Advances in our understanding of human biology have revealed the complexity of the pathogenesis of chronic diseases; however, we know that health does not depend solely on scientific and technological advances, but that the important role of healthy lifestyles at individual and community levels is becoming increasingly clear. Lifestyle change, particularly diet, is the cornerstone of the population strategy for cardiovascular prevention and the basis for individual intervention to reduce the potency of risk factors. To achieve favourable changes in dietary habits, it is important to provide both the target population and health professionals with clear, realistic, and feasible advice based on the latest scientific evidence, so that individuals are equipped with essential tools to improve their health. Our aim is to update the knowledge on the relationship between diet and cardiovascular risk (CVR) and to provide health professionals with a simple guide to translate the dietary recommendations on the major food groups and dietary patterns into clinical practice, defining lines of action to be communicated to people receiving advice on cardiovascular prevention to enable them to choose a healthy dietary pattern.
In 2018, the Spanish Society of Arteriosclerosis (SEA) published a document of recommendations on lifestyle in cardiovascular prevention,1 whose chapters on diet are updated here, considering that dietary advice should be the same for the control of CVR factors and for the prevention of atherosclerotic vascular disease, as reflected in the recent SEA document of standards for global control of vascular risk2 and in the 2021 American Heart Association (AHA) guidance.3 One aspect that has been considered in previous documents1,4 is the modification of the traditional concept of the basic nutritional unit of the diet, i.e., nutrients, to that of foods, which are complex matrices in which the different components that make them up exert synergistic or antagonistic effects on different metabolic pathways and are responsible for the overall effect of the intake of a given food on cardiovascular health. The various mixtures of different foods and their culinary forms make up a specific dietary pattern, which is considered the most appropriate way to assess the relationship between diet and health or disease.
Knowledge about the relationship between diet and CVR is far from reaching the level of evidence achieved in clinical drug trials. In general, randomised clinical trials (RCTs) of dietary interventions with clinical event outcomes are scarce, although of great importance, such as the PREDIMED study,5 a landmark clinical trial of primary prevention of cardiovascular disease, and recently the CORDIOPREV study of secondary prevention6; both RCTs have provided high-level evidence of the cardiovascular health benefits of a Mediterranean diet enriched with paradigmatic foods of this dietary pattern, such as extra virgin olive oil (EVOO) or nuts. However, for most foods and dietary patterns there are no RCTs available with clinical event outcomes, and therefore we have to rely on data from observational epidemiological studies, especially large follow-up cohort studies, and systematic reviews and meta-analyses that synthesise the results of the different studies. However, research into the benefits of diet in cardiovascular prevention has many weaknesses, especially when compared with drug trials. There are no reliable methods to know exactly what a person eats from day to day over the years, because of the difficulty of collecting data and their subjectivity; the differences in the composition of foods at different times; the fact that human behaviour often changes over time; the lack of tools to ensure adherence, except when objective circulating or urinary biomarkers are available, which is not the case for most foods; and so on. However, for the study of the relationship between lifestyle and CVR we have very valuable information that is lacking in pharmacological trials. This is the knowledge provided by historical tradition, which allows us to understand the long-term health effects of lifestyle in different populations. In addition, the number of RCTs investigating the relationship between diet and surrogate markers of CVR has increased exponentially. Some of these are clinical, such as body weight or blood pressure (BP), and others are biochemical, such as lipid profile, glycaemic control, pro-inflammatory status, or oxidative stress, which are very useful markers of CVR and general health status. A recent meta-epidemiological study compared data from prospective cohort studies and RCTs with similar nutritional exposures (of dietary patterns or nutrient intakes) and clinical outcomes (of disease or risk factors), matching meta-analyses with the highest level of evidence from both types of studies, and concluded that the difference between prospective studies and RCTs in pooled results was small.7 This agreement between the levels of evidence from the 2 main methods that nutrition science uses to assess the relationship between diet and health is of great interest and practical application; for example, if an RCT shows that a particular food reduces cholesterolaemia or BP, we can be confident that its long-term consumption will reduce the incidence of cardiovascular disease (CVD).
In recent years, several consensus documents and recommendations from scientific societies have analysed the complex relationship between diet and CVR in general3 and with cardiometabolic diseases such as dyslipidaemia,8 type 2 diabetes mellitus (T2DM9,10 and hypertension (HTN).11 This SEA paper discusses novel aspects of the complex relationship between diet and CVD, some of which modify traditional recommendations for cardiovascular prevention. A good example is that most cohort studies do not show a significant relationship between dietary cholesterol and CVR, so rather than limiting cholesterol intake to a certain level,8 it is advisable to include foods rich in cholesterol, but also in other bioactive nutrients, such as eggs, in a healthy dietary pattern. For example, among healthy adults, especially those who consume more fish and dietary fibre, higher intakes of eggs may contribute to an improved lipid profile.12 A number of recent meta-analyses confirm that whole grain consumption is associated with a lower risk of T2DM, coronary heart disease (CHD), cerebral vascular accident (CVA), and all-cause mortality13; a controversial finding of this series of systematic reviews is that, when comparing high and low glycaemic index and glycaemic load diets in prospective studies or RCTs, no changes in the power of cardiometabolic risk factors or clinical cardiovascular events are apparent. However, another recent meta-analysis of data from 10 large cohorts contradicts these results by showing a significant increase in the incidence of T2DM, CVD, several types of cancer and all-cause mortality with higher glycaemic index diets, contrary to that observed with higher consumption of wholegrain cereals and fibre, also analysed in this meta-analysis.14 In any case, in the context of a varied and healthy diet such as the Mediterranean diet, there is no reason to discourage the consumption of basic foods such as bread made with refined flour, white rice, or potatoes, which should never be eaten alone when their glycaemic index would be high, but always with food (bread), or with sofrito, other sauces, or vegetables (white rice and potatoes).
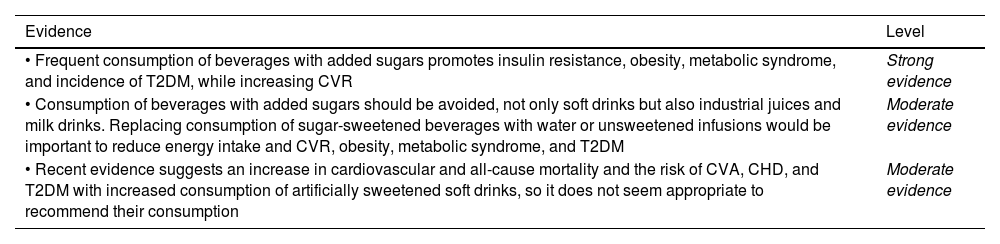
Other aspects that have been evaluated include the inverse association between coffee consumption and the risk of T2DM and the increased risk associated with the consumption of artificially sweetened beverages.15 The beneficial effects of (unsweetened) coffee on BP and CVR have led to its daily consumption being recommended as part of the lifestyle for the treatment of HTN.12 Currently, many consumers who are addicted to sugary drinks, but concerned about the excess energy provided by the added sugar, substitute them with similar drinks sweetened with low-calorie sweeteners, believing them to be safe. However, evidence on the relationship between the consumption of artificially sweetened beverages and CVR suggests an increased incidence of CVD and T2DM16 and an increase in cardiovascular and all-cause mortality17 that is also observed in patients with T2DM18 and makes this type of beverage inadvisable.
Recently, epidemiological studies on the health effects of the consumption of so-called "ultra-processed" foods according to the NOVA classification have increased significantly, as has controversy about their possible adverse effects.19 Although recent evidence confirms the association of their higher overall consumption with the risk of all-cause and CVD mortality,20 not all of these foods are harmful,21 as there are foods classified as ultra-processed (wholegrain breakfast cereals, fruit yogurts, and other dairy desserts) whose consumption is associated with protection against the risk of T2DM.22 In this sense, fruit juices (without added sugar) were considered harmful due to their high content of simple sugars and lower fibre content than natural fruit, and almost equated with industrial sugary drinks; however, recent data from nutritional studies with more precise exposure (e.g., 100% fruit juice with no added sugar) indicate that their consumption is healthy and can help to meet the population recommendation of 5 servings of fruit and vegetables per day for better cardiovascular and general health, especially in children and the elderly.23
A current but evolving issue is that of personalised diets and precision diets, which are often used interchangeably. It is well known that the response of risk factors (such as cholesterol) or vascular risk per se (such as a cardiovascular event) to dietary changes can vary widely between individuals. This is largely due to interactions with each person's genotype, but also with their phenotype, metabolic and lifestyle variables, behaviour, socio-economic status, and environmental exposures.24 It is clear that personalised dietary advice (tailored to each individual) will be more effective in reducing the potency of risk factors and the risk of disease than generic dietary advice. This is early science, but precision nutrition could be of great importance in the future to improve CVR in large segments of the population. Although we may not realise it, we are already using it for relatively common genetic diseases: dairy-free diets for lactose intolerance, gluten-free diets for coeliacs, etc.25 Therefore, there are already personalised diets that are easy to recommend for very specific cases.
