To describe the prevalence of known and ignored type 2 diabetes mellitus (T2DM) among primary care physicians (PCP), as well as the treatment used and the degree of metabolic control reached.
Material and methodsDescriptive cross-sectional study on national level. The participants were randomly selected PCPs, members of the redGDPS Foundation. A total of 495 PCP were enrolled. Capillary HbA1c measurement was done with a A1CNow+® device and a diabetes-related survey specifically designed for the study was administered to the participants.
ResultsThe total prevalence of T2DM was 11.1% (95% CI 8.33–13.9) (known disease 8.1% and ignored disease 3.0%). The prevalence of prediabetes was 16.2% (95% CI 13.0–19.4). A total of 62.5% of PCPs with known T2DM reached HbA1c<7% and 15% had HbA1c>8.5%. Control of blood pressure (BP<140/90mmHg) was reached in 87.5% and control of LDL cholesterol<130mg/dl with no history of cardiovascular disease was reached in 88.6% of cases of known T2DM. In the PCPs with a history of macrovascular disease, good control of LDL was reached in 42.9% of the cases. A total of 12.5% were active smokers. A total of 71.4% of PCPs with known T2DM self-treated their own disease, usually with 2 or more drugs (51.4%). The most commonly used drug was metformin (74.3%) followed by iDPP4 (48.6%).
ConclusionsPCPs with T2DM have better metabolic control than the general population. It is necessary to study whether PCPs with T2DM may have greater adherence to treatment and do they achieve a better metabolic control.
Describir la prevalencia de la diabetes mellitus tipo 2 (DM2) conocida e ignorada entre los médicos de Atención Primaria (MAP), así como el tratamiento utilizado y el grado de control metabólico.
Material y métodosEstudio descriptivo transversal de ámbito nacional. Fueron elegidos 495 MAP aleatoriamente entre los médicos afiliados a la Fundación redGDPS. A todos se les determinó la HbA1c capilar con dispositivo A1CNow+® y se les aplicó una encuesta específicamente diseñada para el estudio.
ResultadosLa prevalencia total de DM2 fue del 11,1% (IC 95% 8,33-13,9) (8,1% con DM2 conocida y 3,0% con DM2 ignorada) y del 16,2% para la prediabetes (IC 95% 13,0-19,4). El 62,5% de los MAP con DM2 conocida alcanzan cifras de control de la HbA1c<7% y el 15% tienen cifras superiores a HbA1c>8,5%. El control tensional (PA<140/90mmHg) se alcanza en el 87,5% y el control del colesterol LDL<130mg/dl sin antecedentes de enfermedad cardiovascular es alcanzado por el 88,6% de los casos de DM conocida, y si existen antecedentes de enfermedad macrovascular, el LDL<100mg/dl solo se alcanza en el 42,9% de los casos. El 12,5% son fumadores activos. El 71,4% de los MAP con DM conocida se autotrataban su propia enfermedad, habitualmente con 2 o más fármacos (el 51,4%). El fármaco más utilizado era la metformina (74,3%), seguido por los iDPP4 (el 48,6%).
ConclusionesLos MAP con DM2 tienen un control metabólico algo mejor que la población general. Es necesario estudiar si los pacientes de MAP con DM2 pueden tener una mayor adherencia al tratamiento y alcanzar un mejor control metabólico.
Type 2 diabetes mellitus (DM2) has become one of the most serious health problems of our time.1 A number of population-based epidemiological studies have been carried out in different regions in Spain to evaluate the prevalence of diabetes and glucose intolerance. These investigations yielded a prevalence of DM2 of between 6 and 10%.2 The above data was updated by a large national epidemiological study (di@bet.es) published in 2012.3 The information obtained from the di@bet.es study reveals a global prevalence of diabetes of 13.8% in the adult population (7.8% with known diabetes and 6% with unknown disease).
