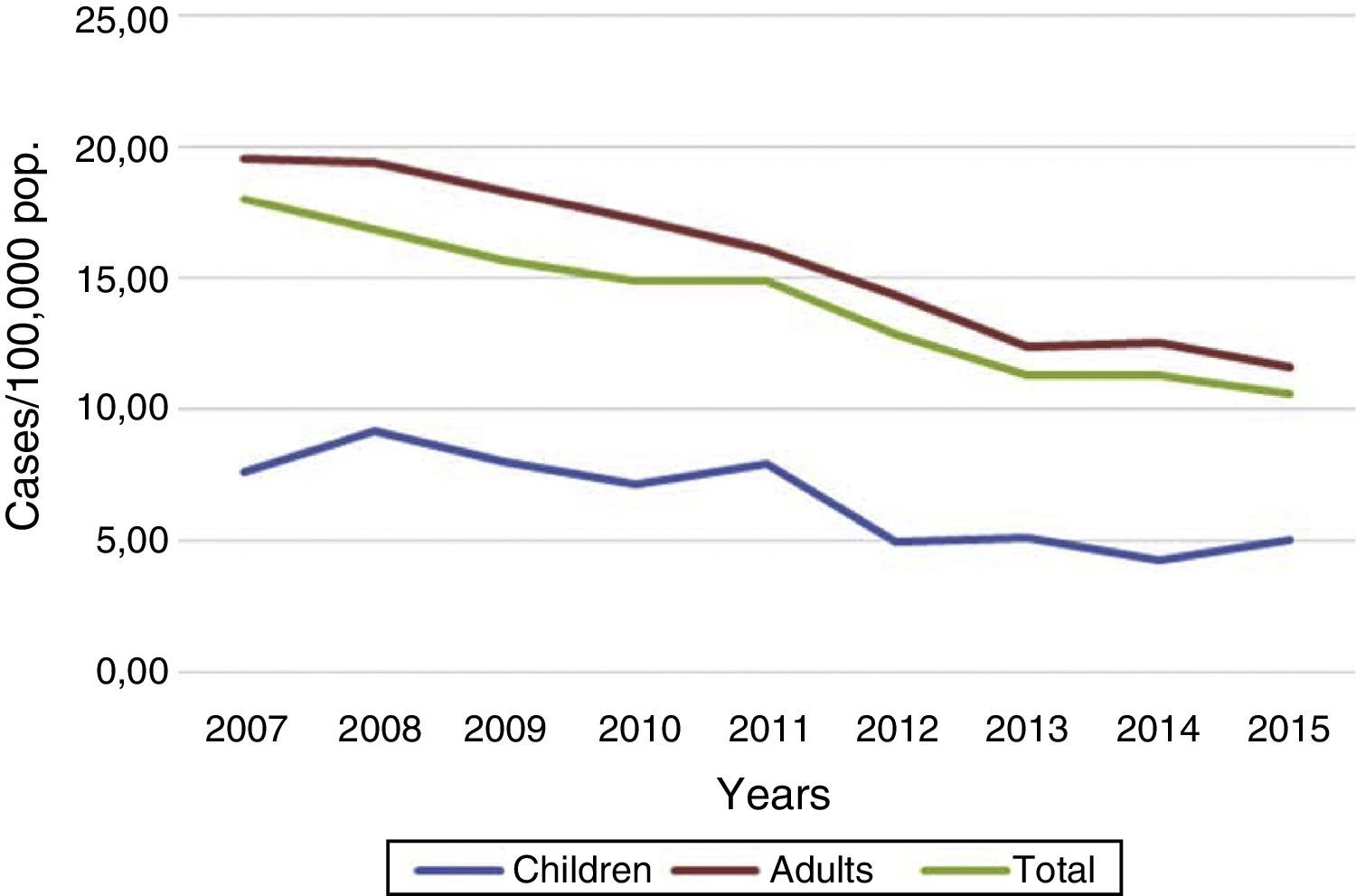
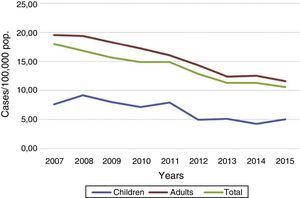
The trend of incidence rates was downward in the period 2007–2015; in adults in a sustained manner and in children (under the age of 15) with small fluctuations (Fig. 3). The mean annual rates of change were −6% in children and −7% in adults. However, in 2015 there was a slight increase with respect to the previous year (5.05 against 4.23) in the rates among children, which meant an increase in the child rate-to-adult rate ratio, from 0.34 in 2014 to 0.44 in 2015. The mean age of the cases remained similar to the previous year; 45.7 compared to 45.4. In 2015, there were 355 cases (7% of the total) in children aged under 15, distributed equally between the 0–4-year-old and 5–14 age groups. The rates of pulmonary disease are similar for children under 5 and those aged 5–14, but, for tuberculous meningitis and other TB, the rates are higher in the 5–14 age group (Table 1). One of the variables introduced in the amendment of the protocol which can be very useful for learning about the epidemiology of TB in children is the country of birth of the mother. In 2015, that information was only available for seven affected children.
