To estimate the economic and health impact of chronic complications (macrovascular and microvascular) of type 2 diabetes mellitus (T2DM) in the autonomous community of Madrid (Spain) (ACM).
MethodsThe number of expected complications was obtained from a descriptive, cross-sectional study on a cohort of 3268 patients with T2DM from the ACM. Cost of complications (€, 2012) was assessed both at hospitals and in primary care. The number of medical visits in primary care and drug treatment for complications were collected by a panel of 21 physicians experienced in treatment of T2DM. Population and epidemiological data and healthcare costs were obtained from Spanish sources. Univariate sensitivity analyses were performed.
ResultsIt is estimated that there are 390,944 patients with T2DM in the ACM, and that they experience 172,406 and 212,283 macrovascular and microvascular complications respectively during their lifetimes. Mean cost of T2DM complications per patient is estimated at €4121.54 (66% due to macrovascular complications). The economic impact of T2DM complications in the ACM would be €1611 million (1065 and 545 millions from macrovascular and microvascular complications respectively). The economic impact would range from €1249 and 2.509 million euro depending on T2DM prevalence.
ConclusionsComplications of T2DM have a great health and economic impact in ACM.
Estimar el impacto económico y sanitario de las complicaciones crónicas macro y microvasculares de la diabetes mellitus tipo 2 (DM2) en la Comunidad de Madrid (CM).
MétodosEl número de complicaciones esperadas se obtuvo de un estudio descriptivo transversal que incluyó una cohorte de 3.268 pacientes con DM2 de la CM. El coste de las complicaciones (€ de 2012) se valoró tanto a nivel hospitalario como en la atención primaria. El número de consultas médicas en atención primaria y el tratamiento farmacológico de las complicaciones se obtuvo mediante un panel de 21 médicos con experiencia en el tratamiento de la DM2. Los datos poblacionales, epidemiológicos y los costes sanitarios se consiguieron de fuentes españolas. Se hicieron análisis de sensibilidad univariantes.
ResultadosSe estima que la población con DM2 en la CM asciende a 390.944 pacientes y que estos sufren a lo largo de su vida 172.406 y 212.283 complicaciones macro y microvasculares, respectivamente. El coste promedio de las complicaciones de la DM2 por paciente se calcula en 4.121,54€ (el 66% debido a las complicaciones macrovasculares). El impacto económico de las complicaciones de la DM2 en la CM sería de 1.611 millones de euros (1.065 en las complicaciones crónicas de tipo macrovascular y 545 en las complicaciones de tipo microvascular). El impacto económico oscilaría entre los 1.249 y los 2.509 millones de euros, según la prevalencia de DM2.
ConclusionesLas complicaciones de la DM2 tienen un gran impacto, tanto sanitario como económico en la CM.
Diabetes mellitus (DM) is a metabolic disease characterized by the presence of hyperglycemia secondary to insulin secretion deficit or absence and/or to a receptor or post-receptor defect in insulin action, with impaired insulin secretion and/or biological action.1 Hyperglycemia causes chronic microvascular and macrovascular complications which are common to all types of DM.1 Specifically, type 2 diabetes mellitus (T2DM) is due to resistance to insulin action and to a relative deficiency in insulin secretion. In the initial phases therefore, hyperinsulinism, and usually hyperglycemia, occur.1