Since 2010, the recommendations of the American Diabetes Association (ADA) accept the diagnosis of diabetes with glycosylated hemoglobin (HbA1c) values of ≥6.5%, and define prediabetes as HbA1c between 5.7 and 6.4%.4 On the other hand, the control of blood glucose and all other associated factors is required to prevent the potential complications of the disease. The degree of blood glucose control must be established on an individualized basis, though in most patients a glycosylated hemoglobin concentration of over 7% is indicative of the need for intervention or treatment change,5 generally indicated by the health professional responsible.
The health of primary care physicians (PCPs) is relevant from the sociosanitary perspective, not only due to the personal consequences but also because it has a direct impact upon the quality of care received by their patients. There is evidence that patients are observant of the health habits of physicians,6 while physicians with healthy personal habits are in turn more liable to discuss preventive behavior with their patients.7 The current evidence referring to the health of healthcare professionals is limited and is mainly centered on cardiovascular health and risk factors.
A number of other issues also generate interest, such as knowledge of the degree of self-management, control of the disease or therapeutic inertia among PCPs, which may be different from the practices the physicians apply to their patients.
This study was therefore designed with the primary objective of determining the prevalence of T2DM in Spanish PCPs, as well as their blood glucose control, degree of self-management, and the presence or absence of therapeutic inertia in this population.
Material and methodsThe PRISMA study was a cross-sectional, descriptive, epidemiological analysis of PCPs with a professional practice in Spain.
The primary study objective was to ascertain the prevalence of T2DM in PCPs. As secondary objectives, the study aimed to determine the degree of blood glucose control (based on HbA1c) and control of the associated cardiovascular risk factors among the PCPs, as well as their treatment and therapeutic approach to their own blood glucose control levels. The presence of complications specific to diabetes was also explored. In addition, the study aimed to determine the prevalence of prediabetes in this population.
The study comprised PCPs of both sexes aged 45 years and over with a professional practice in Spain, randomly selected from among the 5212 physicians listed on the website of the redGDPS Foundation (Fundación redGDPS—network of Diabetes Study Groups in Primary Care) (www.redgdps.org). This was created in 1998 to promote training in diabetes and the study of the disease among primary care health professionals, with a view to improving the quality of patient care.
Other known types of diabetes, such as type 1 diabetes, latent autoimmune disease, adult disease in young patients, and gestational or secondary diabetes were considered exclusion criteria. Individuals with hematological or other disorders capable of interfering with HbA1c measurement were also excluded.
Sample size calculation was based on the attainment of the primary objective of the study. We estimated an age- and gender-adjusted prevalence of diabetes mellitus (DM) in Spain of 13.8%, with a 95% confidence interval (95%CI) of 12.8–14.7.3
Assuming an alpha risk of 0.05 and a beta risk of 0.20 (statistical power of 80%) in two-tailed tests, a random sample of 496 PCPs was needed to determine the prevalence in that population with a precision of ±4.5. The calculation contemplated the possibility of simple random replacement in the event of losses. A total of 64 of the selected physicians (12.9%) declined to participate in the study and were replaced by the next professionals on the random list. The age and sex distribution of the non-participants was not significantly different from that of the overall sample.
The particularity of this study was that the investigating physician collected his or her own personal data after verifying that the screening criteria defined by the study protocol were met. Each physician received a device for the quantitative determination of percentage HbA1c in capillary blood (A1Cnow+®), thereby ensuring homogeneity in the assessment of HbA1c as the primary endpoint of the study.
The main variables analyzed were:
- •
Capillary HbA1c concentration. The prevalence of T2DM was calculated from the already known diagnosis of diabetes which some physicians could have or, alternatively, from an HbA1c value of ≥6.5%, confirmed by a second test according to the recommendations of the American Diabetes Association.5 “Prediabetes” in turn was defined as HbA1c 5.7–6.4%.
- •
Demographic data on the clinical practice of the physician: urban or rural setting, years of professional activity, residency training.
- •
The presence of hyperglycemia and of all other cardiovascular risk factors (high blood pressure [HBP], dyslipidemia, obesity, smoking), their treatment, and their degree of control.
