To assess the clinical characteristics of patients with Charcot neuroarthropathy (CN) in Spain and to identify predictors for CN-related complications.
Patients and methodsA retrospective study was conducted at five tertiary hospitals with diabetic foot care units in Spain. Data were collected from 83 patients, including demographic profiles, foot factors, diabetes characteristics, and presence of microvascular and macrovascular comorbidity, and a podiatric examination was also performed. Logistic regression analyses were used to determine significant predictors of the predefined clinical events.
ResultsSigns of diabetic neuropathy were found in almost all patients (98.9%) at the initial assessment, approximately half of them had diabetic retinopathy or nephropathy (61.5% and 51.8%, respectively), and peripheral artery disease was uncommon (8.6%). Thirty-eight patients (47.5%) experienced one or more relevant clinical events: 22 (27.5%) a new foot ulcer; 7 (8.7%) a major amputation; 20 (25%) were admitted to hospital; and 4 (5%) died. Only the presence of diabetic nephropathy was independently associated to development of any of the complications studied (p = 0.009; odds ratio = 3.37; 95% CI: 1.12-10.1).
ConclusionsAlmost half the patients with CN attending specialised foot care units in tertiary hospitals experienced short-term CN-associated complications, and the risk was 3 times higher in those with a history of diabetic nephropathy.
Determinar las características clínicas de pacientes con neuroartropatía de Charcot (NC) en España e identificar predictores de complicaciones relacionadas.
Materiales y métodosEstudio retrospectivo llevado a cabo en 5 hospitales terciarios de España con unidad de pie diabético. Se recopilaron datos de 83 pacientes incluyendo perfil demográfico, datos provenientes de la exploración podológica, características de la diabetes y presencia de comorbilidad micro y macro vascular. Para determinar los predictores significativos de acontecimientos clínicos predefinidos se utilizaron análisis de regresión logística.
ResultadosCasi todos los pacientes (98,9%) tenían signos de neuropatía diabética en la evaluación inicial, aproximadamente la mitad tenían retinopatía o nefropatía diabética (61,5 y 51,8%, respectivamente) y la enfermedad arterial periférica era infrecuente (8,6%). Treinta y ocho pacientes (47,5%) experimentaron uno o más acontecimientos clínicos relevantes: 22 (27,5%) una nueva úlcera en el pie, 7 (8,7%) una amputación mayor, 20 (25%) fueron hospitalizados y 4 (5%) murieron. Solamente la presencia de nefropatía diabética se encontró independientemente asociada al desarrollo de alguna de las complicaciones estudiadas (p = 0,009; odds ratio = 3,37; 95% CI: 1,12-10,1).
ConclusionesCasi la mitad de los pacientes con NC atendidos en unidades de cuidado del pie diabético en hospitales terciarios experimentaron complicaciones asociadas a NC a corto plazo, y el riesgo entre aquellos sujetos con historia de úlcera previa era 3 veces mayor.