A challenge that has emerged in recent years is to change the food model, advocating that dietary habits should be healthy for the population, but also sustainable for the planet, the paradigm being a plant-based diet, rich in fruits, vegetables, legumes, whole grains, and nuts and, above all, reducing meat consumption, while choosing local and seasonal foods as the basis of the diet, as in the Mediterranean diet.26,27 In terms of consumer information, the Nutri-Score nutritional information system has been implemented in several European countries, including Spain, based on front-of-package labelling of foods with 5 letters and colours according to decreasing quality from ‘A’ green to ‘E’ red.28 The algorithm used to classify foods takes into account their content per 100 g of harmful elements or nutrients (total energy, simple sugars, saturated fatty acids [SFAs] and salt) and of healthy components (protein, fibre, and proportion of vegetables and fruits), but not the degree of processing. However, the Nutri-Score complements the NOVA classification of processed foods. The Nutri-Score algorithm, created in 2017, was updated in 2023 to allow better discrimination between different products and to align with the dietary guidelines for the population of the countries involved.29 The Nutri-Score front-of-pack label on foods highlights their nutritional quality, helping the nutritionally illiterate consumer to choose the healthiest foods at point of purchase. Results from a recent Spanish epidemiological study show that Nutri-Score classification of the usual diet of a large cohort is strongly associated with all-cause, cardiovascular, and cancer mortality, supporting its use in public health nutrition.30 However, the Nutri-Score has been rejected by some Spanish nutritionists because it does not give the best grade to EVOO, which was given an embarrassing 'C' in the first algorithm, although it has been up-graded in the latest re-evaluation to a 'B'.
In our cultural context, the traditional Mediterranean diet, with the use of EVOO as a cooking oil, a preference for natural foods of plant origin, fish, and seafood, together with a reduction in red and processed meats, and the avoidance of ultra-processed foods, is both the healthiest and most sustainable dietary pattern.31
In this paper we have undertaken an updated review that aims to provide useful, graded evidence on diet and cardiovascular and general health, although it must be recognised that it is difficult to base recommendations on commonly used categories of clinical evidence. Nevertheless, we have synthesised the available evidence on the relationship between food and dietary patterns and CVR (Fig. 1) and developed recommendations using RCTs, where available, observational studies of clinical evidence or surrogate markers and their meta-analyses, and expert consensus. In summary, 3 types of recommendations are made, included in each chapter: strong evidence, based on RCTs, meta-analyses of large observational studies and systematic reviews (umbrella meta-analyses) incorporating quality criteria; moderate evidence, based on prospective cohort studies and their meta-analyses, but with evidence of heterogeneity, and case-control studies; and weak evidence based on expert consensus and opinion and small or highly heterogeneous cohort studies. In conclusion, this updated guideline on diet and cardiovascular prevention is aimed at both the target population and health professionals to help them make informed decisions about the best dietary choices to reduce CVR, considering the recommendations useful in both primary and secondary prevention of CVD.
(A) Associations between consumption of different foods and cardiovascular risk. The intensity of the colour reflects the level of evidence, from high to low for reduced risk (green panels) and from low to high for increased risk (red panels). (B) Association between dietary patterns and cardiovascular risk: Mediterranean diet: strong evidence; DASH diet: moderate evidence; vegetarian diet: moderate evidence; Nordic diet: moderate evidence; MIND diet: weak evidence.
Oils contain 100% fat in the form of triglycerides, although the fatty acid composition varies greatly between oil types. Derived from oilseeds, such as maize, sunflower, rapeseed, and soya, or fruits such as coconut, palm, and olive, they are used daily as edible fats by large segments of the world's population, and are an important source of energy for their consumers. Some oils, such as the so-called tropical oils due to their origin (coconut and palm), are very rich in SFAs; others, such as canola (a derivative of rapeseed), olive, and sunflower oils of the high oleic type, are rich in monounsaturated fatty acids (MUFAs); maize, sunflower, and soybean oils are rich in n-6 polyunsaturated fatty acids (PUFAs), particularly linoleic acid (C18:2 n-6), while canola and soybean oils contain about 7% n-3 PUFAs (C18:3 n-3, α-linolenic acid, vegetable omega-3).32 (Table 1) Oils obtained from the milling of most seeds and fruits are not suitable for consumption; to be edible and acceptable to the consumer, they must be refined by physical or chemical processes, including extraction, bleaching, and deodorisation, which retain the lipophilic molecules associated with the fat fraction, such as vitamin E and phytosterols, but lose important hydrophilic components, such as polyphenols. EVOO, which is obtained by simple cold pressing and is therefore pure olive juice, is a notable exception among the cooking oils, as it contains highly bioactive phenolic compounds, especially secoiridoids (oleocanthal, oleuropein, oleacein) and phenolic alcohols (hydroxytyrosol).34 The polyphenol content is therefore much higher in virgin olive oil than in refined olive oil; the European Food Safety Agency (EFSA) has authorised a health claim on the cardiovascular benefits of olive oil containing more than 250 mg/kg of polyphenols (the claim relates to the protection of LDLs from oxidation); this content depends on the variety of olives used to make the oil and their degree of ripeness.35
Average fatty acid content of commonly used edible oils (grams per 100 g).
| Fatty acids | Canola | Coconut | Sunflower | Maize | Olive | Palm | Soybean |
|---|---|---|---|---|---|---|---|
| Saturated | 6.6 | 82.5a | 9.9 | 13.4 | 15.4 | 49.3b | 14.9 |
| Monounsaturated | 62.6 | 6.3 | 29.9 | 27.7 | 69.2 | 37 | 22.1 |
| Polyunsaturated | 25.3 | 1.7 | 59.2 | 52.9 | 9.1 | 9.3 | 57.6 |
| Linoleic | 17.8 | 1.7 | 59.0 | 51.9 | 8.4 | 9.1 | 50.9 |
| α-linolenic | 7.5 | 0 | .2 | 1.0 | .7 | .2 | 6.6 |
Dietary SFAs are known to increase total cholesterol and low-density lipoprotein cholesterol (LDL-C), with an associated increase in CVR, whereas MUFAs and especially PUFAs have the opposite effect.36 Therefore, frequent consumption of SFA-rich oils, such as coconut and palm oil, or PUFA-rich oils, such as corn and soybean oil, may be associated with detrimental or beneficial effects on CVR, respectively. However, with the exception of the paradigmatic case of EVOO, there is no epidemiological or clinical trial evidence on the effects of consumption of different oils on the incidence of CVD. However, there are data from clinical trials on intermediate markers such as circulating lipids, with predictable results when unsaturated oils are replaced by coconut and palm oils: a modest increase in LDL-C, but also in high-density lipoprotein cholesterol (HDL-C).37
Olive oil, the characteristic cooking fat of the Mediterranean diet, is distinguished from other oils not only because of the availability of an affordable virgin variety, but also because its cardioprotective properties and other health effects have been evaluated in numerous cohort and clinical studies, targeting both intermediate markers and CVD. The fat fraction consists mainly of the MUFA oleic acid (C18:1 n-9), with small amounts of tocopherols (vitamin E) and phytosterols, while the aqueous fraction, which is lost during refining, contains the phenolic compounds to which much of the cardioprotective effects of virgin olive oil are attributed.34 When exchanged for SFAs or carbohydrates, MUFAs reduce LDL-C and increase HDL-C.36 A recent meta-analysis of 27 RCTs comparing the lipid effects of olive oil with those of other vegetable oils suggests that olive oil reduces total cholesterol, LDL-C, and triglycerides less than other plant oils, but increases HDL-C more.38 There is also evidence of beneficial effects of olive oil and its polyphenols on endothelial function, inflammation, and LDL oxidation.39
The results of a recent meta-analysis of 24 prospective studies evaluating olive oil exposure in relation to the incidence of various diseases suggest a beneficial association between olive oil consumption (olive oil of unspecified type in general), with a risk ratio (RR) of .84, 95% CI: .76–.94 per additional 25 g/day, for CVD; of .78, 95% CI: .69–.87, also per 25 g/day, for T2DM; and of .89, 95% CI: .85–.93 per 25 g/day, for all-cause mortality, but with no association with cancer risk.40 A recent prospective study in a large Spanish cohort found that virgin olive oil, but not regular olive oil, was associated with a lower risk of all-cause and CVD mortality.41
As EVOO was one of the main foods supplemented in one of the arms of the PREDIMED RCT, which evaluated the effects of the Mediterranean diet on primary prevention of CVD in high-risk individuals, there is first-rate scientific evidence on the health effects of this oil. After approximately 5 years of dietary intervention, the main results showed that participants assigned to the Mediterranean diet supplemented with EVOO experienced an average 31% reduction in the incidence of CVD.5 Another landmark Spanish RCT evaluating the effects of a Mediterranean diet supplemented with EVOO compared to a low-fat diet was the CORDIOPREV trial in patients with established ischaemic heart disease, which showed a 25%–29% reduction in CVD after 7 years of follow-up.6 There is therefore strong evidence for the cardioprotective effect of EVOO as part of the Mediterranean diet.