- •
A history of cardiovascular disease and other chronic complications of T2DM. The presence of hypoglycemic episodes in the previous 6 months.
- •
The value of the last basal blood glucose measurement, lipid profile, glomerular filtration rate (estimated using the MDRD equation), and liver function documented in the case history (all made within the previous year).
- •
Self-control and self-analysis of the disease using test strips.
- •
Drug treatment of hyperglycemia among physicians with diabetes.
The statistical analysis comprised a general descriptive evaluation of the study variables. Qualitative variables are reported as absolute and relative frequencies, while quantitative variables are reported as measures of central tendency and dispersion (mean, standard deviation [SD], median, minimum and maximum). Where inferential analyses were required, parametric tests, or nonparametric tests for variables not normally distributed, were used. Two-tailed hypothesis tests were used in all cases, with a level of significance of p<0.05. A Chi-squared test, or a Fisher exact test when applicable, was used for the analysis of contingency tables and for comparisons of proportions and/or frequency distributions.
The study was approved by the ethics committee of Burgos University Hospital (Burgos, Spain) (reference ALM-DIA-2014–01).
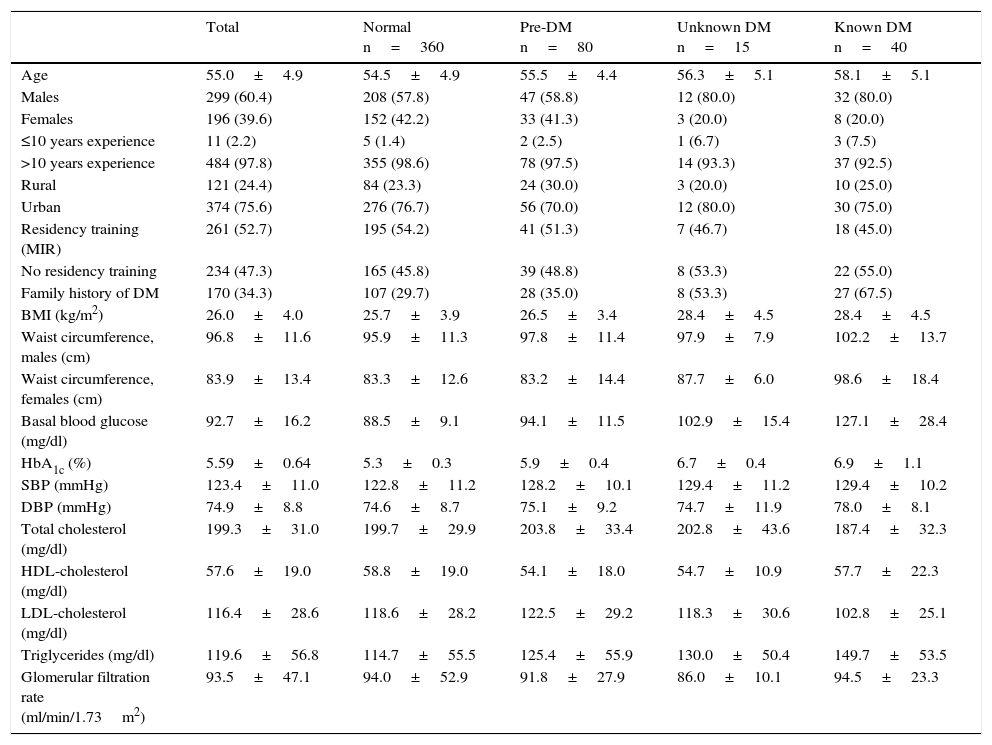
ResultsThe total study sample consisted of 495 PCPs, of whom 60.4% were males. Most of them had over 10 years of professional experience (97.8%). The majority of the physicians worked in an urban setting (75.6%), and 52.7% had received specialist training through the national medical residency program. Table 1 gives a description of the study sample globally and according to the different glucose metabolism categories (normal, prediabetes, unknown diabetes, or known diabetes).