If we take into account the three notification categories, 80% of the cases corresponded to respiratory TB, 1% to tuberculous meningitis and 18% to other TB. Fifteen autonomous regions provided details of the TB site when notifying the disease. According to that data, apart from pulmonary TB, which accounted for 70% of the total, and other non-specific non-respiratory sites accounting for 6%, the next most common were lymph node TB (7%) and pleural TB (6%). All the lymphatic sites were grouped together because of the lack, for the time being, of separate information on intra- and extrathoracic forms.
Previous treatmentThe majority of the cases notified (3935, 80.0%) were new, i.e. they had not received previous anti-TB treatment; 4.0% had previously received therapy, and, in 15.9%, that information was not available (Table 2). Of the 199 cases which had previously been treated, 68% were in the 25–54 age group.
Laboratory resultsLaboratory results (acid-fast bacilli smear microscopy and/or culture) were available in 5362 cases, 1743 of which were positive for both tests. Of the 3453 cases notified as pulmonary TB, 1770 were smear-positive.
A total of 3441 cases (70% of the total) were confirmed by culture (Table 2); 1145 Mycobacterium tuberculosis (M. tuberculosis), 34 Mycobacterium bovis, two Mycobacterium africanum and one Mycobacterium caprae were isolated. In the rest (2257), M. tuberculosis complex was notified without specifying. Among the cases of pulmonary tuberculosis, 75% were confirmed by culture, but the percentage was much lower in the tuberculous meningitis and other-TB cases (27% and 51%, respectively) (Table 2).