According to the World Health Organization, more than 364 million people suffer DM worldwide. DM is becoming a global epidemic, related to the rapid increase in overweight, obesity, and physical inactivity. Deaths from DM are expected to increase by more than 50% in the next 10 years, and DM is expected to be the seventh leading cause of death by 2030.2 The achievement of treatment goals is essential for adequate control of this pandemic. In our healthcare system, primary care physicians are mainly responsible for the diagnosis, treatment, and monitoring of patients with T2DM, with the implementation of ad hoc programs being required to meet these treatment goals.3,4
T2DM is one of the chronic diseases showing the greatest increase in prevalence over the past 50 years.5 In Spain, its prevalence rate ranges from 6% to 15% depending on the study.5–7 In the Community of Madrid (CM), the prevalence of T2DM has been estimated at 8.1%,5 is higher in males (10.2%) as compared to females (6%), and increases with age up to 23.1% between 70 and 74 years of age.7–9 T2DM is among the most significant causes of early death in the adult Spanish population. It is the third and seventh leading cause of death in females and males respectively.5,10
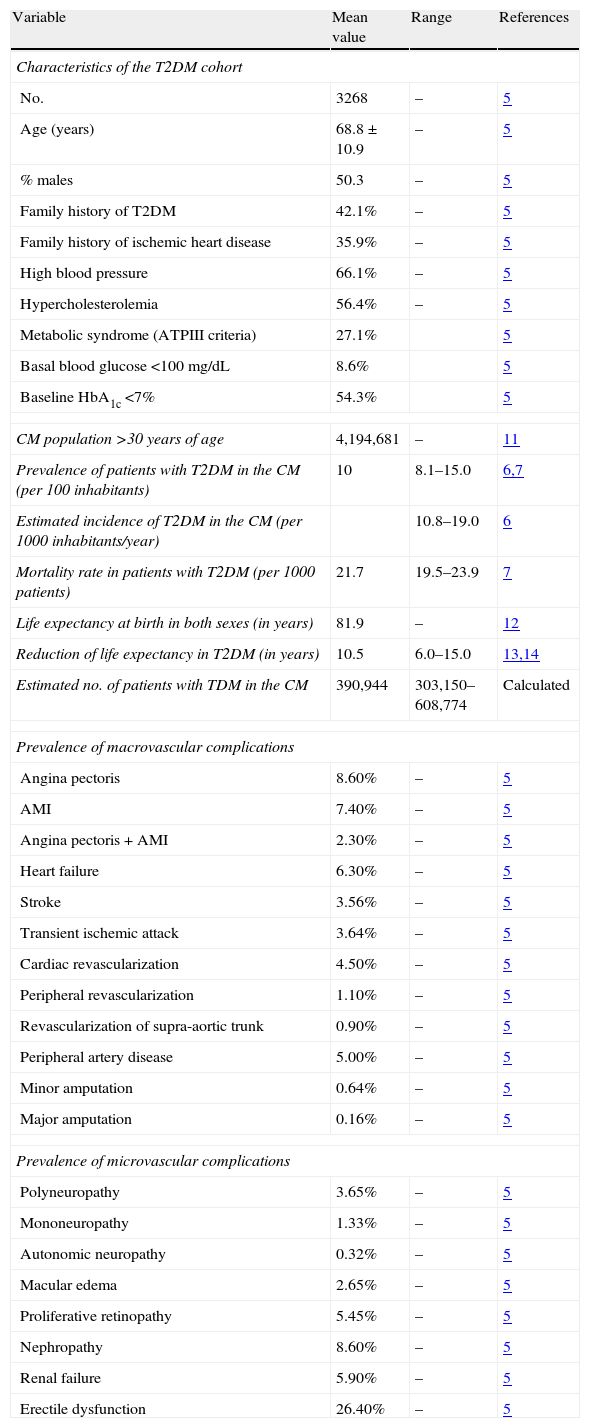
A recent descriptive, cross-sectional study conducted by Arrieta et al.5 on a cohort of patients with T2DM from the CM reported the prevalence of chronic macrovascular and microvascular complications of T2DM (Table 1).
Population and epidemiological premises assumed in the economic model.
| Variable | Mean value | Range | References |
| Characteristics of the T2DM cohort | |||
| No. | 3268 | – | 5 |
| Age (years) | 68.8±10.9 | – | 5 |
| % males | 50.3 | – | 5 |
| Family history of T2DM | 42.1% | – | 5 |
| Family history of ischemic heart disease | 35.9% | – | 5 |
| High blood pressure | 66.1% | – | 5 |
| Hypercholesterolemia | 56.4% | – | 5 |
| Metabolic syndrome (ATPIII criteria) | 27.1% | 5 | |
| Basal blood glucose <100mg/dL | 8.6% | 5 | |
| Baseline HbA1c <7% | 54.3% | 5 | |
| CM population >30 years of age | 4,194,681 | – | 11 |
| Prevalence of patients with T2DM in the CM (per 100 inhabitants) | 10 | 8.1–15.0 | 6,7 |
| Estimated incidence of T2DM in the CM (per 1000 inhabitants/year) | 10.8–19.0 | 6 | |
| Mortality rate in patients with T2DM (per 1000 patients) | 21.7 | 19.5–23.9 | 7 |
| Life expectancy at birth in both sexes (in years) | 81.9 | – | 12 |
| Reduction of life expectancy in T2DM (in years) | 10.5 | 6.0–15.0 | 13,14 |
| Estimated no. of patients with TDM in the CM | 390,944 | 303,150–608,774 | Calculated |
| Prevalence of macrovascular complications | |||
| Angina pectoris | 8.60% | – | 5 |
| AMI | 7.40% | – | 5 |
| Angina pectoris+AMI | 2.30% | – | 5 |
| Heart failure | 6.30% | – | 5 |
| Stroke | 3.56% | – | 5 |
| Transient ischemic attack | 3.64% | – | 5 |
| Cardiac revascularization | 4.50% | – | 5 |
| Peripheral revascularization | 1.10% | – | 5 |
| Revascularization of supra-aortic trunk | 0.90% | – | 5 |
| Peripheral artery disease | 5.00% | – | 5 |
| Minor amputation | 0.64% | – | 5 |
| Major amputation | 0.16% | – | 5 |
| Prevalence of microvascular complications | |||
| Polyneuropathy | 3.65% | – | 5 |
| Mononeuropathy | 1.33% | – | 5 |
| Autonomic neuropathy | 0.32% | – | 5 |
| Macular edema | 2.65% | – | 5 |
| Proliferative retinopathy | 5.45% | – | 5 |
| Nephropathy | 8.60% | – | 5 |
| Renal failure | 5.90% | – | 5 |
| Erectile dysfunction | 26.40% | – | 5 |
ATPIII: Adult Treatment Panel III; CM: Community of Madrid; T2DM: type 2 diabetes mellitus; HbA1c: glycosylated hemoglobin; AMI: acute myocardial infarction; No.: number of patients.