Charcot neuroarthropathy (CN) is an uncommon, but one of the most severe and devastating, complications of diabetic foot (DF) disease, characterised by important foot deformity and a lack of the protective sensation of pain. The current accepted theory is that uncontrolled inflammation is central to the pathophysiology of CN, where somatosensory and autonomic neuropathy trigger the release of proinflammatory cytokines and interleukins.1–3 This activates the nuclear transcription factor-kappa ß, which results in an osteoclast-osteoblast imbalance, and leads to local bone resorption, in turn facilitating progressive joint dislocation and microfractures of the pedal skeleton.1–3
There are few available extensive studies on the prevalence of CN, but estimates from population-based studies range between 0.1% and 8% of patients with diabetes,4–8 it is higher (13%) in patients presenting at specialised foot clinics,9 and the prevalence of radiographic changes in patients with established diabetic neuropathy ranges between 10% and 29%.10–13 There are several prospective studies on the incidence of CN, with figures varying widely between 0.1 and 29% per year.14–16 However, these are probably underestimations because the early presentation of CN may be overlooked or mistaken for other conditions (e.g., infection, osteomyelitis, cellulitis, or other neuropathies), and, as a consequence, diagnosis is often delayed (up to 29 weeks) or even missed in a high proportion of cases (up to 79%).14,17,18
CN is more frequent in patients in their fifth or sixth decade of life, and occurs most commonly in patients with long-standing diabetes (both type 1 and type 2) (i.e., >10 years). Other risk factors include diabetic neuropathy, elevated glycosylated haemoglobin (HbA1c), overweight, diabetic nephropathy, and decreased bone density.14–16,18,19 In addition, CN is associated with significant morbidity, as progression of the disease is associated with joint deformity and instability of the foot, skin ulcers, infection, high rates of hospitalisation, an increase in the risk of amputation,14–16,18,19 and in some studies also increased mortality.20–23 Finally, high rates of severe coronary plaques and a lower survival among CN patients with coronary artery disease have been reported.23,24
Although considerable studies have been devoted to assess risk factors for the development of CN, rather less attention has been paid to the risk of further associated complications and prognostic factors. Nevertheless, these are key for expert management and appropriate intervention in order to reduce or prevent its progression and further outcomes such as ulceration, major lower extremity amputation, hospitalisation or even death. The aim of the present study was to contribute to existing knowledge through the assessment of clinical characteristics and risk factors for short-term patient-oriented relevant outcomes among patients with Charcot foot disease attended at specialised diabetic foot care clinics from tertiary hospitals in Catalonia, a North-eastern area of Spain.
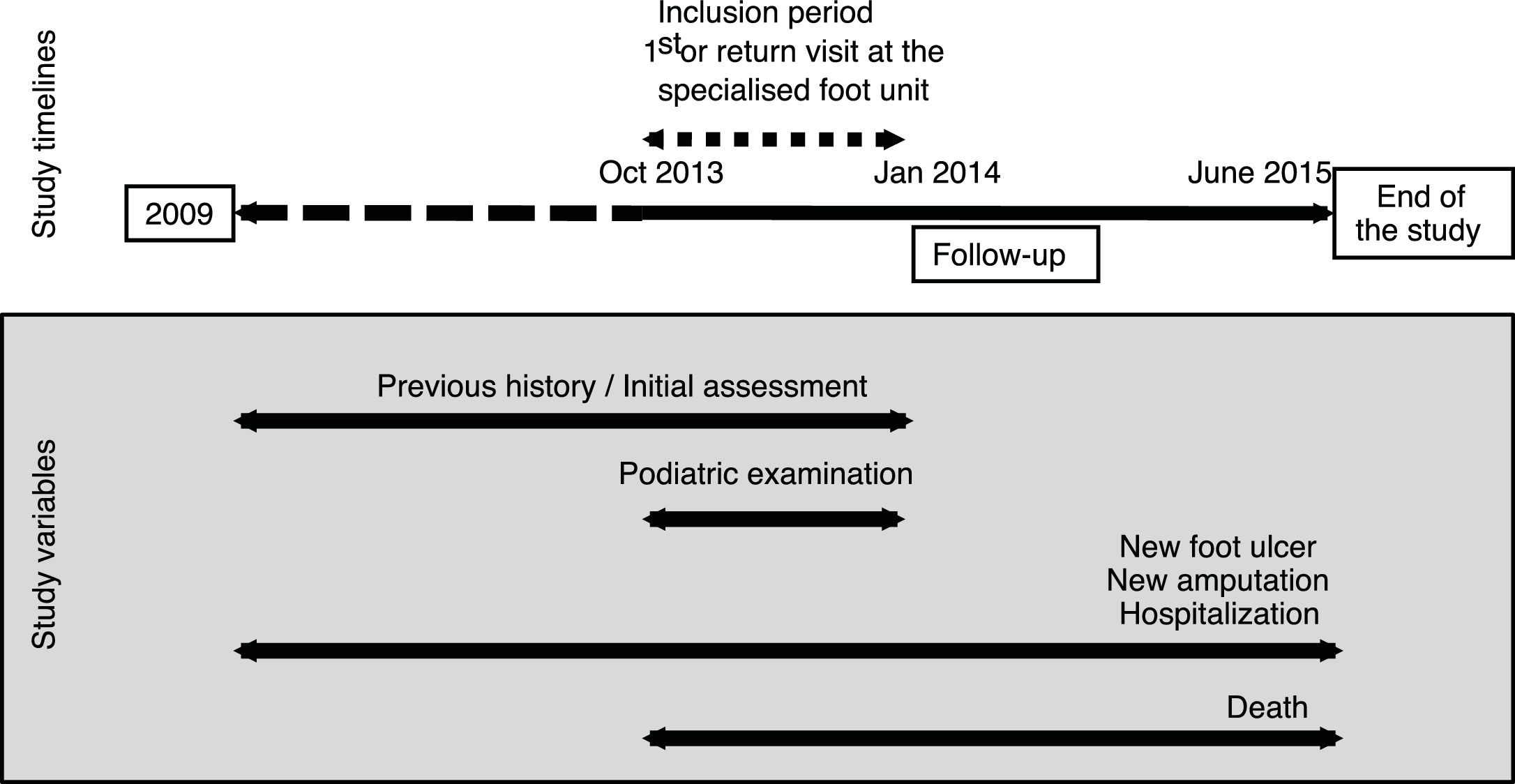
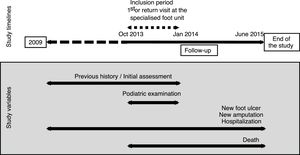