Descriptive analysis of the study sample according to carbohydrate metabolic categories.
| Total | Normal n=360 | Pre-DM n=80 | Unknown DM n=15 | Known DM n=40 | |
|---|---|---|---|---|---|
| Age | 55.0±4.9 | 54.5±4.9 | 55.5±4.4 | 56.3±5.1 | 58.1±5.1 |
| Males | 299 (60.4) | 208 (57.8) | 47 (58.8) | 12 (80.0) | 32 (80.0) |
| Females | 196 (39.6) | 152 (42.2) | 33 (41.3) | 3 (20.0) | 8 (20.0) |
| ≤10 years experience | 11 (2.2) | 5 (1.4) | 2 (2.5) | 1 (6.7) | 3 (7.5) |
| >10 years experience | 484 (97.8) | 355 (98.6) | 78 (97.5) | 14 (93.3) | 37 (92.5) |
| Rural | 121 (24.4) | 84 (23.3) | 24 (30.0) | 3 (20.0) | 10 (25.0) |
| Urban | 374 (75.6) | 276 (76.7) | 56 (70.0) | 12 (80.0) | 30 (75.0) |
| Residency training (MIR) | 261 (52.7) | 195 (54.2) | 41 (51.3) | 7 (46.7) | 18 (45.0) |
| No residency training | 234 (47.3) | 165 (45.8) | 39 (48.8) | 8 (53.3) | 22 (55.0) |
| Family history of DM | 170 (34.3) | 107 (29.7) | 28 (35.0) | 8 (53.3) | 27 (67.5) |
| BMI (kg/m2) | 26.0±4.0 | 25.7±3.9 | 26.5±3.4 | 28.4±4.5 | 28.4±4.5 |
| Waist circumference, males (cm) | 96.8±11.6 | 95.9±11.3 | 97.8±11.4 | 97.9±7.9 | 102.2±13.7 |
| Waist circumference, females (cm) | 83.9±13.4 | 83.3±12.6 | 83.2±14.4 | 87.7±6.0 | 98.6±18.4 |
| Basal blood glucose (mg/dl) | 92.7±16.2 | 88.5±9.1 | 94.1±11.5 | 102.9±15.4 | 127.1±28.4 |
| HbA1c (%) | 5.59±0.64 | 5.3±0.3 | 5.9±0.4 | 6.7±0.4 | 6.9±1.1 |
| SBP (mmHg) | 123.4±11.0 | 122.8±11.2 | 128.2±10.1 | 129.4±11.2 | 129.4±10.2 |
| DBP (mmHg) | 74.9±8.8 | 74.6±8.7 | 75.1±9.2 | 74.7±11.9 | 78.0±8.1 |
| Total cholesterol (mg/dl) | 199.3±31.0 | 199.7±29.9 | 203.8±33.4 | 202.8±43.6 | 187.4±32.3 |
| HDL-cholesterol (mg/dl) | 57.6±19.0 | 58.8±19.0 | 54.1±18.0 | 54.7±10.9 | 57.7±22.3 |
| LDL-cholesterol (mg/dl) | 116.4±28.6 | 118.6±28.2 | 122.5±29.2 | 118.3±30.6 | 102.8±25.1 |
| Triglycerides (mg/dl) | 119.6±56.8 | 114.7±55.5 | 125.4±55.9 | 130.0±50.4 | 149.7±53.5 |
| Glomerular filtration rate (ml/min/1.73m2) | 93.5±47.1 | 94.0±52.9 | 91.8±27.9 | 86.0±10.1 | 94.5±23.3 |
Qualitative variables are given as the number of cases and as a percentage (in brackets) of the total valid cases in the column.
Numerical variables are given as the mean±standard deviation.