This study was intended to assess the economic and care impact associated with microvascular and macrovascular complications occurring in patients with T2DM from the CM monitored at primary care.
MethodsThe study consisted of two phases. In the first phase, an expert panel consisting of 21 primary care physicians experienced in T2DM management and monitoring was consulted in order to find out the number of primary care visits and drug treatments used as a consequence of chronic complications of T2DM. The second study phase consisted of an analysis of the cost of such complications based on resource utilization estimated by the expert panel. For this analysis, carried out using an economic model and referring to the population with T2DM in the CM, the previously reported population and epidemiological premises summarized in Table 1 were used.
The number of patients with T2DM was estimated for the total population of the CM older than 30 years (inclusion criterion of the abovementioned study),5 which was 4,194,681 inhabitants according to the National Statistics Institute database.11 Based on the available data on T2DM prevalence,6,7 incidence,6 and mortality,7 a population of 390,944 patients with T2DM was estimated at the CM, in the base case of the analysis, using the mean values of the above three variables. If the minimum or maximum values of the variables were considered, the population ranged from a minimum of 303,150 to a maximum of 608,774 patients with T2DM in the CM. The mean population of patients with T2DM in the CM (390,944 patients) was calculated based on the following assumptions: (i) an estimated prevalence of T2DM of 10 cases per 100 individuals6,7 (10% of 4,194,681=419,468 prevalent cases in the CM); (ii) that incident cases of T2DM amounted to 14.9 per 1000 inhabitants/year, according to the Valdés et al. study6 (thus, new annual patients with T2DM in the CM would be [4,194,681×14.5/1000]=62,501); (iii) that the mortality rate in patients with T2DM was 21.7 cases per 1000 patients (i.e. [4,194,681×21.7/1000]=91,025); (iv) the mean population with T2DM in the CM was therefore estimated as 419,468+62,501−91,025=390,944 patients (Table 1).
Chronic complications, both macrovascular (angina, acute myocardial infarction, heart failure, stroke, transient ischemic attack, cardiac, peripheral, and supra-aortic trunk revascularization, peripheral artery disease, and minor and major amputations), and microvascular (polyneuropathy and mononeuropathy, autonomic neuropathy, macular edema, proliferative retinopathy, nephropathy, renal failure, and erectile dysfunction), that occur in patients with T2DM were estimated. Estimates were based on the prevalence found retrospectively in the descriptive, cross-sectional study conducted by Arrieta et al. on a cohort of 3268 patients from the CM with T2DM aged 68.8±10.9 years and with a mean disease duration of 7.9±7.4 years5 (Table 1). The time horizon considered in the study corresponded to the time from the onset