Materials and methodsDesign and settingThis was a, multicentre study conducted at 5 tertiary hospitals with a dedicated diabetic foot care clinic in Catalonia, Spain. We included patients who visited the clinic for the first time and were diagnosed with initial episodes of acute CN, and also patients with chronic CN previously managed at the clinic (starting in 2009) presenting with any new concomitant foot complications (Fig. 1). Patients were included between October 2013 and January 2014, and followed for further complications until June 2015.
The local Ethics Committee from each participating hospital approved the protocol, and all patients signed a written informed consent form prior to participation. The study was conducted in accordance with the Declaration of Helsinki (1964).
Studied variablesTo facilitate consistency in clinical examinations and data collection across participants and study sites, a case report form template was developed and agreed among all participant centres.
At the time of the inclusion, all patients (both chronic and acute CN) underwent an initial visit performed by an experienced specialised clinician to collect clinical information and to conduct a podiatric examination. Clinical information included the following variables: (a) the date of the current visit for acute patients, and the date of the first visit to the clinic for chronic patients, considering only the first episode for those with bilateral disease; (b) demographic variables (i.e., sex and age); (c) height; (d) body mass index; (e) type of Charcot (i.e., acute or chronic if one feet affected, or bilateral if both); (f) duration of CN symptoms (for acute cases); (g) type and duration of diabetes mellitus (DM) when applicable, and most recent (within the previous 6 months) HbA1c value; and (h) previous diagnoses, including arthropathy, osteomyelitis, cellulitis, deep vein thrombosis, gout, acute arthritis, psoriatic arthritis, osteoarthritis, and bone tumours. Moreover, the presence of comorbid chronic complications included the assessment of: (a) diabetic neuropathy, defined as abnormal findings in the neurological examination of both feet by means of the 5.07 Semmes-Weinstein monofilament test and tuning fork (128Hz) according to the current consensus of the International Working Group on the Diabetic Foot (IWGDF)25; and (b) of peripheral artery disease (PAD), defined as the absence of any of the pedal or posterior tibial pulses. In addition, data on the following comorbid conditions was supplemented with clinical records of the hospital database: diabetic retinopathy was considered if diagnosed by an experienced clinician; diabetic nephropathy was defined as the presence of albuminuria (>30μg/g creatinine) and/or creatinine >1.3mg/dl and/or glomerular filtration rate below 60ml/min/1.73m2 during the prior year; coronary heart disease if confirmed by pathological findings in an ergometry or coronary angiography; history of myocardial revascularisation procedure or a recorded clinical diagnosis of coronary heart disease; and cerebrovascular disease, defined as any diagnosis of previous stroke.