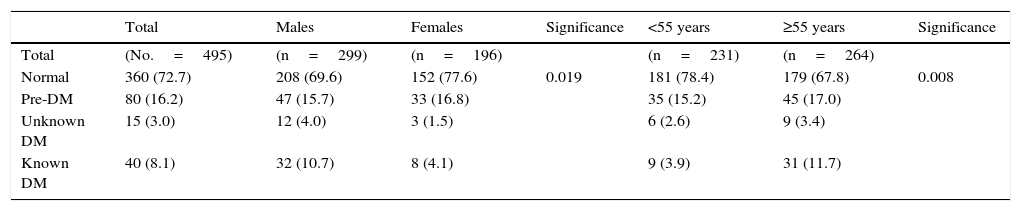
Table 2 shows the prevalence of the different glucose metabolism categories. The overall prevalence of T2DM among PCPs was 11.1% (95% CI 8.33–13.9). An interesting observation was the difference in prevalence between the sexes: 14.7% in males and 5.6% in females. The prevalence of unknown T2DM was 3.0% (95% CI 1.50–4.50). The unknown/known diabetes ratio was 0.37/1. Known diabetes was more frequent among males, and from the age of 55 years onwards (p=0.008).
Prevalence of carbohydrate metabolic disorders.
| Total | Males | Females | Significance | <55 years | ≥55 years | Significance | |
|---|---|---|---|---|---|---|---|
| Total | (No.=495) | (n=299) | (n=196) | (n=231) | (n=264) | ||
| Normal | 360 (72.7) | 208 (69.6) | 152 (77.6) | 0.019 | 181 (78.4) | 179 (67.8) | 0.008 |
| Pre-DM | 80 (16.2) | 47 (15.7) | 33 (16.8) | 35 (15.2) | 45 (17.0) | ||
| Unknown DM | 15 (3.0) | 12 (4.0) | 3 (1.5) | 6 (2.6) | 9 (3.4) | ||
| Known DM | 40 (8.1) | 32 (10.7) | 8 (4.1) | 9 (3.9) | 31 (11.7) |
Qualitative variables are given as the number of cases and as a percentage (in brackets) of the total valid cases in the column.
The overall prevalence of prediabetes was 16.2% (95% CI 13.0–19.4), with no relevant differences between males and females or by age group.
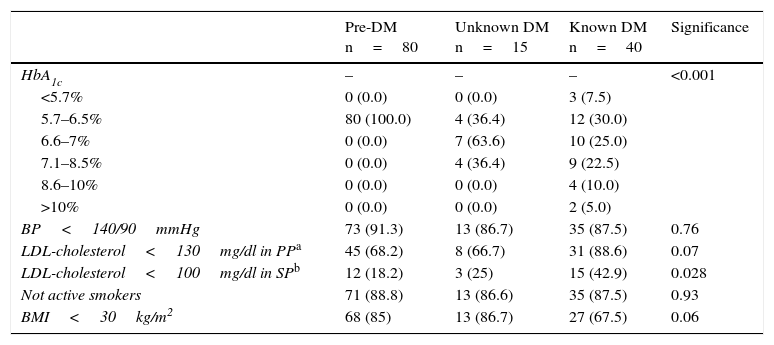
On analyzing the degree of control of the risk factors among the physicians with some glucose metabolism disorder (Table 3), 62.5% of those who were aware of the disease presented HbA1c control values of <7%, while 15.0% had concentrations above 8.5%. Blood pressure control (BP<140/90mmHg) was reached by 87.5% of the physicians with known diabetes. In the PCPs with known diabetes and no history of macrovascular disease, LDL-cholesterol control (<130mg/dl) was reached in 88.6% of the cases, while in the case of the PCPs with known diabetes and a history of macrovascular disease, LDL-cholesterol control (<100mg/dl) was only reached in 42.9% of the cases. A total of 12.5% continued to be active smokers.