of disease. Thus, as an example, since the Arrieta et al. study reported the occurrence of angina pectoris in 8.6% of patients from the T2DM cohort, the number of patients with T2DM who experienced angina in the CM over a period of 7.9±7.4 years was estimated as 390,944×8.6%=33,621.5 The number of all other macrovascular and microvascular complications of T2DM in the CM was similarly estimated. The economic model assumed that the same patient with T2DM could experience more than one episode of a complication in the time horizon considered.
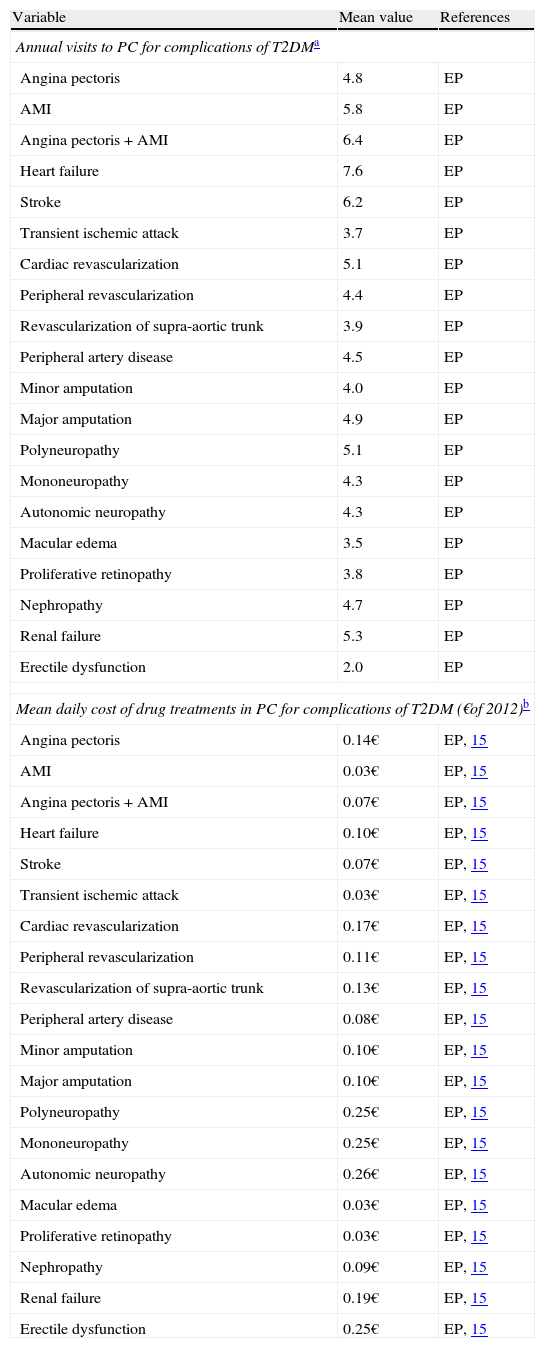
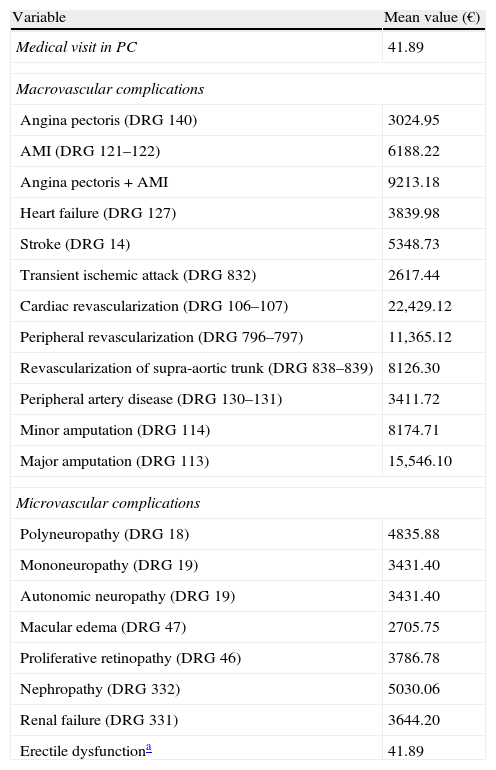
The direct healthcare cost of complications (in € of 2012) was assessed at both hospital level (for diagnosis-related groups [DRGs]) and in primary care. Healthcare resource utilization in primary care, estimated by the expert panel, was calculated as mean values and is summarized in Table 2. The cost of complications was calculated by taking into consideration life expectancy in the overall population12 and its reduction in patients with T2DM.13,14 Unit healthcare costs (drugs, visits, DRGs) were taken from Spanish sources15,16 (Tables 2 and 3).
Utilization of the healthcare resources considered in the economic model.
| Variable | Mean value | References |
| Annual visits to PC for complications of T2DMa | ||
| Angina pectoris | 4.8 | EP |
| AMI | 5.8 | EP |
| Angina pectoris+AMI | 6.4 | EP |
| Heart failure | 7.6 | EP |
| Stroke | 6.2 | EP |
| Transient ischemic attack | 3.7 | EP |
| Cardiac revascularization | 5.1 | EP |
| Peripheral revascularization | 4.4 | EP |
| Revascularization of supra-aortic trunk | 3.9 | EP |
| Peripheral artery disease | 4.5 | EP |
| Minor amputation | 4.0 | EP |
| Major amputation | 4.9 | EP |
| Polyneuropathy | 5.1 | EP |
| Mononeuropathy | 4.3 | EP |
| Autonomic neuropathy | 4.3 | EP |
| Macular edema | 3.5 | EP |
| Proliferative retinopathy | 3.8 | EP |
| Nephropathy | 4.7 | EP |
| Renal failure | 5.3 | EP |
| Erectile dysfunction | 2.0 | EP |
| Mean daily cost of drug treatments in PC for complications of T2DM (€of 2012)b | ||
| Angina pectoris | 0.14€ | EP, 15 |
| AMI | 0.03€ | EP, 15 |
| Angina pectoris+AMI | 0.07€ | EP, 15 |
| Heart failure | 0.10€ | EP, 15 |
| Stroke | 0.07€ | EP, 15 |
| Transient ischemic attack | 0.03€ | EP, 15 |
| Cardiac revascularization | 0.17€ | EP, 15 |
| Peripheral revascularization | 0.11€ | EP, 15 |
| Revascularization of supra-aortic trunk | 0.13€ | EP, 15 |
| Peripheral artery disease | 0.08€ | EP, 15 |
| Minor amputation | 0.10€ | EP, 15 |
| Major amputation | 0.10€ | EP, 15 |
| Polyneuropathy | 0.25€ | EP, 15 |
| Mononeuropathy | 0.25€ | EP, 15 |
| Autonomic neuropathy | 0.26€ | EP, 15 |
| Macular edema | 0.03€ | EP, 15 |
| Proliferative retinopathy | 0.03€ | EP, 15 |
| Nephropathy | 0.09€ | EP, 15 |
| Renal failure | 0.19€ | EP, 15 |
| Erectile dysfunction | 0.25€ | EP, 15 |
PC: primary care; T2DM: type 2 diabetes mellitus; AMI: acute myocardial infarction; EP: expert panel.