MargarinesThese foods are structured water-in-oil emulsions that are stable, spreadable, and have a pleasant mouth feel. They are made by converting a liquid food such as oil into a semi-solid that is easy to spread. In the past, this was achieved by partial hydrogenation of unsaturated oils (converting the double bonds of fatty acids into single bonds, i.e., creating SFAs), which also created trans fatty acids (TFAs). The scientific evidence that emerged in the 1990s on the adverse effects of TFAs on lipids and CVR led to a significant shift in margarine production using healthier bases (unsaturated vegetable oils such as soya, sunflower, or canola) in combination with technologies that make it possible to produce products low in SFAs and virtually free of TFAs (transesterification instead of hydrogenation), as well as higher levels of n-6 (linoleic acid) and n-3 (α-linolenic acid) essential fatty acids. The nutritional composition of modern margarines varies in terms of fat and water content, ranging from 20% to 80%, depending on whether they are low or high in fat and energy. They contain up to 50% of fatty acids in the form of PUFAs, of which 10%–20% are n-3, with only 20%–25% SFAs and <1% TFAs. The current production process of margarines allows them to retain the vitamin E bound to the fat fraction of the original oil, and they are also often fortified with vitamins A and D.42 As they are made from seed oils, margarines and other commonly used spreads such as mayonnaise can be an important source of n-6 (linoleic) and n-3 (α-linolenic) PUFAs, especially in Spain where consumption of these essential fatty acids is rather low.32
Levels of evidence for dietary fats and cardiovascular risk
| Evidence | Level |
|---|---|
| • In epidemiological studies, olive oil consumption in general is associated with a reduction in the incidence of CVD, T2DM, and all-cause mortality | Moderate evidence |
| • In clinical trials and in the context of the Mediterranean diet, extra virgin olive oil has been shown to be effective in the prevention of CVD | Strong evidence |
Based on the composition and cardiometabolic effects of commonly used vegetable oils, there is little doubt that virgin olive oil is the healthiest and is recommended for daily use in cooking and at the table. If you want to use PUFA-rich oils such as maize, soybean, and sunflower oils, use them raw for dressing and not for cooking or frying, as heat stress causes auto-oxidation of PUFAs mediated by oxygen-free radicals, producing aldehydes, TFAs, and other pro-inflammatory and atherogenic molecules.43,44 In contrast, olive oil withstands frying temperatures well because of its low PUFA content. However, it should not be fried at temperatures that cause the oil to smoke (burn) and degrade: 160 °C for EVOO, 215 °C for virgin olive oil, and 240 °C for refined oil. EVOO loses polyphenols during frying, but remains rich in these powerful antioxidants.45 Due to their high PUFA content, margarines should not be used for cooking or frying, but only as a spread.
Vegetables, fruits, and tubersVegetables (including vegetables), fruits and tubers are a wide range of plant foods characterised by a high water content (around 80% of their weight), a low calorie content and a very similar nutrient composition, with some differences such as a higher carbohydrate content in fruits and tubers. Another important characteristic is the contribution of micronutrients such as vitamins A, B, C, and E, folic acid, minerals, phenolic compounds and, last but not least, a high fibre content. On the one hand, the contribution of vitamins and minerals other than sodium gives them beneficial properties in age-related diseases such as CVD. On the other hand, the complex carbohydrates and fibre contained in these foods have significant cardiometabolic benefits.
When consuming these foods, it is important to take into account the way they are prepared, since in many cases their inclusion in stews, boiled, or fried foods alters both their organoleptic properties and their composition, since cooking causes the loss of water-soluble vitamins, such as those in the B and C groups, minerals, and even phenolic compounds, which dissolve in the cooking liquid or can be destroyed by heat, especially during frying. For this reason, it is important to eat them raw, in salads, gazpacho, or salmorejo, and to follow some recommendations when preparing them, such as not peeling them, cutting them into large portions, avoiding long soaking or boiling times, preferably steaming them, etc., or avoiding frying them for a long time at high temperatures or reheating them repeatedly.
Fruit and vegetablesThere is a large body of scientific evidence linking vegetable consumption with health benefits in terms of cardiometabolic effects, CVD, and all-cause mortality. A recent meta-analysis of 81 prospective cohorts with more than 4 million participants and an average follow-up of 11 years concluded that the highest compared with the lowest category of vegetable consumption was associated with a significant reduction in total CVD, CHD, and CVA risk, with reductions of 9%, 12%, and 18%, respectively.46 In this systematic review, consumption of garlic, carrots, cruciferous vegetables, and green leafy vegetables was associated with greater CV benefits. A recent meta-regression analysis of cohort studies concluded that increasing vegetable intake from zero to a theoretical minimum of 306 g–372 g/day was associated with a 23% reduction in the risk of CHD and CVD and a 26% reduction in the risk of T2DM.47
The nutritional function of fruits is very similar to that of vegetables, although they are more energy-dense due to their high carbohydrate content, mainly in the form of simple sugars such as sucrose and fructose. Like vegetables, fruit has a high fibre content, although this is reduced when the fruit is peeled and especially when it is consumed as juice. The nutrients in fruit have beneficial effects on cardiometabolic risk factors, including effects on blood pressure and the risk of developing HTN, with consumption of 200 g/day of fruit significantly reducing the risk of HTN by up to 8%, suggesting a likely dose-response effect; in contrast, no association was found for vegetables.48 It is clear that fruit consumption has a positive effect on health. A meta-analysis of observational studies showed that an increase in fruit consumption of 100 g per day was linearly associated with an 8%–13% reduction in the risk of CVD; for all-cause mortality, a significant reduction was found for fruit consumption of up to 200 g per day, with no greater benefit at higher intakes.49
Because of their similar compositional characteristics and health effects, many prospective studies and systematic reviews have examined the effects of combined fruit and vegetable consumption on health variables. In a recent meta-analysis of 22 prospective studies, compared with low fruit and vegetable consumption, high consumption was associated with a 28% (95% CI 15–39) reduction in the risk of CVD death.50 Another meta-analysis concluded that, compared with consumption of 2 servings of fruit and vegetables per day, consumption of 5 servings per day was associated with a 12% lower risk of CVD death and a 13% lower risk of all-cause mortality.51 A daily intake of 3 servings of vegetables and 2 servings of fruit was associated with the lowest mortality, and there was no further reduction in risk above these doses. As in other studies, higher fruit and vegetable consumption was also associated with beneficial effects on cancer and non-cancer mortality. The PURE study, which examined lifestyle and morbidity and mortality from various diseases in 80 countries on 5 continents, confirms that a diet high in fruit and vegetables is an important factor in reducing CVD and all-cause mortality.52 However, an umbrella review of 11 and 13 meta-analyses of fruit and vegetable consumption, respectively, concluded with moderate evidence that higher consumption of these foods has no effect on the incidence of T2DM.15 In any case, there is ample evidence that fruit and vegetable consumption is an important part of a heart-healthy diet.
Fruit and vegetable juicesIn Spanish, "zumo" (juice) is the liquid obtained directly from fruit or vegetables after they have been crushed, squeezed, or shredded; "zumo" usually retains the flesh, which contains the fibre, giving it a thick texture and an intense flavour. "Jugo" (juice), on the other hand, is the product of filtering the "zumo" to remove skin, seeds, and pulp; "jugo" contains little fibre, and therefore is more liquid than "zumo" and may contain more sugar. Unfortunately, this distinction does not exist in English, where the single word "juice" covers both concepts. This may partly explain the controversy and discrepancies in the medical literature, mostly in English, about the alleged beneficial or harmful effects of juices. Another reason for the mixed results of prospective studies in this area is that, unless 100% fruit juice is specified, the dietary exposure may be a mixture of pure juice and added sugars. Traditionally, whole fruit has been considered healthier to consume than juice; however, juice retains all the nutrients and bioactive compounds (mainly carotenoids, vitamin C, and polyphenols) present in fruit, although it provides less fibre and is a beverage rich in sugars (those inherent in the fruit) that provides similar calories to commercial sugar-sweetened beverages, and therefore some authors have equated it with them in terms of health detriment.53
Although the evidence on the health and non-health effects of fruit juices is more limited than for sugar-sweetened beverages, several large cohort studies and meta-analyses have provided data with mixed results. For example, there are data suggesting that high fruit juice consumption is associated with higher all-cause mortality,53,54 and that its effect on mortality,51,55,56 or CVD risk56,57 is neutral, and even that it is associated with a reduced risk of total CV events,58 CHD,55 and CVA,46,58 albeit with a generally low level of evidence. In addition to prospective studies, the systematic review by D'Elia et al.58 also analysed 35 RCTs comparing the effects of pure fruit juices with a control drink on cardiometabolic risk factors; the results show that fruit juices reduce systolic and diastolic blood pressure and improve endothelial function, without changing body weight, lipid profile, or glucose metabolism. Based on a review of 10 cohort studies, this meta-analysis also suggests that fruit juice consumption is not associated with the risk of T2DM.58 Considering all the available data, as in the recent comprehensive review by Rossi et al.,59 the consumption of pure vegetable and fruit juices has no adverse effects and may have beneficial effects on cardiometabolic risk, depending on the type of juice (citrus and other fruit juices, tomato, carrot, or beetroot juices, etc.). These 2 reviews58,59 emphasise that consumption of pure juices is not associated with obesity.
Given that the population (in Spain and worldwide) is far from meeting the recommendation of 5 servings of fruit and vegetables a day, a clear conclusion from the scientific evidence on the health effects of juices is that consuming one or two small glasses of fruit or vegetable juice (150–200 ml) can help meet the recommendation of 5 servings a day.23 This would be particularly useful and practical for children and the elderly. In conclusion, there is currently no justification for discouraging moderate consumption of unsweetened fruit juices as part of a balanced diet, nor for classifying these drinks as sweetened carbonated drinks.