Regarding the podiatric examination at the inclusion visit, the assessment of acute phase CN included the following clinical signs and symptoms: localised unilateral swelling, erythema, warmth, pain, increased temperature (>2°C compared to contralateral foot), deformities, and diabetic neuropathy of the affected foot. An ulcer was considered when a sore extended through the full thickness of the skin on the foot below the ankle. The assessment of clinical signs of chronic phase CN included foot deformities associated with old signs and symptoms of the acute phase or a history of surgical procedures for CN correction. Moreover, all patients underwent X-ray imaging to assess radiographic signs characteristics: for CN acute phase, these included osteopenia and osteolysis, subchondral bone damage, dislocations, subluxations, and bone fractures; for chronic patients, the presence of bone fragmentation, fusion or consolidation. All images were electronically sent to one of the participating centres, where a trained radiologist reviewed and confirmed radiographic findings. Finally, for chronic patients, we retrospectively collected data from hospital records regarding the history of previous amputations, which were classified as minor (defined as any amputation below the ankle) or major (all other types), and we also considered the presence of a previous foot ulcer when located below the ankle joint as a result of DM.
The following predefined outcomes were retrospectively collected at the end of the study (15th June 2015) through the hospitals’ databases for all included patients: presence of a new ulcer, new major amputation, and hospitalisation or death of any cause. For acute CN cases, a new outcome or death necessarily happened during the period between the inclusion period (October 2013–January 2014) and the end of the study, while for chronic CN patients a new outcome (except death) could as well have happened before the inclusion period. In all cases, the date of the first newly diagnosed event after the initial CN diagnosis was considered.
Statistical analysisA descriptive analysis was performed using percentages for categorical variables and mean and standard deviations (SD) for continuous variables. We analysed the association of all variables (i.e., age, gender, type and duration of DM, HbA1c, chronic diabetes complications, Charcot type, amputations, and previous foot ulcer) with different predefined outcomes or complications of CN (dependent variables, namely new foot ulcer, major amputation, hospitalisation, death, or a composite of any of these) by the Chi-square test or Fisher exact test to compare proportions and the Mann–Whitney U test to compare distributions of continuous factors. To determine significant predictors of the predefined outcomes we computed crude and adjusted odds ratios (ORs) with 95% confidence intervals (CIs) using a simple logistic regression analysis. The bivariate analyses included the following variables: gender, diabetes type, diabetic retinopathy, diabetic nephropathy, previous ulcer, previous amputation, Charcot type (acute, chronic or bilateral), and data (recorded as present or absent) from the podologic exploration at the initial visit: limb oedema, limb erythema, diabetic neuropathy, distal pulses, pain, deformity/biomechanical changes, infection, and probe-to-bone test. Finally, we used an adjusted model (multiple logistic regression analysis) including all statistically significant variables (p<0.05) in the bivariate analysis and potential confounders (i.e., age, diabetes duration, and history of cardiovascular disease). All statistical analyses were performed using SPSS software package (version 15.0, IBM Corp., Armonk, NY, USA).
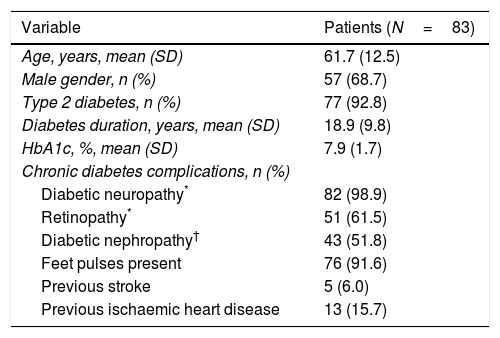
ResultsA total of 83 patients with CN were included in the study. Baseline demographic and clinical characteristics of the study participants are shown in Table 1. The mean age was 61.7 years (SD=12.5) and the percentage of males was 68.7%. The vast majority of patients had type 2 DM (92.7%), with mean diabetes duration of 18.9 years (SD=9.8) and a mean HbA1c value of 7.9% (SD=1.7).
Baseline demographic and clinical characteristics of the study population.
| Variable | Patients (N=83) |
|---|---|
| Age, years, mean (SD) | 61.7 (12.5) |
| Male gender, n (%) | 57 (68.7) |
| Type 2 diabetes, n (%) | 77 (92.8) |
| Diabetes duration, years, mean (SD) | 18.9 (9.8) |
| HbA1c, %, mean (SD) | 7.9 (1.7) |
| Chronic diabetes complications, n (%) | |
| Diabetic neuropathy* | 82 (98.9) |
| Retinopathy* | 51 (61.5) |
| Diabetic nephropathy† | 43 (51.8) |
| Feet pulses present | 76 (91.6) |
| Previous stroke | 5 (6.0) |
| Previous ischaemic heart disease | 13 (15.7) |
HbA1c, glycated haemoglobin; SD, standard deviation.