Degree of control of the risk factors in the physicians with carbohydrate metabolic disorders.
| Pre-DM n=80 | Unknown DM n=15 | Known DM n=40 | Significance | |
|---|---|---|---|---|
| HbA1c | – | – | – | <0.001 |
| <5.7% | 0 (0.0) | 0 (0.0) | 3 (7.5) | |
| 5.7–6.5% | 80 (100.0) | 4 (36.4) | 12 (30.0) | |
| 6.6–7% | 0 (0.0) | 7 (63.6) | 10 (25.0) | |
| 7.1–8.5% | 0 (0.0) | 4 (36.4) | 9 (22.5) | |
| 8.6–10% | 0 (0.0) | 0 (0.0) | 4 (10.0) | |
| >10% | 0 (0.0) | 0 (0.0) | 2 (5.0) | |
| BP<140/90mmHg | 73 (91.3) | 13 (86.7) | 35 (87.5) | 0.76 |
| LDL-cholesterol<130mg/dl in PPa | 45 (68.2) | 8 (66.7) | 31 (88.6) | 0.07 |
| LDL-cholesterol<100mg/dl in SPb | 12 (18.2) | 3 (25) | 15 (42.9) | 0.028 |
| Not active smokers | 71 (88.8) | 13 (86.6) | 35 (87.5) | 0.93 |
| BMI<30kg/m2 | 68 (85) | 13 (86.7) | 27 (67.5) | 0.06 |
Qualitative variables are given as the number of cases and as a percentage (in brackets) of the total valid cases in the column.
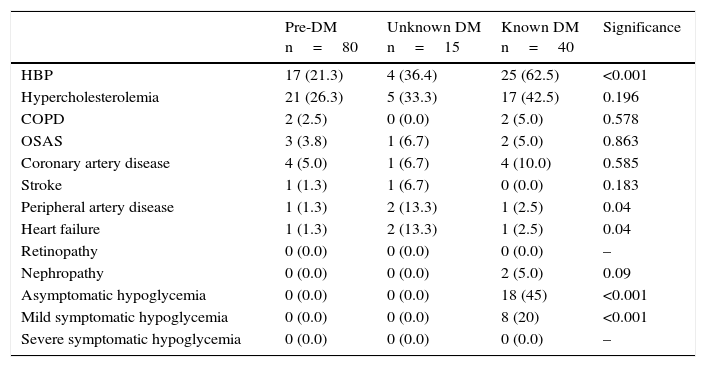
Table 4 analyzes the presence of comorbidities and chronic complications in the different scenarios referring to carbohydrate metabolism. The presence of both in the subjects with known T2DM should be noted (62.5%). Macrovascular complications (particularly peripheral artery disease) were more common in the physicians with unknown diabetes than in those with known disease (p=0.04).
Presence of comorbidities and/or complications in the physicians with carbohydrate metabolic disorders.
| Pre-DM n=80 | Unknown DM n=15 | Known DM n=40 | Significance | |
|---|---|---|---|---|
| HBP | 17 (21.3) | 4 (36.4) | 25 (62.5) | <0.001 |
| Hypercholesterolemia | 21 (26.3) | 5 (33.3) | 17 (42.5) | 0.196 |
| COPD | 2 (2.5) | 0 (0.0) | 2 (5.0) | 0.578 |
| OSAS | 3 (3.8) | 1 (6.7) | 2 (5.0) | 0.863 |
| Coronary artery disease | 4 (5.0) | 1 (6.7) | 4 (10.0) | 0.585 |
| Stroke | 1 (1.3) | 1 (6.7) | 0 (0.0) | 0.183 |
| Peripheral artery disease | 1 (1.3) | 2 (13.3) | 1 (2.5) | 0.04 |
| Heart failure | 1 (1.3) | 2 (13.3) | 1 (2.5) | 0.04 |
| Retinopathy | 0 (0.0) | 0 (0.0) | 0 (0.0) | – |
| Nephropathy | 0 (0.0) | 0 (0.0) | 2 (5.0) | 0.09 |
| Asymptomatic hypoglycemia | 0 (0.0) | 0 (0.0) | 18 (45) | <0.001 |
| Mild symptomatic hypoglycemia | 0 (0.0) | 0 (0.0) | 8 (20) | <0.001 |
| Severe symptomatic hypoglycemia | 0 (0.0) | 0 (0.0) | 0 (0.0) | – |
Qualitative variables are reported as the number of cases and as a percentage (in brackets) of the total valid cases in the column for each variable.