As regards the new laboratory tests introduced in the protocol amendment (detection of nucleic acid, and the presence of granulomas), the available information is still limited (970 cases with detection of nucleic acid and 514 with the presence of granulomas).
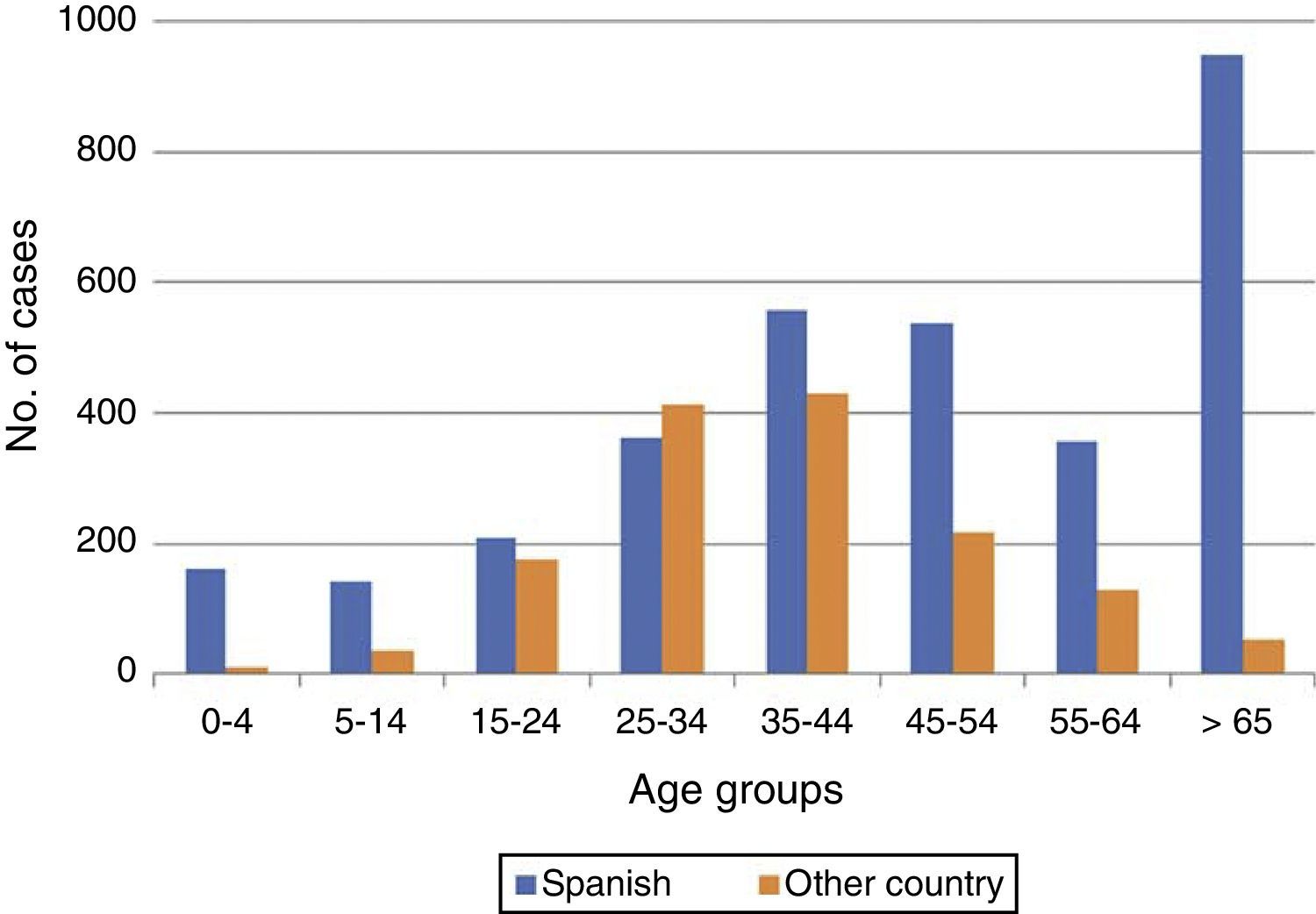
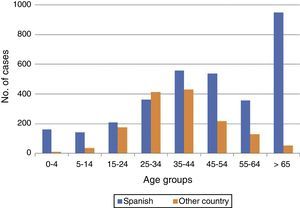
TB in patients not born in SpainIn 2015, 30% (1463) of the TB cases had not been born in Spain. In 170 cases, there was no information on place of birth. The patients not born in Spain were, in general, younger than those who had been born in Spain (mean age of 38±14 years compared to 49±24 years for Spanish-born, p<0.001). Among both Spanish-born cases and those not born in Spain, the majority were male (61% and 60%, respectively). The distribution according to age group and origin is shown in Fig. 4. The proportion of cases not born in Spain varied greatly from one autonomous region to another, with the highest proportions (37% and 20%, respectively) in the regions of Catalonia and Madrid, and the lowest in Extremadura and Asturias. Of the cases not born in Spain, information on the country of birth was available in 1463 cases: in 469 (32%) the case was notified as “not born in Spain”, but without reporting the country of birth; and in the remaining 994 cases, the actual country of birth was reported. There were up to 71 different countries; Morocco continued to be the country with the highest number of cases (230), followed by Romania (105), Bolivia (80), Peru (77) and Pakistan (60).