Regarding chronic complications, diabetic neuropathy was the most frequent condition and was present in almost all patients (98.9%) at initial assessment, and about half of them had retinopathy or diabetic nephropathy (Table 1). However, PAD was infrequent, and distal feet pulses were present in almost all patients.
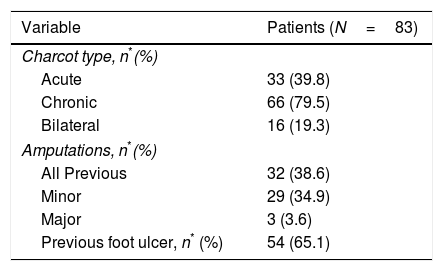
Regarding CN characteristics, most patients were classified as chronic (79.5%), and 19.3% had bilateral disease (Table 2); a history of amputations was present in 38.5% of patients, the majority of them minor, and more than half of patients had a history of previous foot ulcer.
At the end of the study, data on predefined outcomes (namely new ulcer, major amputation, hospitalisation, death or a composite of any of these) were available for 80 patients. The mean time to death or last clinical visit was 1.8 years (SD=1.6), and the mean follow-up time for unilateral or bilateral chronic CN cases was 3.1 years (SD=1.7). Thirty-eight patients (47.5%) experienced at least one or more of the predefined relevant outcomes: 22 (27.5%) a new foot ulcer; 7 (8.7%) a major amputation; 20 (25%) were admitted at a hospital for any reason; and 4 (5%) died. There were no significant differences between any of the demographic or clinical characteristics and the predefined outcomes or complications of CN.
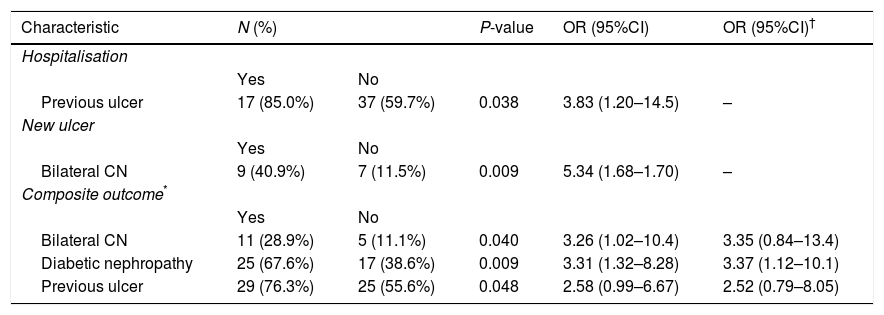
From the bivariate analysis (Table 3; Supplementary Table), the only variables significantly associated with an increased risk of a particular outcome were a previous ulcer, which was associated with a higher risk of hospitalisation, (OR=3.83; 95% CI=1.20–14.5), and bilateral CN, which was associated with an increased likelihood of developing a new ulcer (OR=5.34; 95% CI=1.68–1.70). Moreover, a previous ulcer, bilateral CN or diabetic nephropathy were predictors of the development of a composite of any of the studied complications. None of the factors were associated with amputation or mortality. Finally, the multivariate analysis (Table 3) showed that only the presence of diabetic nephropathy was independently associated with the development of the composite of any of the outcomes studied (p = 0.009; odds ratio = 3.37; 95% CI: 1.12-10.1).
Bivariate (only significant predictors are shown) and multivariate analysis for factors associated with relevant outcomes.
| Characteristic | N (%) | P-value | OR (95%CI) | OR (95%CI)† | |
|---|---|---|---|---|---|
| Hospitalisation | |||||
| Yes | No | ||||
| Previous ulcer | 17 (85.0%) | 37 (59.7%) | 0.038 | 3.83 (1.20–14.5) | – |
| New ulcer | |||||
| Yes | No | ||||
| Bilateral CN | 9 (40.9%) | 7 (11.5%) | 0.009 | 5.34 (1.68–1.70) | – |
| Composite outcome* | |||||
| Yes | No | ||||
| Bilateral CN | 11 (28.9%) | 5 (11.1%) | 0.040 | 3.26 (1.02–10.4) | 3.35 (0.84–13.4) |
| Diabetic nephropathy | 25 (67.6%) | 17 (38.6%) | 0.009 | 3.31 (1.32–8.28) | 3.37 (1.12–10.1) |
| Previous ulcer | 29 (76.3%) | 25 (55.6%) | 0.048 | 2.58 (0.99–6.67) | 2.52 (0.79–8.05) |
CI, confidence interval; CN, Charcot neuroarthropathy; OR, odds ratio.