The same table shows that no severe hypoglycemic episodes occurred in the physicians with diabetes. Eight physicians with known diabetes (20%) had experienced mild symptomatic hypoglycemia on some occasion over the previous 6 months, and 18 (45%) had detected a drop in capillary blood glucose to under 70mg/dl, without symptoms.
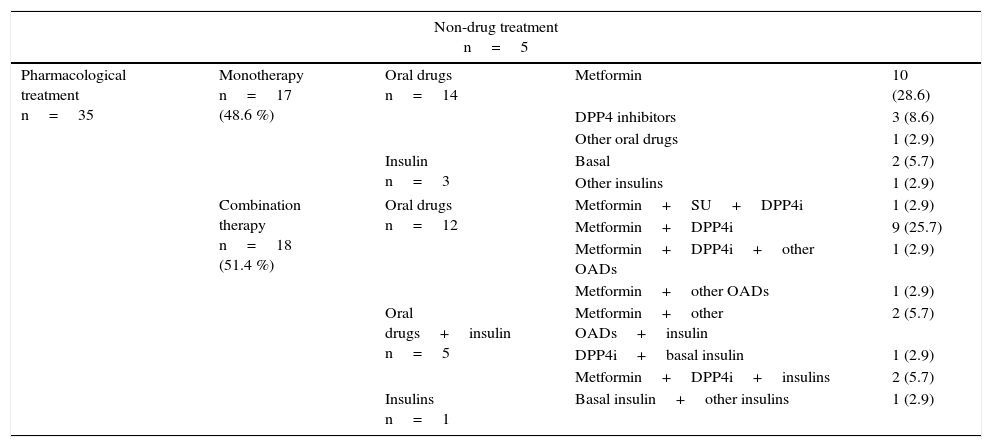
As regards their treatment of T2DM, of the 40 physicians with known diabetes (Table 5), five did not use drugs to control their blood glucose levels. Of the 35 PCPs who used drug treatment, 71.4% self-prescribed such medication. Monotherapy was used by 48.6%, while 51.4% used some form of combination treatment. Overall, among the physicians who used drug treatment to control T2DM, metformin was the most widely used option (74.3%), followed by DPP4 inhibitors (48.6%).
Treatment of hyperglycemia in the physicians with known diabetes mellitus (n=40).
| Non-drug treatment n=5 | ||||
|---|---|---|---|---|
| Pharmacological treatment n=35 | Monotherapy n=17 (48.6 %) | Oral drugs n=14 | Metformin | 10 (28.6) |
| DPP4 inhibitors | 3 (8.6) | |||
| Other oral drugs | 1 (2.9) | |||
| Insulin n=3 | Basal | 2 (5.7) | ||
| Other insulins | 1 (2.9) | |||
| Combination therapy n=18 (51.4 %) | Oral drugs n=12 | Metformin+SU+DPP4i | 1 (2.9) | |
| Metformin+DPP4i | 9 (25.7) | |||
| Metformin+DPP4i+other OADs | 1 (2.9) | |||
| Metformin+other OADs | 1 (2.9) | |||
| Oral drugs+insulin n=5 | Metformin+other OADs+insulin | 2 (5.7) | ||
| DPP4i+basal insulin | 1 (2.9) | |||
| Metformin+DPP4i+insulins | 2 (5.7) | |||
| Insulins n=1 | Basal insulin+other insulins | 1 (2.9) | ||
OADs: oral antidiabetic drugs. Percentages of total subjects on drug treatment are given in brackets.
Sulfonylureas were only used in one case (2.9% of the total drug treatments) and in the context of triple therapy (together with metformin and DPP4 inhibitors). A total of 25.7% of the diabetic physicians on drug treatment used some type of insulin.
DiscussionIt is quite common to forget that health professionals are exposed to the same risk factors and diseases as the rest of the population. As a result, few studies specifically address this patient subgroup. In the specific case of T2DM, we have found no study on the epidemiology and management characteristics of the disease among Spanish PCPs. This is probably the strong point of our study.