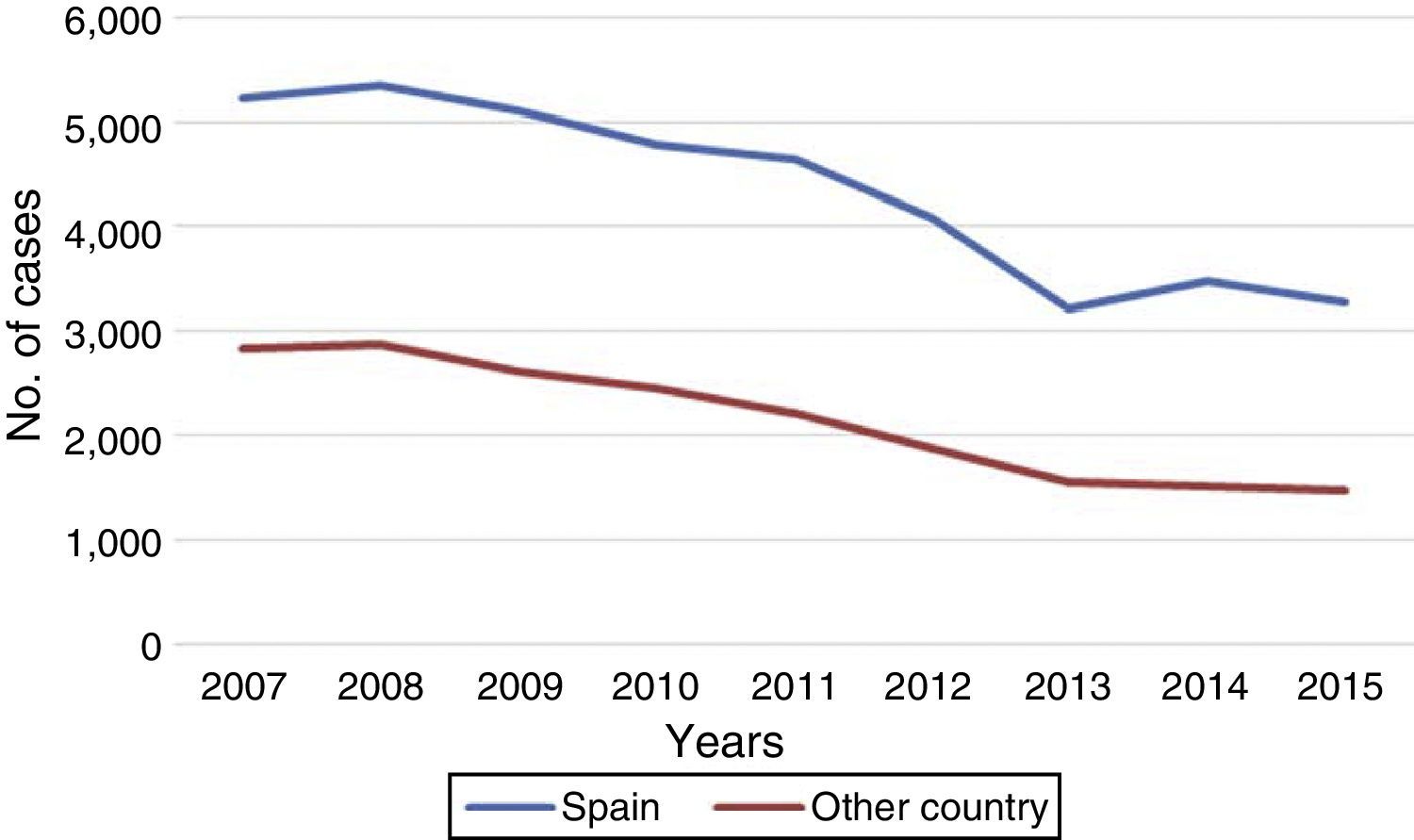
The number of notified cases who were not born in Spain continues to decline, although at a slower rate than that of those born in Spain (Fig. 5). Registering of the origin of the cases (born/not born in Spain) has improved greatly since 2007, with the information available in over 97% of cases in 2015. Information on the year of arrival in Spain was available in 524 of the cases born elsewhere. Of these, 13% had arrived in the previous two years, 8% had been residing in Spain for 3 to 5 years, 30% from 6 to 10 years and 49% for over 10 years.