Unit costs considered in the economic model (€ of 2012).
| Variable | Mean value (€) |
| Medical visit in PC | 41.89 |
| Macrovascular complications | |
| Angina pectoris (DRG 140) | 3024.95 |
| AMI (DRG 121–122) | 6188.22 |
| Angina pectoris+AMI | 9213.18 |
| Heart failure (DRG 127) | 3839.98 |
| Stroke (DRG 14) | 5348.73 |
| Transient ischemic attack (DRG 832) | 2617.44 |
| Cardiac revascularization (DRG 106–107) | 22,429.12 |
| Peripheral revascularization (DRG 796–797) | 11,365.12 |
| Revascularization of supra-aortic trunk (DRG 838–839) | 8126.30 |
| Peripheral artery disease (DRG 130–131) | 3411.72 |
| Minor amputation (DRG 114) | 8174.71 |
| Major amputation (DRG 113) | 15,546.10 |
| Microvascular complications | |
| Polyneuropathy (DRG 18) | 4835.88 |
| Mononeuropathy (DRG 19) | 3431.40 |
| Autonomic neuropathy (DRG 19) | 3431.40 |
| Macular edema (DRG 47) | 2705.75 |
| Proliferative retinopathy (DRG 46) | 3786.78 |
| Nephropathy (DRG 332) | 5030.06 |
| Renal failure (DRG 331) | 3644.20 |
| Erectile dysfunctiona | 41.89 |
PC: primary care; DRG: diagnosis-related group; AMI: acute myocardial infarction.
Source: Order 629/2009, of 31 August, establishing the public prices for the provision of healthcare services and activities at the network of centers of the Community of Madrid.16
As cost values were not rounded to two decimal places, it should be noted that the results of costs given in the examples below differ from those which would be achieved if the operations were only done with those two decimal places. In the specific case of angina pectoris, the unit cost of an attack (€3693.75) was calculated by adding the costs of DRG 140 (€3024.95),16 primary care visits (€529.58), and drugs used for treatment (€139.22) (the latter two taken from the answers given by the expert group) for 2.7 effective years of visits and drug treatments. This duration was calculated for a life expectancy in Spain of 81.95years, patients with a mean age of 68.8years, and a reduction in life expectancy in T2DM by 10.5years (81.95−68.8−10.5=2.7years).12–14 The total estimated cost of anginal attacks in patients with T2DM in the CM was the result of multiplying the number of anginal attacks (33,621) by the cost of each attack (€3693.75) (€33,621×3693.75€=124,188,336). The total cost of macrovascular complications (€1,065,908,569) was obtained by adding the costs of individual complications.
The cost of macrovascular complications in the CM per patient with T2DM was obtained by dividing the total cost of macrovascular complications (€1,065,908,569) by patients with T2DM (390,944) (€1,065,908,569,390,944=2726.50). The cost of angina per patient with T2DM in the CM (€317.66) was calculated by multiplying the total cost of macrovascular complications per patient (€2726.50) by the frequency of angina among total macrovascular complications (11.7%) (2726.50€×11.7%=317.66€).