TubersTubers (potatoes, sweet potatoes, yucca, turnips, beetroot, etc.) are thickenings of the roots of certain plants, in whose cells reserve substances of nutritional value accumulate. Tubers contain a high percentage of water, up to 75%, but also 18% of complex carbohydrates, 2%–3% of proteins, 2% of fibre, mainly soluble, and micronutrients such as potassium, calcium, magnesium, and zinc, as well as mainly B vitamins. They are also rich in vitamin C, although this is easily lost through oxidation during processing or prolonged storage. The most recommended preparation methods are steaming, baking, or boiling, although it is advisable to cook them with the skin on in order to preserve as much of their nutritional properties as possible. The most important tuber in our diet is the potato, which provides 86 kcal/100 g. At the cardiometabolic level, its consumption has been associated with an increased risk of HTN and T2DM, mainly due to the consumption of other unhealthy foods, such as those rich in saturated fats, or to preparation methods, such as commercial frying (with oils of problematic composition or that have been frequently reheated). In this regard, a meta-analysis of cohort studies shows an increase in the risk of developing T2DM of up to 10% associated with the consumption of potatoes (especially French fries).60 In fact, most studies show a neutral effect of potato consumption on cardiometabolic and other diseases; for example, a recent meta-analysis of 20 cohort studies showed no significant association between potato consumption and the risk of cardiovascular, cancer, and all-cause mortality, as long as they were boiled or baked.61 Another meta-analysis of 19 prospective studies focusing on the risk of T2DM and gestational diabetes concluded that only potato consumption above 100 g per day increased the risk, while lower intakes had a neutral or even risk reducing effect.62
Potatoes are a staple food in many cultures, widely available, inexpensive, versatile, and sustainable, but they have had an undeserved reputation as an unhealthy food, largely because they are an integral part of the unhealthy "Western diet", where they are often consumed fried,63 and because they have a high glycaemic index, a controversial index of carbohydrate quality for which recent meta-analyses have produced mixed results regarding their effect on the risk of all-cause mortality and the incidence of CHD or T2DM.13,14 In any case, given their healthy nutritional composition and the fact that in our diet they are usually eaten with sauces and combined with vegetables, potatoes are not a food to be avoided, but a healthy option in any varied and balanced diet, such as the Mediterranean diet.
Levels of evidence on vegetables, fruit, and tubers, and cardiovascular risk
| Evidence | Level |
|---|---|
| • Consumption of 5 daily servings of fruit and vegetables reduces total, CVD and cancer mortality and CVD incidence | Strong evidence |
| • The beneficial effects of fruit and vegetables are dose-dependent up to 3 daily servings of fruit and 2 daily servings of vegetables, and do not increase beyond these amounts | Strong evidence |
| • To meet the 5 daily servings of fruit and vegetables, one or more servings may be unsweetened juices, which have similar nutritional properties and cardiometabolic health effects to the original products | Moderate evidence |
| • Consumption of up to 100 g per day of boiled or baked potatoes, preferably with vegetables, does not increase the risk of CVD or T2DM | Moderate evidence |
Evidence suggests that the daily consumption of fruit and vegetables is crucial due to their beneficial effects on health, as they reduce the risk of all-cause mortality and the incidence of CVD and certain neoplastic processes. These foods are one of the pillars of the Mediterranean diet, the healthiest and most deeply rooted in our culinary tradition. There is a dose-response effect, so that the health benefits are maximised with a daily consumption of 3 servings of vegetables and 2 servings of fruit. A daily plate of raw vegetables (salad) and 2 plates of vegetables, boiled, roasted, or fried in extra virgin olive oil, with a low salt content are recommended, which can be accompanied by potatoes or other tubers up to a maximum of 100 g per day. For children and the elderly, 1 or 2 portions of conventional vegetables or fruit can be replaced by juices, preferably freshly made at home, but which can also be industrially produced, always without added sugar.
Legumes and cerealsLegumesLegumes are seeds with a high energy density and excellent nutritional value, consumed by humankind for thousands of years and an integral part of any plant-based diet, such as the Mediterranean diet. They have complex matrices, very rich in nutrients and phytochemicals, designed to support the growth of the future plant and protect its DNA, thus facilitating the perpetuation of the species. The most consumed legumes in the Spanish diet are lentils, beans, chickpeas, and peas, with a lower consumption of broad beans and soya, an oilseed legume. Their composition is dominated by complex carbohydrates (starch: 20%–27%), with a high fibre content and a low glycaemic index, and they are a good source of vegetable protein (5%–9%), although this has a lower biological value than that of animal origin, lacking some essential amino acids such as methionine. The fat content of conventional (non-oilseed) legumes is low (.5%–2.5%) and, of the micronutrients, they are rich in B vitamins, folic acid, calcium, potassium, and non-haem iron; they also contain bioactive phytochemicals such as saponins and phytosterols, which reduce the intestinal absorption of cholesterol, and powerful polyphenol-type antioxidants.64
According to a recent meta-analysis of 25 prospective studies comparing extremes of legume intake, higher intakes were associated with moderate reductions in the risk of CVD (RR: .94; 95% CI: .89–.99) and CHD (RR: .90; 95% CI: .85–.96), with no significant results for CVA.65 In this review, it was possible to perform a dose-response analysis for the risk of CHD, finding a non-linear protective association up to an intake of 400 g/week, which was associated with a risk reduction of about 20%. There is also evidence from a meta-analysis of 32 cohorts that a higher legume intake is associated with a 6% reduction in the risk of all-cause mortality and a 9% reduction in stroke death, with no association observed on CVD, CHD, or cancer mortality.66 In a linear dose-response analysis, each 50 g increase in legume intake was associated with a 6% reduction in all-cause mortality. Another recent meta-analysis of 31 cohort studies found no association between legume intake and the incidence of CVD or T2DM.67 On the other hand, 2 prospective Spanish studies based on the PREDIMED cohort found conflicting results for the higher legume intake groups: increased all-cause and CVD mortality, but decreased cancer deaths and reduced incidence of T2DM.69 The discordance between the results of the meta-analyses65,67 and those of the PREDIMED substudies68,69 highlights the need for further studies to better elucidate the effect of legume consumption on cardiovascular health and T2DM.
The apparent cardiovascular benefit of legumes suggested by most epidemiological studies would be supported by evidence from RCTs of their effects on cardiometabolic risk factors. The systematic review by Thorisdottir et al.67 also analysed 15 RCTs of legume diets versus control diets that assessed effects on risk factors and concluded that legumes modestly reduced LDL-C, blood glucose, and HOMA-IR and had no effect on HDL-C, triglycerides, and fasting insulinaemia. The effect of legumes on blood pressure is controversial, with a benefit only reported in overweight or obese individuals.70
Despite the questionable results of the above meta-analyses, with doubts as to whether their effects on CVD and T2DM are neutral or beneficial, no large prospective study has found legume consumption to be harmful to health. Due to the smaller sample size of the PREDIMED substudy, the higher risk of all-cause and CVD mortality associated with legumes should be considered an unconfirmed exception.68 Evidence from RCTs also suggests a cardiometabolic benefit of legumes.67 These foods are usually preserved dried, in which case their culinary preparation requires rehydration by soaking for 8−12 hours; they are mainly consumed after boiling or as a garnish when eaten cold. In view of the above and the excellent nutritional density of legumes, a minimum consumption of 2 servings (200 g) per week is recommended and, if possible, 4 servings per week.
Levels of evidence on legumes and cardiovascular risk
CerealsCereals, the edible seeds of grasses such as wheat, rice, corn, maize, barley, oats, rye, etc., are the main source of energy for human populations on a planetary scale. This is due to their richness in complex carbohydrates (65%–75% of their weight) and moderate protein content (3%–16%), although they are biologically incomplete, lacking lysine and, in the case of maize, tryptophan. In addition, cereals contain little fat (1%–6.5%, mostly unsaturated) and, like other seeds, when whole grain, are rich in fibre, B vitamins, vitamin E, non-sodium minerals (potassium, calcium, magnesium, phosphorus, iron, zinc, and silicon) and other phytochemicals with antioxidant activity (polyphenols).64 Whole grain cereals retain the 3 components of the grain (bran, endosperm, and germ) in the same proportions as the intact grain. The industrial refining of cereals results in products rich in starch and protein, with good digestibility and a pleasant taste after cooking (white rice), or the production of flour derivatives (white bread), but most of the vitamins, minerals, and healthy phytochemicals found in the outer protective layer (bran) or germ (embryo) are lost.
Cereal intake has a beneficial effect on health, especially wholegrain. For example, a meta-analysis of 48 RCTs comparing refined and wholegrain cereals to assess effects on glycaemic control variables concluded that the latter achieved significant reductions in glycaemia, insulinemia, glycosylated haemoglobin (HbA1c), and HOMA-IR.71 Consistent with this beneficial effect on glucose metabolism, the umbrella review by Neuenschwander et al.15 of 12 meta-analyses evaluating the association of whole grain intake with the risk of T2DM concluded with a high level of evidence that an increased intake of 30 g/day of whole grains and 10 g/day of dietary fibre from these foods is associated with a reduction in the risk of T2DM of 13% and 15%, respectively. In the same review, higher consumption of refined cereals had a neutral effect on the incidence of T2DM in 14 meta-analyses. With regard to lipid control, a network meta-analysis of 55 RCTs comparing different cereals and brans concluded that only oat bran and whole oats, which are rich in soluble fibre (beta-glucans), had a hypocholesterolaemic effect, with a mean reduction in LDL-C of about 10 mg/dl.72 Whole grain consumption has also been associated with a lower risk of incident CVD, as shown in a meta-analysis of observational studies in which the risk of CVD, CHD, CVA, and all-cause mortality was reduced by 8%, 6%, 2%, and 6%, respectively, for each 30 g/day increase, with a dose-response effect in which higher consumption was associated with greater risk reduction.73 Similarly, the aforementioned meta-analysis of observational studies by Bhandari et al.50 showed that high whole grain intake was associated with a 13% reduction in the risk of CVD death (HR: .87; 95% CI: .80–.95).