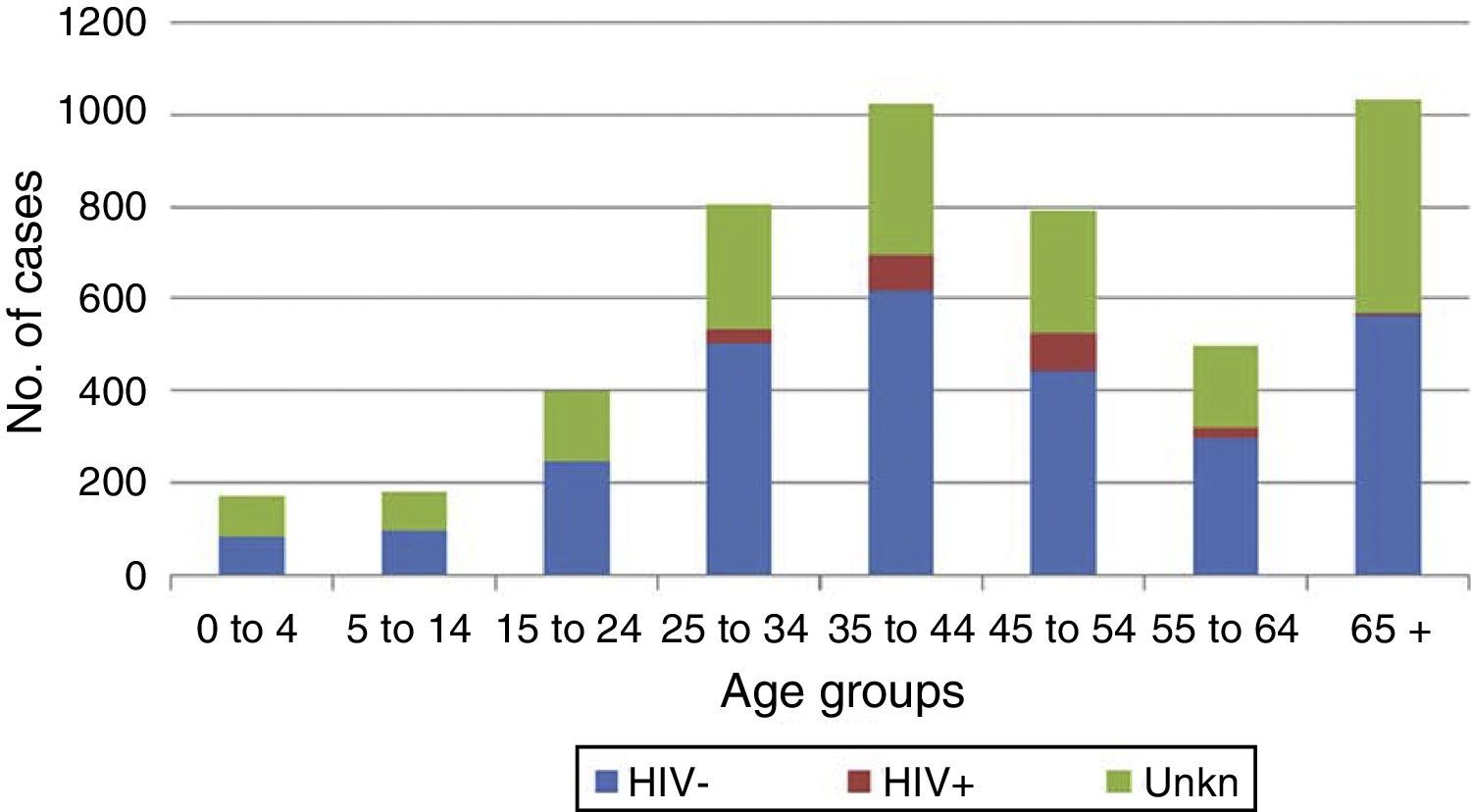
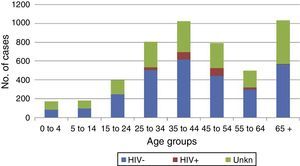
TB-HIV co-infectionIn 2015, HIV status was available for 63% of TB cases, with 217 HIV-infected individuals notified as positive, representing 4.4% of the total (7% of those with recorded status) (Table 2). Most of the HIV-positive cases were concentrated in the age groups 35–44 and 45–54 (Fig. 6). No cases of HIV-TB in children were notified. There was no difference in mean age according to HIV status (44±9 years for HIV+ compared to 45±21 years for HIV−, p=0.26). The majority of the HIV-positive cases were male (male/female ratio 3.4). The HIV-positive females were distributed in the same age groups as the HIV-positive males (35–54). The HIV-positive cases had a higher proportion of meningeal and non-respiratory forms than the HIV-negative cases (2.8% and 22.1% among HIV+ compared to 1.3% and 20.8% among HIV−, respectively). With regard to other characteristics, there were a higher percentage of previously treated cases among the HIV-positive cases of TB than among the HIV-negative cases (12% vs 4%), and a higher proportion of cases confirmed by culture (77% vs 70%).