Total costs and cost per patient of all other macrovascular and microvascular complications were similarly calculated.
Univariate sensitivity analyses were performed for the minimum and maximum values of the following variables (Table 1): (i) the population with T2DM; (ii) values of prevalence, incidence, and mortality; and (iii) estimated reduction in the life expectancy of patients with T2DM.
As this study included no patient data, approval from an ethics committee was not required.
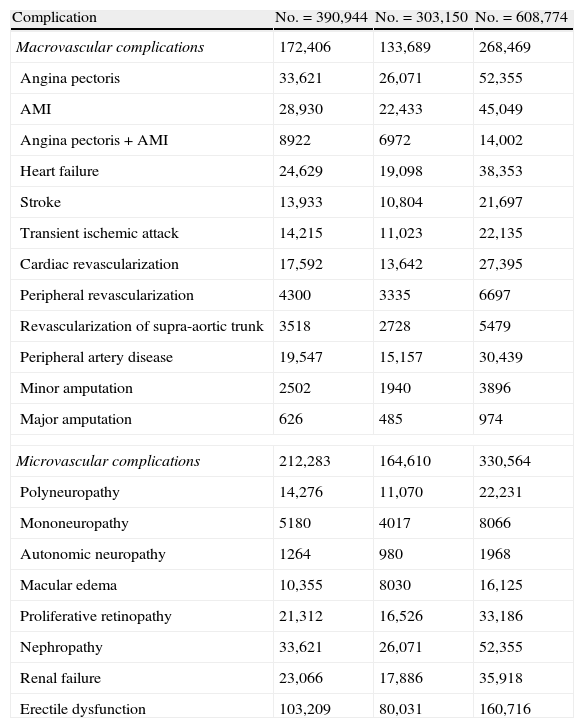
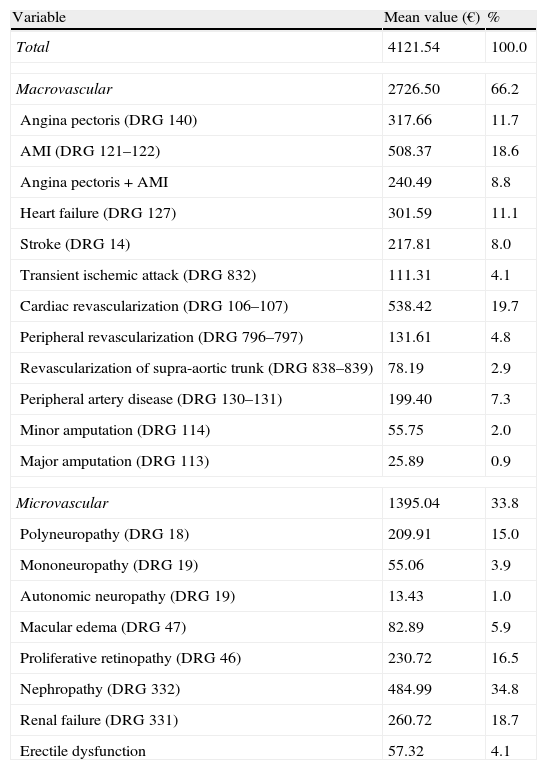
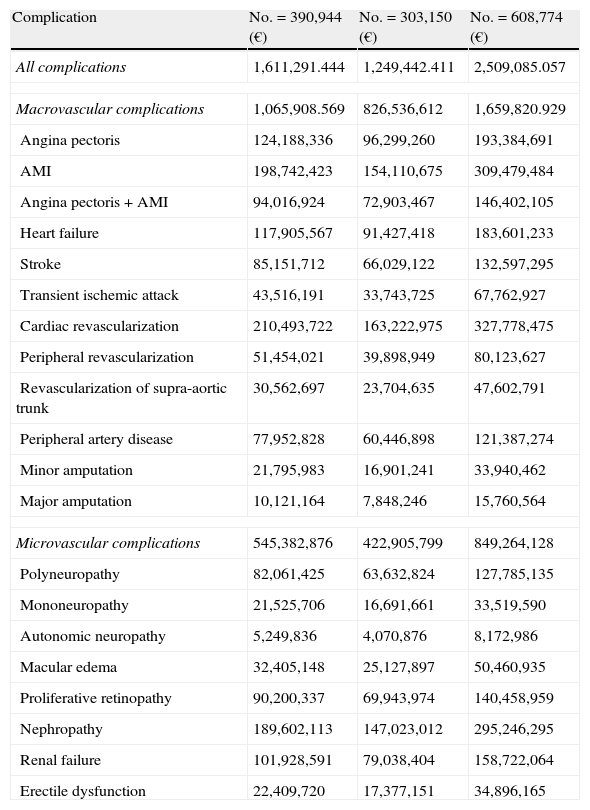
ResultsBase caseThe population with T2DM in the CM was estimated to be 390,944 patients, who experienced during their lifetime 172,406 macrovascular and 212,283 microvascular complications respectively (Table 4). The mean cost per patient of complications of T2DM was calculated as €4121.54 (66.2% due to macrovascular complications) (Table 5). The economic impact of complications of T2DM in the CM was therefore €1611 million (€1065 million due to macrovascular complications and €545 million due to microvascular complications) (Table 6). The greatest expenses resulted from cardiac revascularization (€210 million) acute myocardial infarction (€198 million), and nephropathy (€189 million). The less costly complications were autonomic neuropathy (€5 million) and major amputations (€10 million), as shown in Table 6.
Estimated number of complications that occur in patients with type 2 diabetes mellitus from the Community of Madrid, based on estimates of population size.
| Complication | No.=390,944 | No.=303,150 | No.=608,774 |
| Macrovascular complications | 172,406 | 133,689 | 268,469 |
| Angina pectoris | 33,621 | 26,071 | 52,355 |
| AMI | 28,930 | 22,433 | 45,049 |
| Angina pectoris+AMI | 8922 | 6972 | 14,002 |
| Heart failure | 24,629 | 19,098 | 38,353 |
| Stroke | 13,933 | 10,804 | 21,697 |
| Transient ischemic attack | 14,215 | 11,023 | 22,135 |
| Cardiac revascularization | 17,592 | 13,642 | 27,395 |
| Peripheral revascularization | 4300 | 3335 | 6697 |
| Revascularization of supra-aortic trunk | 3518 | 2728 | 5479 |
| Peripheral artery disease | 19,547 | 15,157 | 30,439 |
| Minor amputation | 2502 | 1940 | 3896 |
| Major amputation | 626 | 485 | 974 |
| Microvascular complications | 212,283 | 164,610 | 330,564 |
| Polyneuropathy | 14,276 | 11,070 | 22,231 |
| Mononeuropathy | 5180 | 4017 | 8066 |
| Autonomic neuropathy | 1264 | 980 | 1968 |
| Macular edema | 10,355 | 8030 | 16,125 |
| Proliferative retinopathy | 21,312 | 16,526 | 33,186 |
| Nephropathy | 33,621 | 26,071 | 52,355 |
| Renal failure | 23,066 | 17,886 | 35,918 |
| Erectile dysfunction | 103,209 | 80,031 | 160,716 |
AMI: acute myocardial infarction.