The PRISMA trial was a cross-sectional, descriptive study of a sample of PCPs with professional practice in Spain. As regards the limitations of the study, mention should be made of its small sample size (n=495), which resulted in the limitation of the cases of T2DM to only 40. This situation often makes it difficult to find statistically significant relationships and underscores the need in many cases to interpret the data more in terms of their clinical relevance than in terms of their statistical significance. Another potential source of bias is represented by the selection of the PCPs from the registry of the Fundación redGDPS, since registration on its website is entirely voluntary and presumably reflects a greater interest in diabetes on the part of those who register compared with other PCPs in Spain. A further potential source of bias is the methodology used to determine capillary HbA1c, despite the fact that its concordance versus other laboratory methods is excellent (R2=0.94).8
A comparison of the epidemiological data from our study with those of the di@bet.es study showed that the prevalence of unknown diabetes was lower in our study than in the general population (3.0% versus 6%). However, in contrast to our study, which was only based on the HbA1c values, the di@bet.es trial also contemplated the possibility of glucose overload testing. There were less significant differences in the overall prevalence of T2DM (11.1% versus 13.8%) and in the prevalence of prediabetes (16.2% versus 14.8%).3
With regard to the degree of blood glucose control, a comparison with the largest study conducted in Spain with information from large databases (eCONTROL)9 showed the percentage of known diabetics with HbA1c<7% to be slightly higher among the physicians of the PRISMA study (62.5% versus 56%). The degree of control of BP (87.5% versus 69%) and the lipid profile in both primary (88.6% versus 72.5%) and secondary prevention (42.9% versus 38%), was also higher among the physicians of the PRISMA trial.10
As regards treatment, it should be noted that 71.4% of diabetic physicians self-treated their disease, and most used combinations of two or more drugs (51.4%). Metformin was the most widely used drug (74.3%), followed by DPP4 inhibitors (48.6%). Only 2.9% of the diabetic physicians used sulfonylureas, which is not consistent with the recommendations of many of the clinical practice guidelines endorsed by the medical profession11,12 or the data of the population-based eCONTROL study (sulfonylureas were the second most frequently used drugs in the global diabetic population of Catalonia in 2009).13 Interpreting this discrepancy between physician self-prescription and the therapeutic recommendations to patients would require a specific analysis that falls outside the scope of our study.
Different studies have shown the influence of the attitudes and perception of healthcare professionals upon their patients. In Spain, mention in this regard should be made of the CHABS14 and ICARIA studies.15,16 The CHABS study specifically assessed the self-perceived health of 2583 PCPs and found a self-reported prevalence of diabetes mellitus of 2.9%, while 8.5% reported obesity. In contrast, the ICARIA study, conducted on 782,519 workers, of whom 1340 were physicians (their specialties were not stated), found worrisome figures in terms of obesity and overweight among the medical population (37.7% of the cases).
The physician–patient relationship is known to influence the control of chronic diseases such as DM2 (as was clearly seen in studies such as MOSAIc,17 HRS18,19 and others20,21). However, we have found no studies in diabetic physicians allowing an analysis of the relationship between their disease perception and control and their therapeutic approach to patients or patient adherence to therapy. We think that this study may serve as a starting point for analyzing this dichotomic diabetic physician–diabetic patient relationship from a different perspective.
FundingFunding without restrictions from Laboratorios Almirall.
Conflicts of interestThe authors state that they have no conflicts of interest in relation to this article.
This study has been possible thanks to unrestricted funding from Laboratorios Almirall.
Please cite this article as: Franch-Nadal J, Mediavilla-Bravo J, Mata-Cases M, Mauricio D, Asensio D, Sarroca J. Prevalencia y control de la diabetes mellitus tipo 2 entre los médicos de Atención Primaria de España. Estudio PRISMA. Endocrinol Diabetes Nutr. 2017;64:265–271.