Other risk factorsVariables about risk factors, such as injected drug use and alcoholism, which were not previously contemplated, have been included in the new protocol. For 2015, information on risk factors was only available in 109 cases. A history of alcohol use was reported in 43 cases, injected drug use (IDU) in six and alcohol use plus IDU in three. The other 57 cases were reported as having another risk factor. The data for 2015 includes information on hospital admission in 3821 cases, with 1452 (38%) being hospitalised. In the new protocol, “hospitalisation” is defined as at least one overnight stay in hospital.
End-of-treatment outcomes for the 2014 casesAs recommended internationally, the categories of cured and treatment completed were grouped into the single category of “treatment success”. Deaths are presented in a single category as it is still not possible to separate TB deaths from other causes.
The tuberculosis cases notified with treatment success in 2014 represented 76% of the total (2062 cases reported cured and 1952 with treatment completed), and 77% of the new pulmonary cases confirmed by culture. The above figures signify a worsening compared to the previous year, when treatment success was over 80% in both groups. This information was not available in 11% of the cases overall, slightly higher than the previous year (9%). In the updated information for 2014, of the 5251 cases not imported, 325 deaths were reported (6%).
Outbreaks of pulmonary TBIn the surveillance protocol, the development of one or more cases of tuberculosis from the same index case, within a period of one year after diagnosis of the primary case, is considered an outbreak for intervention purposes. When groups of cases have been identified by molecular techniques, grouping is defined as: two or more cases of TB with identical IS6110 restriction fragment length polymorphism (RFLP) pattern; or, in strains with fewer than six bands of the IS6110-RFLP pattern, those that share the same spoligotyping, PGRS-RFLP or MIRU-VNTR pattern. The protocol also sets out that the Autonomous Region's Surveillance Department will send the final report on the outbreak to the Centro Nacional de Epidemiología (CNE) [Spanish Epidemiology Centre] within three months of completing its investigation. This causes a delay in outbreak notification with respect to the notification of cases, and different dates for consolidation of the information.
An average of 84 outbreaks/year were reported in the 2011–2015 period. The majority of outbreaks notified were in a family setting (324 outbreaks, 77% for the entire period). Next were outbreaks classified as “others” (38 outbreaks, 9%), which are very heterogeneous and usually refer to workplace outbreaks, and then outbreaks in schools/nurseries (29 outbreaks, 7%). In this last area, although the number of outbreaks is small, they can involve a large number of cases.
Tests for sensitivity to anti-TB drugsData from tests on sensitivity to anti-TB drugs carried out in 2015 on strains of M. tuberculosis came from 14 autonomous regions and cities which sent information about resistance to the CNE. Strains of M. tuberculosis resistant to at least isoniazid and rifampicin are defined as multidrug-resistant TB (MDR-TB). Strains which, in addition to being multidrug-resistant, have resistance to fluoroquinolones and to one or more of the second-line drugs for injection (amikacin, capreomycin or kanamycin), are defined as extensively drug-resistant (XDR).
Results were available for susceptibility tests in 898 cases of non-imported pulmonary tuberculosis in 2015. Forty-two cases were MDR (4.7% of those analysed) and, of these, one (2.4%) was considered XDR.