An essential component of wholegrain cereals is fibre, which is partly responsible for the beneficial effects of their regular consumption. It consists of carbohydrates that are resistant to digestion and absorption in the small intestine and are partially or completely fermented in the large intestine. Its chemical nature is heterogeneous (polysaccharides, oligosaccharides, lignin, and similar substances) and it can be soluble or insoluble. Its presence is important in wholegrains (it is mostly insoluble in wheat and maize, and mostly soluble in oats and barley). Wholegrains contain up to 20 g/100 g of insoluble fibre, which is effective against constipation and regulates intestinal transit, while the soluble form favours the control of cholesterol and glycaemia. By increasing satiety, both types of fibre help to control body weight; a meta-analysis of RCTs in patients with T2DM concluded that fibre consumption favourably modulates the gut microbiota, lipid profile, C-reactive protein, and adiposity.74 There is good evidence that dietary fibre from whole grains is strongly associated with a lower incidence of T2DM, with a HR: .75; 95% CI: .65–.86 per 10 g/day increase, whereas there was no effect of dietary fibre from vegetables.15 There is also evidence from a recent meta-analysis of 64 prospective studies that high dietary fibre intakes were associated with significant reductions in all-cause, CVD and cancer mortality of 23%, 26%, and 22% respectively.75 The complete meta-analysis by Reynolds et al.13 confirmed the beneficial effects of dietary fibre on cardiometabolic risk factors and all-cause, CVD, and cancer mortality. These authors suggest that the consistency of findings from RCTs and prospective studies, together with dose-response relationships, support a causal relationship between dietary fibre consumption and beneficial effects on mortality and incidence of CVD, T2DM, and cancer. The recent meta-analysis by Jenkins et al.14 confirmed the beneficial effects of wholegrains and fibre. Thus, there is ample evidence that dietary fibre, particularly from cereals, is an essential component of a heart-healthy diet.
Quinoa, chia, and buckwheat are pseudo-cereals whose seeds are among the few plant foods rich in high-quality proteins, which, unlike cereals, contain all the essential amino acids in proportions ranging from 12% to 20%. They are also rich in fibre and healthy micronutrients such as vitamins, non-sodium minerals, phytosterols, polyphenols, and other antioxidants. Their consumption helps to control weight due to their satiating effect and has a beneficial effect on cardiometabolic risk factors, although at the moment there are no epidemiological data on their effect on cardiovascular health because of their limited consumption; pseudo cereals are also gluten-free and are therefore recommended for people with coeliac disease.76
Levels of evidence on cereals and cardiovascular risk
| Evidence | Level |
|---|---|
| • Consumption of wholegrain cereals and their fibre promotes better glycaemic control and is associated with a reduced risk of T2DM | Strong evidence |
| • A diet rich in wholegrain cereals or their fibre improves lipid profile, aids weight control, and is associated with a reduced risk of total CVD, CHD, CVA, and CVD and cancer mortality | Moderate evidence |
To promote cardiovascular health and reduce cardiometabolic risk factors, particularly glycaemic control, the recommended cereal intake is approximately 4 servings per day, including bread at all meals of the day, pasta 2–3 times per week, and rice 2–3 times per week. It is advisable to eat wholemeal bread, but white bread is usually consumed in the Mediterranean diet, and wholemeal rice or pasta is rarely used; however, refined cereals are not consumed on their own, but with other foods (bread), in combined dishes (such as paella) or mixed with sofrito, which increases their palatability and reduces their glycaemic index, allowing more vegetables to be consumed. It is interesting to note the sensible habit of combining cereals and legumes in the same meal (e.g. rice with lentils), which supplements the amino acids that are lacking in each food, resulting in a complete mix of proteins with a high biological value. Eating both types of food has been shown to have cardiovascular benefits and also provides fibre, another essential part of a healthy diet.
Eggs, meat, and fishEggsEgg dishes, especially hen's eggs (fried in olive oil, scrambled, in omelettes, or as an accompaniment to salads) are part of Mediterranean gastronomic culture. Eggs contain ovalbumin, a protein of high biological value that contains all the essential amino acids, minerals (selenium, phosphorus, iodine, and zinc), vitamins (A, D, B2, B12, pantothenic acid, and niacin) and other carotenoids such as lutein and its isomer zeaxanthin, the consumption of which has been associated with improvements in insulin sensitivity, oxidative stress, and inflammation, and are structural pigments of the retina, which are very important for eye health. Eggs also contain alpha-glucosidase, dipeptidyl peptidase, and angiotensin converting enzyme inhibitory peptides with potential antidiabetic and antihypertensive effects.77 Eggs are an important source of choline, an essential nutrient involved in the formation of cell membranes, and an adequate dietary intake is important for pregnant women as a deficiency can lead to neural tube defects in the foetus. Egg fat, which represents 11% of the edible portion, is found in the yolk and is mainly composed of triglycerides and cholesterol, with a cholesterol content of around 200 mg–230 mg per unit (350 mg–385 mg per 100 g) and a SFA content of 3 mg per 100 g, which is lower than the unsaturated fat content: MUFAs (5 g/100 g) and PUFAs (1.2 g/100 g).32
Due to its high cholesterol content, egg consumption has traditionally been associated with an increase in total cholesterol and LDL-C, and this is one of the reasons for its restriction in dietary recommendations for cardiovascular prevention. However, intestinal cholesterol absorption ranges greatly from 29%–80%, depending on the activity of the Niemann-Pick C1-like-1 receptor in enterocytes, which modulates cholesterol uptake.78 Egg consumption causes a modest increase in total cholesterol and LDL-C, with a predominant production of large and low atherogenic LDL, as well as an increase in HDL-C that seems to be associated with enhancing its function, without increasing atherogenic ratios, such as LDL-C: HDL-C, or triglyceridemia.8,79
A study of 177,000 participants from 3 large cohorts in 50 countries found no significant association of egg consumption with increased blood lipids, blood pressure, CVD incidence, or cardiovascular mortality.80 Another large population-based study in China found that consumption of one egg per day was associated with a lower risk of CVD (HR: .89, 95% CI:.87−.92), as well as ischaemic (HR: .90, 95% CI: .85–.95) and haemorrhagic (HR: .74, 95% CI: .67–.82) CVA compared with no consumption.81 A meta-analysis of 23 prospective studies found no significant association between egg consumption and increased CVR (HR: .99; 95% CI: .93–1.0682 and these results were similar to those of another meta-analysis that analysed 24 observational studies83 and to the data presented in a recent AHA review of its document on dietary cholesterol recommendations.8 In the Spanish EPIC cohort of 40,621 individuals followed for 18 years, no significant association with CVD and all-cause mortality was found when comparing the quartile with the highest and lowest egg consumption.84
However, not all results are homogeneous. In the follow-up of 6 North American cohorts, a direct association was observed between egg intake and the risk of CVD and all-cause mortality, with hazard ratios of 1.06, 95% CI 1.03–1.10, and 1.08, 95% CI 1.04–1.11, respectively, for each additional half egg per day; however, the relationship was no longer significant after adjusting for dietary cholesterol intake.85 Another meta-analysis found that higher egg consumption was associated with a modest increase in CVD and all-cause mortality, but when subgrouped by geographical area, the increased risk of egg consumption was found in US cohorts, with borderline values in European cohorts and no risk in Asian cohorts.86 Egg consumption has also been reported to be associated with a lower risk of CVD. For example, in another recent large meta-analysis that analysed 39 prospective studies involving almost 2 million people, a reduction in CVD incidence was observed with consumption of up to one egg per day, with an RR: .94, 95% CI: .89–.99.87
An aggregate analysis of US cohorts found an association between egg intake and increased risk of T2DM, but this association has not been found in other European and Asian studies,88 suggesting that the way eggs or accompanying foods are cooked (e.g., different types of oil, fried potatoes) may influence the divergent results in different cohorts.89
In summary, increased egg consumption appears to have a neutral or modest beneficial effect on CVR in the general population, whereas in participants with T2DM, observational studies tend to show an increase in CVR, while clinical trials show no adverse effect.90 Therefore, there is no strong evidence for restricting the consumption of such nutritious and versatile foods as eggs to reduce CVR or improve metabolic control11 and they can be enjoyed as part of a healthy diet.8,91
Levels of evidence on eggs and cardiovascular risk
| Evidence | Level |
|---|---|
| • Egg consumption is not harmful and can be part of a healthy diet. There is insufficient evidence to restrict egg consumption to reduce CVR or improve metabolic control | Moderate evidence |
| • Both the general healthy population and people with risk factors, a history of CHD or T2DM can consume up to one egg per day without increasing their CVR | Weak evidence |
Like fish and eggs, meat is rich in high biological value protein, but relatively high in SFAs, mainly palmitic (C16:0) and stearic (C18:0), although it is also an important source of MUFAs.32 They also contain cholesterol, but also other beneficial nutrients (vitamins such as B12 and niacin, and minerals such as iron, potassium, phosphorus, selenium, and zinc). The fat content of different types of meat varies: white meat (poultry and rabbit), which is not red because it contains little myoglobin, has a lower fat content than red meat, and pork has a lower fat content than beef or lamb. The fat content is also strongly influenced by the anatomical origin of the meat, being lower in pork loin than in ribs or belly. In lamb it is lower in leg than in chops, and in veal the fat content of the flank is four times that of the loin. Another important factor is how the animal is fed, which changes both the quantity and quality of its fat. Grass-fed cattle contain less intramuscular fat than feedlot cattle, but the quality of the fat also varies between species, as dietary changes are less pronounced in ruminants than in monogastric animals such as pigs and poultry, because microbial action in the rumen converts dietary unsaturated fatty acids into SFAs. Lean pork has a high MUFA content (oleic acid), which represents 44% of the total fatty acids in the fat of white pigs and 49% in Iberian pigs, both fed with feed, with a higher content (55%) in Iberian pigs fed with acorns (which make their diet richer in unsaturated fats).