The study showed that patients with CN in our setting were in most cases chronic at the time that they were referred to specialised foot care clinics, almost all of them were type 2 diabetic subjects, and a high proportion had some type of comorbid condition, mainly diabetic neuropathy. A history of a previous foot ulcer was the only factor independently associated with the probability to experience any of the studied short-term CN-related complications, namely a new foot ulcer, a major amputation, hospitalisation or death.
The baseline demographic characteristics of our study population, with a high proportion of men, in their sixties, with type 2 diabetes of long duration, and suboptimal glycaemic control, support previous findings that have identified all of them as risk factors for the development of CN.14,18,19 Moreover, more than half of the included patients had concomitant diabetes-associated microvascular complications such as retinopathy or diabetic nephropathy, and diabetic neuropathy was present in 99% of patients. All together, these results are consistent with the literature, and add to the evidence that long-lasting diabetes is key in the development of CN.14,18,19 The frequency of PAD in our sample was low (8.4% of patients) and, although rarely explored in CN patients, it was much less prevalent than previously reported (34–40%).23,26 Differences may be attributable to different assessment procedures, as we determined PAD by manual palpation of both pedal pulses, but we did not use more accurate measurements such as Doppler ultrasound, and we could have therefore missed less severe forms of vascular insufficiency. This is because this was a retrospective study and the data on Doppler explorations were lacking for a high number of patients. However, another study only using pulsation of pedal arteries found a much lower percentage of PAD (1%) among Danish CN patients.4
Regarding the characteristics of CN, about 80% of our sample had a chronic form of the disease when they were recruited, 65% had developed a previous foot ulcer, and almost 40% a previous amputation. The fact that a high proportion of cases were chronic is not unexpected given that the activity of the disease is usually prolonged and that the diagnosis was delayed before patients were referred to a specialised foot care clinic, and therefore not active as defined by usual clinical signs.15 The frequency of preceding foot ulcers in our study is in line with the 65% described by Sohn et al. in a sample of about 1000 incident CN patients followed for 5 years in the UK,21,27 and also close to the 70% recently described in a smaller sample of 85 CN patients from the US.26 Of note, and also in agreement with the high proportion of chronic patients in our sample, the proportion of previous foot ulcers almost halves to 35% when only considering acute CN cases.28 The proportion of patients with a history of amputations in our study, at 40%, is between the 28.7% and 51.3% previously reported,4,23 although the frequency of major amputations in our sample (3.6%) was slightly higher than in these 2 previous studies (less than 2%). Disparities between studies may be attributable to differences in sample size and duration of follow-up.
The proportion of CN-associated new foot ulcers in our sample was 27.5%, and was complementary to other studies that found an incidence between 25% and 50%,21,23,27–29 a frequency varying as a function of the type of patients studied, with the lowest incidence reported among acute CN patients,29 and duration of follow-up, with the highest incidence corresponding to a study following subjects for 15 years.23 The frequency of amputations during our study period was 8.7%, which is between the 1.8% and 13.5% reported by the few available studies with data on this variable.4,23,27 Again, differences between studies may be attributable to the proportion of acute/chronic patients studied and the length of the observation period. In addition, the rates of hospitalisation and mortality in our study were 25% and 5%, respectively. While to our knowledge there are no available studies to be compared with our proportion of hospital admissions, results on mortality have shown rates ranging between 1.7% and 44.7%,4,20–23,29,30 a wide range mainly dependent on the length of the follow-up time.