DiscussionThe incidence rates of TB in Spain are on a downward trend. There was a fall in rates for all sites, and, for tuberculous meningitis, this was the third consecutive year after a period of stabilisation. However, for low-incidence countries, the WHO has estimated that an annual decrease of 11% would be necessary to achieve elimination by 2050 (defined as less than one case per million population per year),8 and, in Spain, the decrease was only 7% for the period from 2008 to 2015. These data suggest that additional efforts are needed to achieve the above goal.
Analysis of the rates by age group indicates that there is active transmission of the disease. One of the age groups with the highest pulmonary TB rates is adults aged 25–34. Given the higher rates of active transmission in this age group, and the fact that half of these cases come from countries where TB is highly endemic, early detection of pulmonary TB in young adults needs to be intensified in order to cut the chains of transmission.
As far as children are concerned, the indicators relating to childhood TB have improved (incidence rates and the ratio of childhood/adult TB rates have decreased, while the average age of cases has increased). However, we need to be vigilant, stressing the importance of adequate testing of contacts and early diagnosis of cases when pulmonary TB is found in adults, giving special attention to family contacts under the age of 5 and the control of outbreaks in schools. In the majority of cases of childhood TB, the children have been born in Spain, and we do not know what percentage are from immigrant families; the country of origin of the parents is one of the new variables included in the amendment to the surveillance protocols, and there is very little information available.
In younger people, both males and females, the high incidence may be related to a higher percentage of immigrants from countries where TB is highly endemic, particularly for the 25–34 age group, in which more than half of the TB cases are non-Spanish. There is also more active transmission among young people, both Spaniards and non-Spaniards. In contrast, in the older age groups, the majority of cases are Spanish and male. This may be the result of a greater prevalence of risk factors and risky behaviours (HIV, smoking, occupational exposure, etc.) and, for males and females, reactivation of the disease caused in adulthood. Elderly people are also more likely to develop extrapulmonary forms of the disease, which are more difficult to detect and treat; hence the importance of controlling it. This requires increasing clinical awareness in terms of suspecting TB in elderly people, who are more difficult to treat and have correspondingly higher TB-related mortality rates.
The number of cases born outside Spain has been decreasing in recent years, in parallel to that of Spanish cases, although less markedly, and the proportion of the total remains at 30%. Taking into account that the average age of these cases is 37, and that many come from countries in Africa, Asia or Eastern Europe, where TB is highly endemic, early diagnosis and testing of contacts is extremely important in order to cut possible chains of transmission as quickly as possible. We also have to be aware of labour mobility and the precarious living conditions many of these people endure, with these factors further reinforcing the importance of bringing it under control.9
The information available on the year of arrival in Spain in foreign cases, although not representative, seems to indicate that most have been living in Spain for over 5 years. This is consistent with figures reported by some of the autonomous regions,10 but we will need to have national data before we can perform a more detailed analysis.
The number of TB cases positive for HIV continued to decrease compared to previous years (217 in 2015 compared to 237 in 2014), although we should point out that the information about HIV status in TB cases is not complete, in particular for young adults and those over 65, and an evaluation cannot therefore be made until these data are consolidated. As is customary in the epidemiology of TB, the majority of cases of TB co-infected with HIV are male, and the mean age does not differ significantly from HIV-negative cases. The age group with the highest percentage of cases with no information about HIV status is the over-65s, followed by young adults, so we need to stress the importance of collecting information in these groups. We must not forget that HIV infection is one of the main risk factors for the reactivation of latent tuberculosis infection, and that, while the risk of developing TB in an immunocompetent person is 10% throughout their lifetime, for a person with HIV it is 15% per year.