Omnivorous diets include 2 types of red meat, "natural" (unprocessed) red meat and meat derivatives (processed meat) such as sausages, bacon, cold cuts, and cured meats, which have been shown in epidemiological studies to have different effects on cardiovascular health and diabetes. Processed meats contain the same proportions of SFAs and cholesterol as unprocessed red meat, but are less healthy because they have been processed by salting, curing, fermenting, smoking, or other processes to preserve them and enhance their flavour, and therefore often contain salt and additives such as nitrites, nitrates, and nitrosamines.32
The evidence from recent epidemiological studies on meat consumption and the risk of CVD, T2DM, and mortality is controversial. After analysing 43 observational studies on CVD and 27 on T2DM, a systematic review and meta-analysis showed that consumption of unprocessed red meat (per 100 g/day increment) is associated with an increased risk of CVD of 11%; 95% CI: 5–16, and that of processed red meat (per 50 g/day increment) with a greater increase of 26%; 95% CI: 18–35, with similar associations with the risk of T2DM.92 For the specific risk of CHD, another meta-analysis concludes that consumption of unprocessed red meat (per 50 g/day increment) is associated with an increased RR of 9%; 95% CI: 6–12, while for an equivalent higher intake, processed meat is associated with an increased risk of 18%; 95% CI: 12−25: 95% CI: 12–25, while white meat does not increase the risk.93 Results from another meta-analysis suggest that white meat consumption does not increase the risk of CVD, cardiovascular mortality, or T2DM.94
In any case, the conclusions of a recent meta-analysis of 37 prospective studies95 and the umbrella review of 29 reviews and meta-analyses97 are that the evidence for an association between consumption of unprocessed red meat and the risk of CVD, T2DM, and mortality from these causes is weak, and it is not possible to make firm recommendations. The review by Hill et al.96 suggests that processed meat intake is consistently associated with an increased risk of T2DM, but finds weak evidence for an association between processed meat and CVD risk. On the other hand, red meat consumption has a negligible effect on lipid profile,97 glycaemic control,98 or inflammation.97,98 Industrial meat processing often involves high-temperature cooking, which can produce heterocyclic amines and polycyclic aromatic hydrocarbons that increase CVR99; these harmful molecules are also produced during stewing, especially when the meat is blackened.
When assessing dietary protein sources, it should be noted that isocaloric replacement of red and processed meat with other animal protein sources, such as oily fish, yoghurt, cheese or eggs, is associated with a 15%–24% reduction in the risk of CVD.100 Similarly, replacing red and/or processed meat with poultry is inversely associated with CVR, 101 suggesting that it is a healthier alternative to eating red or processed meat. Finally, a dietary pattern of reduced red meat intake appears to reduce CVR, especially when replaced by other sources of animal protein100,101 and especially plant protein such as nuts and legumes,102 while contributing to environmental sustainability due to the significant carbon footprint and water consumption involved in red meat production.103
Levels of evidence on meat and cardiovascular risk
| Evidence | Level |
|---|---|
| • Consumption of processed meats (sausages, cold cuts, cured meats, etc.) is associated with an increased risk of CVD, T2DM and all-cause mortality and is therefore not recommended, except occasionally | Moderate evidence |
| • Unprocessed meat should be eaten in moderation, no more than 3−4 times per week, preferably poultry, lean red and white meat with visible fat removed before cooking. To improve the sustainability of the diet and reduce its carbon footprint, it is desirable to reduce the consumption of meat and increase the consumption of foods rich in plant protein | Weak evidence |
Fish and seafood are the main dietary source of long-chain n-3 PUFAs, including eicosapentaenoic acid (EPA, C20:5n-3) and docosahexaenoic acid (DHA, C22:6n-3), which are abundant in the flesh of oily fish (sardine, anchovy, tuna, herring, mackerel, salmon, trout, etc.),while the flesh of white fish (cod, hake, anglerfish, monkfish, sole, megrim, etc.) and shellfish contain smaller amounts.32 These fatty acids accumulate in the liver of fish, with cod liver being the usual source of fish oil, a concentrate of n-3 PUFAs. In general, wild fish contain more n-3 PUFAs than farmed fish, depending on the type of feed they receive and varying according to the season, with higher fat content in summer.
The benefits of fish consumption, especially oily fish, are often attributed to its richness in n-3 PUFAs, which have a variety of beneficial cardiometabolic effects,104 summarised in Table 2, but other nutrients in fish and seafood (amino acids such as taurine, minerals such as potassium, magnesium, calcium, phosphorus, selenium, iodine, iron, and zinc, and vitamins such as riboflavin and vitamin D) may also contribute to its effects on cardiovascular health.
Beneficial cardiometabolic effects of n-3 PUFAs.
|
PUFAs: polyunsaturated fatty acids; LDLs: low-density lipoproteins.
It is important to distinguish between the cardiovascular effects of fish oil supplements or pharmacological doses of n-3FA and those of eating fish and seafood as natural foods.
Supplements of n-3 PUFAs, in pharmacological formulations with varying combinations of EPA and DHA or in the form of fish oil, have been used in numerous clinical trials to reduce CVR, but in general no beneficial effects have been demonstrated. A notable exception was the REDUCE-IT trial,105 a large randomised clinical trial conducted in patients with moderate hypertriglyceridaemia (triglycerides between 135 and 499 mg/dl) at high CV risk due to established CVD or T2DM and additional risk factors, treated with statins, and with well-controlled LDL-C. In this study, n-3 PUFA supplementation in the form of icosapent ethyl, a highly purified ethyl ester of EPA, at a dose of 4 g/day reduced the incidence of CVD by 25% compared with placebo (mineral oil) after 4.9 years of follow-up (HR: .75, 95% CI: .68–.83).105 This study found a mean 20% reduction in triglycerides, which was not associated with a reduction in CVD events. Other large clinical trials using mixed EPA/DHA formulations at doses of 1 g–4 g/day found a reduction in triglycerides but no reduction in CVD risk.106 These inconsistent results, despite similar reductions in triglycerides, are due to differences in the effects of EPA and DHA on cell membrane and endothelial function; a higher concentration of EPA during icosapent ethyl treatment is associated with superior antioxidant, anti-inflammatory, and plaque stabilising effects than DHA, which may influence CV risk reduction beyond triglyceride reduction.104,106 EPA, but not DHA, has also been shown to be effective in reducing CVD risk in patients with T2DM.107 An unsuspected adverse effect of high-dose n-3 FA therapy, including icosapent ethyl, is the occurrence of atrial fibrillation, most commonly at doses >1 g/day.108 Except in special cases of high residual CVR, where icosapent ethyl may be indicated, n-3A supplements are not recommended for CV prevention.
Regarding intake of the natural source of EPA/DHA, a recent systematic review of 24 observational studies shows that higher consumption of non-fried fish is directly associated with lower CVR and myocardial infarction risk,109 and a recent meta-analysis concludes that weekly consumption of 2–3 servings of fish (150 g per week) moderately reduces CVR (RR: .93; 95% CI: .91–.96).110 In follow-up of 3 large cohorts of patients with a history of CVD, lower CV risk (HR: .84; 95% CI: .73–.96) and total mortality (HR: .82; 95% CI: .74–.91) were observed in those who consumed 2 servings (about 175 g) of fish per week compared with those who consumed less than 50 g per month. Consumption of oily fish, but not other types of fish, was significantly associated with a lower risk of CVD, with a 6% reduction per 5 g increment of intake in patients with a history of CVD, but not in the healthy population.111 Similarly, a recent meta-analysis shows that the cardiovascular benefit of fish consumption is attributable only to oily fish, with an inverse association between fish consumption and cardiovascular mortality (RR: .83; 95% CI: .70–.98) and all-cause mortality (RR: .97; 95% CI: .94–.99), with no effect of white fish.112 Another meta-analysis confirms that a higher intake of n-3 PUFAs from oily fish is associated with a reduction in cardiovascular mortality (RR .87, 95% CI .85–.89).113 In most prospective studies and meta-analyses, fish consumption is associated with modest reductions in the risk of total CVD and CHD, but data on CVA are conflicting.
Recently, a large study with pooled data from over 180,000 participants from 29 international cohorts described an inverse association between circulating concentrations of EPA and DHA (an objective biomarker of intake) and the risk of ischaemic CVA, with reductions of 18% and 14%, respectively, when higher and lower concentrations of EPA and DHA were compared.114 A not inconsiderable benefit could be obtained if fish replaced meat as the main course at mealtimes, providing a healthy source of protein in the diet and contributing to a significant reduction in coronary risk.100 All this evidence supports the recommendation to eat at least 2 portions of fish a week, preferably oily fish.3
The presence of contaminants in fish (such as methylmercury, dioxins, and polychlorinated bisphenols) has raised concerns about the safety of fish consumption, as the protective effect of fish on CVR appeared to be attenuated by exposure to polychlorinated bisphenols.115 However, in the follow-up of the PREDIMED cohort, the benefit of fish consumption outweighed the potential risk of contaminants,116 which are more abundant in fish such as mackerel, swordfish, dogfish, bluefin tuna, and shark.