Mean cost per patient of complications of type 2 diabetes mellitus in the Community of Madrid (€ of 2012).
| Variable | Mean value (€) | % |
| Total | 4121.54 | 100.0 |
| Macrovascular | 2726.50 | 66.2 |
| Angina pectoris (DRG 140) | 317.66 | 11.7 |
| AMI (DRG 121–122) | 508.37 | 18.6 |
| Angina pectoris+AMI | 240.49 | 8.8 |
| Heart failure (DRG 127) | 301.59 | 11.1 |
| Stroke (DRG 14) | 217.81 | 8.0 |
| Transient ischemic attack (DRG 832) | 111.31 | 4.1 |
| Cardiac revascularization (DRG 106–107) | 538.42 | 19.7 |
| Peripheral revascularization (DRG 796–797) | 131.61 | 4.8 |
| Revascularization of supra-aortic trunk (DRG 838–839) | 78.19 | 2.9 |
| Peripheral artery disease (DRG 130–131) | 199.40 | 7.3 |
| Minor amputation (DRG 114) | 55.75 | 2.0 |
| Major amputation (DRG 113) | 25.89 | 0.9 |
| Microvascular | 1395.04 | 33.8 |
| Polyneuropathy (DRG 18) | 209.91 | 15.0 |
| Mononeuropathy (DRG 19) | 55.06 | 3.9 |
| Autonomic neuropathy (DRG 19) | 13.43 | 1.0 |
| Macular edema (DRG 47) | 82.89 | 5.9 |
| Proliferative retinopathy (DRG 46) | 230.72 | 16.5 |
| Nephropathy (DRG 332) | 484.99 | 34.8 |
| Renal failure (DRG 331) | 260.72 | 18.7 |
| Erectile dysfunction | 57.32 | 4.1 |
DRG: diagnosis-related group; AMI: acute myocardial infarction.
Cost of complications that will occur in patients with type 2 diabetes mellitus from the Community of Madrid based on estimates of population size (€ of 2012).
| Complication | No.=390,944 (€) | No.=303,150 (€) | No.=608,774 (€) |
| All complications | 1,611,291.444 | 1,249,442.411 | 2,509,085.057 |
| Macrovascular complications | 1,065,908.569 | 826,536,612 | 1,659,820.929 |
| Angina pectoris | 124,188,336 | 96,299,260 | 193,384,691 |
| AMI | 198,742,423 | 154,110,675 | 309,479,484 |
| Angina pectoris+AMI | 94,016,924 | 72,903,467 | 146,402,105 |
| Heart failure | 117,905,567 | 91,427,418 | 183,601,233 |
| Stroke | 85,151,712 | 66,029,122 | 132,597,295 |
| Transient ischemic attack | 43,516,191 | 33,743,725 | 67,762,927 |
| Cardiac revascularization | 210,493,722 | 163,222,975 | 327,778,475 |
| Peripheral revascularization | 51,454,021 | 39,898,949 | 80,123,627 |
| Revascularization of supra-aortic trunk | 30,562,697 | 23,704,635 | 47,602,791 |
| Peripheral artery disease | 77,952,828 | 60,446,898 | 121,387,274 |
| Minor amputation | 21,795,983 | 16,901,241 | 33,940,462 |
| Major amputation | 10,121,164 | 7,848,246 | 15,760,564 |
| Microvascular complications | 545,382,876 | 422,905,799 | 849,264,128 |
| Polyneuropathy | 82,061,425 | 63,632,824 | 127,785,135 |
| Mononeuropathy | 21,525,706 | 16,691,661 | 33,519,590 |
| Autonomic neuropathy | 5,249,836 | 4,070,876 | 8,172,986 |
| Macular edema | 32,405,148 | 25,127,897 | 50,460,935 |
| Proliferative retinopathy | 90,200,337 | 69,943,974 | 140,458,959 |
| Nephropathy | 189,602,113 | 147,023,012 | 295,246,295 |
| Renal failure | 101,928,591 | 79,038,404 | 158,722,064 |
| Erectile dysfunction | 22,409,720 | 17,377,151 | 34,896,165 |
AMI: acute myocardial infarction.
For populations with T2DM of from 303,150 to 608,774 patients (corresponding respectively to the minimum and maximum values of prevalence, incidence, and mortality), the economic impact ranged from €1249 to €2509 million (Table 6). If the minimum and maximum values of prevalence and incidence are considered, the impact was from €1212 to €2546 million. For the minimum and maximum mortality of T2DM reported in the literature, the impact was from €1648 to €1574 millions. For a six-year reduction in life expectancy in patients with T2DM, the economic impact for the CM was €1974 million.
DiscussionIn our healthcare system, the family physician is usually responsible for the diagnosis, treatment, and monitoring of T2DM, referring patients to the endocrinologist or diabetologist when appropriate, based on referral criteria. Despite the high prevalence and social and health impact of T2DM, most studies available in Spain are cross-sectional and population-based.8 There have been no studies monitoring large cohorts of diabetic patients.
The main limitation of this study, derived from the abovementioned deficiency, is the wide variability of the epidemiological data available on the prevalence, incidence, and mortality of Spanish patients with T2DM.6,7,9 Estimates of the total population of patients with T2DM in the CM are therefore subject to a great variability depending on the epidemiological values under consideration. The study is however robust as regards data on the prevalence of complications of T2DM, as these come from a cross-sectional study conducted on a cohort of 3268 patients from the CM with T2DM.5
It should also be noted that incidence in the CM was estimated using the available data, from Málaga and Asturias,6 which may not have corresponded to the actual incidence of T2DM in the CM. An additional weakness of the study stems from the fact that resource utilization in primary care (number of medical visits and drug treatment used as a consequence of chronic complications of T2DM) was estimated by an expert panel consisting of 21 primary care physicians experienced in the treatment and monitoring of T2DM. These estimates may not correspond to actual healthcare resource utilization.