One of the basic indicators proposed by the ECDC to evaluate the European Action Plan is the percentage of TB cases in which HIV status is known.8 The goal is to have information on all notified cases. In the case of elderly people, one reason for the lack of information could be the low perception of risk in this group in terms of testing for HIV. However, in young adults, it is probably because of deficiency in the collection of information.11
With regard to other risk factors included in the new protocol which healthcare workers have recently started to record, it is still early to carry out an evaluation as the information available remains very limited (use of drugs, alcohol, etc.). The additional information requirements introduced into the new TB protocol6 are gradually being incorporated into the surveys of the cases notified by the autonomous regions, and will help to identify risk groups and contribute to improving surveillance and control of tuberculosis in Spain.12
One of the variables, for which information is already being collected, is hospitalisation. Although not representative, the 2015 data on the percentage of hospitalised cases seem to be in line with the studies conducted from the Minimum Basic Set of Hospital Data and the surveillance data from the autonomous regions,10,13,14 and show that the percentage of hospitalised cases is quite high, although we cannot determine length of stay from the RENAVE surveillance.
The data regarding the completion of anti-TB treatment have worsened compared to the previous year, in terms of the percentage of cases with treatment success.
In the latest ECDC report, overall figures for the entire EU/EEA indicated 76% treatment success in patients who started treatment in 2014.2 The figures for Spain were similar to the European average. Nevertheless, these figures are lower than the internationally established target of 85%.1,15 There may be a number of different reasons for these deficiencies, among which the ECDC points to the high percentage of cases still undergoing treatment in some countries, problems with the collection of information, and the high number of deaths, particularly in the Spanish cases with an older mean age, as this leads to greater complications during treatment, with more likelihood of fatal outcome.16 A similar situation was recently reported in Spain from the surveillance data, showing that 8% of Spanish cases die during anti-TB treatment, compared to 3% of those born in other countries.17 It has also been found that young adults not born in Spain have a higher risk of not completing the treatment.18 In relation to deaths during treatment, the new protocol differentiates TB-related death from death from other causes, but for the analysis it was considered as one single category as the information available at present is very limited.
Both the national12 and international guidelines (ECDC7 and WHO in their new strategy1) recommend that all TB cases confirmed by culture should be tested for microbial susceptibility at least to first line anti-TB drugs. In Spain, that information is still not representative at a national level, and is only notified by some autonomous regions. The aim is to routinely include the anti-TB susceptibility results in the case notification surveys, in order to steadily improve the amount of information available and allow comparison with other countries. Despite the present limitation, levels of resistance to anti-TB drugs in Spain are similar to the European average2 (4.1% MDR cases in the EU/EEA in 2013, and 4.7% in Spain in 2015).
The information provided by the notification of outbreaks shows us that the majority occur in the family environment, reinforcing the importance of thorough testing of contacts in each case of pulmonary TB. Control of outbreaks in schools is also very important to prevent the complications TB can cause in young children.19
We would like to conclude by stating that analysis of the surveillance data by RENAVE confirms that the incidence of TB in Spain is decreasing, but at a lower rate than desirable to reach the goals for the elimination of TB.8
In line with the objectives of the 2016–2035 World Plan for the control of TB, we need to follow the recommendations of the new global elimination strategy (End TB Strategy) which, among other things, is based on early diagnosis, detection of risk groups, universal healthcare coverage and patient support. We also need to intensify and promote research and innovation aimed at the development of new drugs with shorter treatment regimens and new vaccines. All this requires a political commitment, and an improvement in cooperation between sectors.1
Conflicts of interestThe authors declare that they have no conflicts of interest.
To the professionals who have carried out the surveillance and notification of the cases at the different levels of the Red Nacional de Vigilancia Epidemiológica (RENAVE) [National Epidemiological Surveillance Network] and in the Tuberculosis Programmes in the Autonomous Regions and the Autonomous Cities of Ceuta and Melilla. We would also like to express our gratitude to the Mycobacteria Laboratory at the Centro Nacional de Microbiología [National Microbiology Centre] (ISCIII, Madrid) and the professionals who work in the clinical microbiology laboratories for their collaboration.
Please cite this article as: Cano-Portero R, Amillategui-dos Santos R, Boix-Martínez R, Larrauri-Cámara A. Epidemiología de la tuberculosis en España. Resultados obtenidos por la Red Nacional de Vigilancia Epidemiológica en el año 2015. Enferm Infecc Microbiol Clin. 2018;36:179–186.