Levels of evidence on fish, shellfish, and cardiovascular risk
| Evidence | Level |
|---|---|
| • Consuming fish or seafood at least 3 times a week, including 2 times a week in the form of oily fish, is recommended to reduce the risk of total CVD and cardiovascular and all-cause mortality. Replacing meat with fish as a main meal provides a proportionately greater benefit | Moderate evidence |
| • Although fish (especially larger, predatory fish) may contain contaminants such as methylmercury, the benefits of fish consumption in the context of a Mediterranean diet appear to outweigh the potential risk of exposure to contaminants. However, pregnant women and children should avoid eating potentially contaminated fish such as bluefin tuna, dogfish, swordfish, and mackerel | Moderate evidence |
| • Consumption of commercial fish oil preparations, which may contain other additives and added fats, is not recommended | Moderate evidence |
The natural function of milk is to nourish and support the growth of mammalian offspring, and therefore it contains all the essential nutrients as well as several anabolic hormones. Milk and dairy products are complex foods, providing (per 100 ml) macronutrients such as carbohydrates (5 g), protein and fat (about 3 g each), and minerals such as potassium, phosphorus, magnesium, and calcium.117 The majority of milk fat is made up of the characteristic odd-chain SFAs, pentadecanoic (C15:0) and heptadecanoic (C17:0) acids. In addition to being the most important dietary source of calcium (116 mg/100 ml), dairy provides micronutrients such as vitamin D, deficiency of which has been linked to a range of diseases from mental health problems to cancer, although the only clear scientific evidence is that it is associated with osteoporosis. However, in intervention trials, vitamin D supplementation has not shown any cardiovascular benefit compared with placebo.118,119 Calcium supplementation has also shown no effect on CVD or all-cause mortality.120
Another potential cardiovascular health benefit of dairy products is the presence of vasoactive peptides, which have an antihypertensive effect through inhibition of angiotensin-converting enzyme.121 One meta-analysis found an association between total dairy consumption and a low risk of HTN,122 and another meta-analysis of cohort studies found a similar association for low-fat dairy, milk, and fermented milk consumption, with mean risk reductions of 14%, 6%, and 5%, respectively.123 In addition, several epidemiological studies have concluded that plasma concentrations of milk-specific C15:0 and C17:0 fatty acids are associated with a reduced risk of CHD and T2DM.124 A meta-analysis of 16 prospective studies shows that circulating or adipose tissue concentrations of C15:0 and C17:0 and a naturally occurring trans fatty acid found in milk, trans-palmitoleic acid, are inversely associated with the risk of T2DM125 and another meta-analysis of observational studies finds that higher concentrations of these two odd-chain SFAs are associated with lower CVR.126 These biomarkers are being used to study the influence of dairy fat consumption on cardiometabolic health.127
Irrespective of their fat content, dairy products have little effect on cholesterol levels and adiposity,122,128 and there is consistent evidence that consumption of dairy products, whether full-fat or low-fat, does not increase CVR and may even decrease it.117 After more than 9 years of follow-up, the multinational PURE study showed that consumption of more than 2 servings of dairy per day was associated with a lower risk of total and CVD mortality compared with no dairy consumption.129 A recent meta-analysis of 55 cohort studies confirms the inverse association between total dairy consumption, comparing higher with lower consumption, and the risk of HTN, concluding that the risk of CHD is reduced by 4% and that of stroke by 10%.130 In terms of cardiovascular health, full-fat dairy products do not appear to have an adverse effect compared with low-fat or skimmed dairy products.131
Higher total dairy consumption is associated with a lower risk of T2DM, although it is important to consider the presence of added sugars in many dairy products, which may counteract this protection. A recent meta-analysis of prospective studies shows that total milk and yoghurt consumption is associated with a 3% and 7% reduction in the risk of T2DM per 200-g/d and 50-g/d increments, respectively.122
The reduced risk of T2DM associated with yoghurt consumption is partly explained by the fact that yoghurt promotes favourable changes in the microbiota of obese individuals and patients with T2DM, with improved glycaemic response and insulin resistance. In addition, yoghurts increase the concentration of glucagon-like peptide (GLP)-1, which has an anorectic effect and may play a role in its protective effect against obesity and T2DM. Consumption of yoghurt and other fermented dairy products has also been inversely associated with the risk of CHD, CVA, and several types of cancer, as well as promoting bone health, largely due to their ability to improve lactose digestion and counteract lactose intolerance.132
Cheese consumption does not alter the lipid profile, as would be expected from its high SFA content. Fermented cheeses contain andrastin, a fungal metabolite with cholesterol-lowering properties, as it inhibits farnesyl transferase, an enzyme that modulates cholesterol synthesis. A systematic review of meta-analyses of cohort studies concludes that higher compared with lower cheese consumption is inversely associated with the risk of all-cause mortality, CVD mortality, and the incidence of CVD, CHD, CVA, and T2DM, with RRs ranging from –7 to –8%.133 However, mature cheese contains significant amounts of salt and would therefore not be recommended in hypertensive patients.
Regarding butter, a meta-analysis found that its consumption was weakly associated with all-cause mortality (RR: 1.01; 95% CI: 1.00–1.03), but not significantly associated with a higher CVR (RR: 1.00; 95% CI: .98–1.02).134 However, replacing dairy fat such as butter or cream with unsaturated vegetable fat is associated with a lower CVR.135
The heterogeneity of dairy products may make it difficult to draw conclusions, as the benefits attributed to dairy products in general may be different for each specific dairy product, given the large number of products available, ranging from whole milk to fermented milk, yoghurts of different types, or milks with very different fat compositions. In the past, to improve cardiovascular health and metabolic profile, the consumption of low-fat or skimmed dairy products was commonly recommended to reduce the dietary intake of SFAs present in full-fat dairy products. However, the presence of other nutrients and even some SFAs or TFAs with beneficial properties in dairy products gives the consumption of the food (in this case full-fat dairy products) as a dietary matrix a benefit greater than that of its constituent nutrients analysed independently, and it does not seem a good strategy to restrict or eliminate full-fat dairy products from the diet in order to reduce CVR.136 Apart from their lower caloric content, consumption of low-fat or skimmed dairy products does not show better cardiovascular outcomes compared to full-fat dairy products in the different studies reviewed.131
In conclusion, there is moderate- to high-quality evidence that the intake of whole milk, cheese, and yoghurt has a neutral or slightly beneficial effect on the risk of CVD, and we can state that their consumption, regardless of their fat content, does not increase CVR or T2DM. Therefore, there is no compelling argument to restrict the intake of full-fat dairy products in order to reduce the incidence of CVD or T2DM, although dairy products with added sugars should be discouraged. For better cardiovascular prevention, it is advisable to reduce the consumption of concentrated dairy fat, such as butter and cream, and replace it as a cooking fat with other sources of unsaturated fat, such as EVOO.