According to the CODE-2 study, a retrospective study published in 2002,17 the mean annual cost (updated in 2012) of microvascular complications in a Spanish patient with T2DM amounted to €773.17, while the cost of macrovascular complications was €1692.43. The mean age of the Spanish population enrolled into the CODE-2 study was 67.4years. Assuming for patients of that age with T2DM a reduction in life expectancy of 10.5years13,14, they had a mean life expectancy of 4years. The estimated lifetime costs of vascular complications therefore amounted to €3092.68 and €6869.72 for microvascular and macrovascular complications respectively. These lifetime costs from complications of T2DM estimated from the CODE-2 study were higher than those calculated in our study: €1395.04 and €2726.50 for microvascular and macrovascular complications respectively (Table 5). However, the different design of the studies should be taken into account when comparing these results. The CODE-2 study reviewed the clinical histories of 1004 patients with T2DM treated at 29 primary care centers.17 In the present study, healthcare resource utilization was taken from a structured survey completed by 21 primary care physicians. Using the costs of complications by patient estimated from the CODE-2 study, the total cost of complications in the CM amounted to approximately €3600 million (some €2300 million due to microvascular complications and €1300 million due to macrovascular complications).
It should be noted that this study found higher direct population costs from macrovascular complications as compared to microvascular complications, despite the greater prevalence of the latter. This was due to the lower unit costs of microvascular complications (Table 3), resulting in a lower mean cost (Table 5) and, as a consequence, a lower population cost.
Four additional studies on the costs of T2DM in Spain are available.18,19 The López-Bastida et al. study20 assessed the economic impact (direct and indirect costs) of DM in the Canary Islands in 1998. The results of this and our study cannot be compared because of the time elapsed and the global presentation of the results.
The Oliva et al. study21 is not comparable either because it did not provide costs of T2DM, but only the global cost of DM. Another Spanish study, conducted by Ballesta et al.,22 estimated that the direct annual costs of a patient with T2DM were €2504. According to this observational study, the mean cost per patient of macrovascular complications was €2219 (€728–€3710), as compared to €2726 in this study, and the mean cost per patient of microvascular complications was €1943 (€565–€3320), as compared to €1395 in the current study. The results of this study are therefore within the limits of the Ballesta et al. study.22 Finally, the observational study by Costi et al. was intended to assess the direct healthcare costs incurred by patients with T2DM who start insulin therapy in Spain, but it did not estimate the cost attributable to complications of T2DM.23
It is well known that intensive blood glucose control in patients with T2DM of short duration decreases the incidence of vascular complications.24 In this regard, it is interesting to note that therapeutic goals may be inadequately achieved in both primary25 and hospital care.26,27 According to our study, complications of T2DM have a great health and economic impact in the CM, and should therefore be considered both in healthcare assessment and budget calculation. In order to delay the occurrence of chronic complications of T2DM and thereby decrease the healthcare costs associated with them, we recommend that programs intended to intensify therapeutic intervention to optimize blood glucose control in poorly controlled patients with T2DM be devised, and that actions aimed at the early diagnosis and treatment of cardiovascular risk factors be increased.3,27 In this regard, we would like to see further studies in which the costs are directly calculated for the population being cared for.
Conflicts of interestThis study was conducted with a research grant from Sanofi Spain. Ana Magaña is a former employee of Sanofi Spain; Carlos Rubio-Terrés has received honoraria from Sanofi Spain in relation to this article; all the other authors state that they have no conflicts of interest with this study.
Study funded by the Spanish Agency for Biosanitary Research of Instituto Carlos III P08/90596, PS09/00680 with the collaboration of Sanofi.
A.M. Arias-Salgado (C.S. Ciudad Jardín); J. Camalda (C.S. Águilas); L.M. Campos (C.S. Avenida de Aragón); J.R. Carravilla (C.S. Águilas); C. Casado (C.S. General Ricardos); M.C. Chilcon (C.S. Águilas); C. Debán (C.S. Restón); M.S. Gómez (C.S. General Ricardos); M.J. Gónara (C.S. Las Cortes); A.M. Herranz (C.S. Alameda de Osuna); R. Iglesias (C.S. Pedro Laín Entralgo); B. de Llones (C.S. Entrevías); M.S. Mayayo (C.S. Martín de Vargas); G. Mora (C.S. Alpes); P. Nogales (C.S. Águilas); B. Novella (C.S. Potosi); M. Sanz (C.S. Águilas); J. Sierra (C.S. Águilas); J. Vázquez (C.S. Águilas).
Please cite this article as: Arrieta F, Rubio-Terrés C, Rubio-Rodríguez D, Magaña A, Piñera M, Iglesias P, et al. Estimación del impacto económico y sanitario de las complicaciones de la diabetes mellitus tipo 2 en la Comunidad de Madrid. Endocrinol Nutr. 2014;61:193–201.
The names of the members of the Study Group on Diabetes, who have collaborated in this study are listed in Annex 1.