Although several studies on risk factors for the development of CN are available, the risk of further associated complications has been given much less attention and has not been studied at large. The results of our multivariate analysis showed that only diabetic nephropathy was independently associated with a more than 3-fold higher risk for any further complication of CN (new foot ulceration, major amputation, hospitalisation or death). In the study of Sohn et al.,27 patients with CN and a concomitant foot ulcer had 12 times more risk of lower extremity amputation than patients with CN alone, and the risk increased to 13-fold among subjects >65 years. In an independent study,23 risk factors for minor amputations included diabetic retinopathy and PAD, and the risk for major amputations was increased in patients with a history of previous minor or major amputations or coronary heart disease. Finally, a study conducted by Sämann et al. in acute CN cases found diabetic nephropathy as an independent risk factor for foot outcomes and related major complications (namely foot deformities, plantar ulcers, and amputations).29 The design of the Sämann study is similar to ours as it included a composite of outcomes, and in our bivariate and multivariate analysis diabetic nephropathy was also associated with any of the studied CN outcomes (which included re-ulcerations and major amputations).
Regarding the risk of mortality among CN patients, studies have been scarce and inconclusive: an increased mortality rate among patients with CN compared with patients with uncomplicated neuropathic ulceration was first described as higher than expected by Gazis et al.20 The work published by Sohn et al.21 found an increased mortality risk for both patients with CN and diabetic foot ulcer (DFU) compared with diabetes alone, a risk that in the case of CN was associated regardless of the presence of ulcers or other comorbidities. A further study by Van Baal et al.22 compared associated mortality in acute phase CN patients vs. patients with uninfected neuropathic foot ulcers and healthy controls, and reported that, although there was no difference in the survival rate between the two patients’ groups, mortality was higher among subjects with coexisting renal dysfunction, and life expectancy was lower for both conditions combined compared to the general population. However, a recent prospective observational report studying foot complications and mortality in patients with diabetes found that neither CN nor DFU had an independent effect on mortality in fully adjusted models, and only lower extremity amputation was a predictor of increased risk of death.30 Of note, CN patients with diabetic neuropathy have been reported to have a higher prevalence of severe coronary plaques compared with those without CN,24 and coronary artery disease has been identified as the only independent predictor of survival among type 2 diabetes patients with CN.23
The main strength of the study is that it was conducted at 5 different specialised diabetic foot care units, with a low percentage of losses (3.6%) during follow-up. However, patients were recruited from tertiary reference hospitals that may not reflect patients attended at community diabetic foot centres. This could have in turn resulted in selection bias because of the inclusion of diabetic patients attended at the hospital, probably bearing a higher morbidity than average diabetic population, or because they presented a severe form of Charcot at presentation. Another limitation of the study is its retrospective design, inherently subject to incorrect documentation and loss of data concerning those variables that were extracted from medical records. Moreover, the results must be interpreted with caution because of the joint analysis of acute and chronic CN patients, which implies that foot care might have been different between the two populations and impacted the incidence of new outcomes. In addition, the relatively small sample, mainly because of the limited available population with this condition, may have reduced the statistical power of the study. Finally, the short follow-up period may have lead to an underestimation of the incidence of some CN-related outcomes and complications in some patients.
ConclusionsThe results show that most patients with CN attended at specialised diabetic foot care units in our area had a chronic form of the disease. About half of the patients experienced at least one short-term CN-related complication, namely a new foot ulcer, major amputation, hospitalisation or death. Moreover, patients with diabetic nephropathy had three fold increased risk for any further complication. These results underline the importance of lifelong foot care in this devastating complication of diabetic foot disease.
FundingThis study was partially supported by Institut Universitari d’Investigació en Atenció Primària Jordi Gol (IDIAP Jordi Gol). The funding source had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript.
Conflicts of interestThe authors declare that they have no conflict of interest associated regarding the publication of this article.
The authors thank the patients who participated in the study and Mònica Gratacòs and Amanda Prowse for providing support in the manuscript preparation and editing. CIBER of Diabetes and Associated Metabolic Diseases (CIBERDEM) is an initiative from Instituto de Salud Carlos III (Plan Nacional de I+D+I and Fondo Europeo de Desarrollo Regional [FEDER]). This project was developed in the context of the programme “Doctorat en Medicina de la Universitat Autònoma de Barcelona” Autonomous University of Barcelona.