Levels of evidence on dairy and cardiovascular risk
| Evidence | Level |
|---|---|
| • Dairy products, whether whole or skimmed and fermented or non-fermented, have a neutral or moderate effect on reducing CVR | Moderate evidence |
| • It does not seem appropriate to limit the consumption of full-fat dairy products in order to reduce the incidence of T2DM or CVD | Moderate evidence |
| • It is recommended to consume at least 2 portions of whole or skimmed dairy products per day, although the consumption of dairy products with added sugar is discouraged | Moderate evidence |
| • Dairy consumption, especially yoghurt, is associated with a reduced risk of T2DM | Moderate evidence |
| • Cheese consumption is not associated with increased CVR | Moderate evidence |
Nuts (almonds, hazelnuts, walnuts, pistachios, cashew nuts, macadamia nuts, pine nuts, pecans, etc.) are peculiar fruits because of their high fat content, which usually exceeds 50% of energy, but mainly composed of unsaturated fatty acids, either oleic MUFAs (in almonds, hazelnuts, etc.) or linoleic n-6 PUFAs (pine nuts, pecans, walnuts) and n-3 such as α-linolenic acid (walnuts), while they contain few SFAs. Peanuts are legumes, not tree fruits, but their composition and high content of unsaturated fatty acids make them similar to nuts, both nutritionally and in terms of their biological effects. Apart from their high fat content, nuts, like all seeds, are rich in fibre, potassium, calcium, magnesium, and other biologically active phytochemicals such as phytosterols and polyphenols. These are largely found in the skin, so it is best to eat nuts raw, unpeeled, and unroasted. They are also an important source of plant protein, especially almonds and pistachios.137
Interest in nuts has been sparked by consistent epidemiological evidence that regular nut consumption reduces CVD risk and mortality. A recent meta-analysis that pooled evidence from 89 articles, including data from 23 previous meta-analyses, compared consumption of one serving of nuts per day (28 g) with no consumption and found an association with a 21% reduction in CVD risk (including incidence and mortality from CHD, atrial fibrillation, and CVA mortality) and a 22% reduction in all-cause mortality.138 Although a reduction in DM mortality was observed, there was no association with DM incidence. Another meta-analysis of observational studies confirms the lack of association between nut consumption and DM incidence,139 despite a probable effect of increasing insulin sensitivity, although no improvements in blood glucose or HbA1c140 were observed.140 Although RCT data on nut consumption and blood pressure are controversial, there is consistent evidence from prospective studies of their association with a reduced risk of HTN.141 The PREDIMED CVD primary prevention trial provided the first scientific evidence of the benefit of nut consumption, demonstrating a 28% reduction in the incidence of CVD (myocardial infarction, CVA, or death from these causes) after 5 years of intervention with a Mediterranean diet supplemented with EVOO or nuts (30 g per day: 15 g of walnuts, 7.5 g of almonds, and 7.5 g of hazelnuts) in people with high CVR.5
The cardioprotective effect can be partly attributed to the lipid effects of nuts. Indeed, several RCTs, both in healthy volunteers and in hypercholesterolaemic patients, have shown that daily consumption of an appropriate amount of nuts has a clear and consistent cholesterol-lowering effect. The most studied nuts have been almonds and walnuts, but positive results have also been published from studies of other nuts, such as peanuts, so that the cholesterol-lowering effect can be considered "first class". The reduction in total cholesterol and LDL-C depends on baseline levels, being more effective the higher the baseline cholesterol. There is also a dependence on body mass index, with lean people responding more than obese people.137 A recent meta-analysis of 120 RCTs evaluating the lipid effects of different nuts shows a consistent cholesterol-lowering effect of doses ranging from 30 to 60 g/day, with a mean reduction in LDL-C of 4.25 mg/dl (95% CI, 2. 71−5.42), no change in HDL-C, and a mean triglyceride reduction of 5.31 mg/dl (95% CI: 2.66–7.08), plus a mean apoB reduction (determined in 39 studies) of 3.01 mg/dl (95% CI: 1.58–4.44), again with no change in BP.142 The richness of nuts in PUFAs, phytosterols, and fibre are important determinants of their cholesterol-lowering effect. Consumption of walnuts, but not other nuts, has been associated with improved endothelial dysfunction and reduced circulating markers of inflammation, which could be explained by their different composition compared to other nuts: abundance of plant-based n-3 PUFAs (alpha-linolenic acid), arginine (a precursor of nitric oxide), and highly bioactive polyphenols.137
Because nuts are very high in fat and calories, there has been concern that their frequent consumption is associated with undue increases in body weight. There is now sufficient RCT evidence that nuts, whether added to the usual diet (without advice to balance calories by reducing consumption of other foods) or as a replacement for another source of dietary fat, do not cause weight gain. Furthermore, in prospective studies, regular nut consumers tend to be leaner and gain less weight during follow-up than non-consumers.141 The main explanation for this apparent contradiction is the high satiating capacity of nuts, which (as long as they are eaten during the day or as a snack) compensates for the calories consumed by limiting consumption at the next meal. In addition, depending largely on the chewing and subsequent fragmentation of nuts, part of the fat (up to 20%) is not absorbed by the intestine because it is contained in cell membranes within solid particles, making the energy absorbed lower than would be predicted from their composition, while implying some faecal fat loss, which may be associated with softer than usual stools.137,143
Levels of evidence on nuts and cardiovascular risk
Frequent consumption (daily or at least 3 times a week) of a handful of nuts (equivalent to a 30 g serving) is highly recommended for cholesterol control and general health. It is best to eat them raw and unpeeled (not roasted or salted) as most of the antioxidants are in the skin. To maintain their satiating effect, they should be eaten during the day and not as a dessert after dinner. This recommendation can be made for people of all ages (from 5 years); the only contraindication is a rare nut allergy (the most common is peanut allergy in childhood).
Cocoa and chocolateCocoa, the basic ingredient of chocolate, shares with other seeds a favourable composition of nutrients and phytochemicals. It contains 40%–50% fat in the form of cocoa butter, made up of 33% oleic acid, 33% stearic acid, and 25% palmitic acid. It also contains polyphenols, which make up 10% of the dry weight of the seed, making it one of the richest natural foods in phenolic compounds. Its main product for consumption is chocolate, of which there are many varieties with different ingredients. Dark chocolate has the highest cocoa content and the lowest milk and sugar content; its composition includes 50% complex carbohydrates, 35% fat, and up to 7% protein, as well as abundant potassium and magnesium, phytosterols, and polyphenols.143 These are flavonoids, particularly flavanols, which are highly bioactive because they increase the production and bioavailability of nitric oxide, reduce oxidative stress in the vascular endothelium and promote vasodilation and blood flow.145 Although much of the fat in cocoa is made up of SFAs, stearic acid predominates, which does not have a hypercholesterolaemic effect.36
A recent systematic review of meta-analyses analysing data from large prospective cohort studies with different food exposures concludes that there is consistent evidence of a significant relative risk reduction for CVD (CHD, myocardial infarction, and CVA) of 4%–10% for each 10 g/day of chocolate intake.146 The results of another meta-analysis of prospective studies evaluating the dose-response of chocolate with the risk of chronic diseases confirmed an inverse association with the risk of CHD and CVA for doses up to 20 g/day, with no major benefit above this dose.147 Another recent meta-analysis of cohort studies with nearly 900,000 participants examined chocolate consumption in relation to mortality risk and found a modest inverse association of increased consumption with all-cause, CVD and cancer mortality, with significant RRs between –5% and –10%.148 Exceptionally for a food, an RCT of consumption of a flavanol-rich cocoa extract (500 mg per dose) compared to placebo was conducted with a primary endpoint of CVD incidence, the COSMOS trial, which included almost 21,500 participants in primary prevention.149 After a mean intervention period of 3.6 years, the incidence of CVD in the cocoa extract group was similar to that in the placebo group (RR: .90; 95% CI: .78–1.02; p = .11). However, a beneficial effect of cocoa extract was observed for one of the secondary endpoints (CVD mortality), with an HR: .73; 95% CI: .54−.98. The results are encouraging and suggest that a significant reduction in CVD risk may have been achieved with longer follow-up. A COSMOS sub-study of approximately 18,300 participants without T2DM at baseline showed no effect of cocoa extract on the incidence of T2DM (HR: 1.04; 95% CI: .91–1.20; p = .58).150
Numerous RCTs have been conducted with cocoa drinks, dark chocolate (containing at least 50% cocoa) or similar products to assess their effect on cardiometabolic risk variables, demonstrating a consistent effect of improved endothelial function and reduced BP and cholesterolaemia, with increased HDL-C; improved glycaemic control, insulin resistance, and inflammation have also been reported.144 A recent meta-analysis of 31 RCTs evaluating the effects of cocoa products on BP shows a greater antihypertensive effect with chocolate than with cocoa drinks and in hypertensive subjects than in normotensive subjects.151 Notably, some of these clinical trials have used flavonoids isolated from cocoa rather than chocolate, showing the same beneficial effect on BP and endothelial function, suggesting that these phytochemicals are a major bioactive component of cocoa. Despite its energy richness, there is no evidence that frequent consumption of dark chocolate is fattening; on the contrary, studies suggest an inverse association between cocoa flavonoids and adiposity152 and the incidence of T2DM.153
However, many chocolates and other cocoa products on the market have a low concentration of cocoa and contain added simple sugars and other vegetable oils, making them unsuitable for cardiovascular health.
Levels of evidence on the relationship between cocoa/chocolate and cardiovascular risk
Dark chocolate can be consumed frequently, up to 20 g per day, to reduce cholesterol, BP, and CVR as part of a healthy diet. There is no concern that regular consumption of dark chocolate will cause undue weight gain.
Coffee and teaCoffee and tea are two of the most widely consumed beverages in the world; both are rich in highly bioactive polyphenols as antioxidants and anti-inflammatories, which give them their characteristic bitter taste. Green coffee infusion retains relatively high concentrations of potassium, magnesium and niacin from the original seeds and, in addition to caffeine (an alkaloid with stimulating properties), contains other polyphenols, mainly chlorogenic acid, with antioxidant, antihypertensive, and lipid-regulating properties.154 The richness of these bioactive components in coffee seems to be responsible for its potential benefits on cardiovascular and general health.155
Coffee consumption, with or without caffeine, has been extensively investigated in prospective studies for CVD incidence, T2DM, and general health, and in RCTs for effects on CVR factors, almost always showing beneficial effects.156 There is a non-linear inverse relationship (U-curve) between coffee consumption and CVD, cancer, and all-cause mortality. In a recent meta-analysis, an average intake of 3.5 cups per day, but not higher doses, was associated with a 15% (95% CI 11–18) reduction in the RR of all-cause mortality compared with no coffee consumption.157 In the same vein, a large prospective study based on the UK Biobank cohort shows a lower risk of CVD and all-cause mortality among consumers of up to 5 cups of coffee per day, with a U-shaped association among those drinking coffee with or without sugar, but the association was less consistent when coffee was consumed with artificial sweeteners; benefits appeared with different types of coffee: instant, ground, and decaffeinated.158 A recent meta-analysis of 32 cohort studies concluded that, overall, coffee consumption is not associated with the risk of CHD, although in subgroup analyses it may worsen the risk in men and improve it in women.159 Another meta-analysis of 30 prospective studies describes a direct association of coffee consumption with a lower risk of T2DM, results were similar for caffeinated and decaffeinated coffee160; there is also evidence that regular coffee consumption reduces CVD mortality by 32% and all-cause mortality by 40% in people with T2DM compared with no coffee consumption.161
Coffee can raise blood pressure acutely, but there is no evidence that regular moderate coffee consumption promotes the development of HTN, and it has even been associated with a lower risk of HTN in some studies. Conversely, occasional coffee consumption may temporarily increase BP. In people with HTN, coffee consumption (one to three cups per day) may reduce the risk of all-cause mortality,162 although a large prospective Japanese study shows that in people with grade 2–3 HTN, consumption of two or more cups of coffee per day is associated with an increased risk of CVD mortality compared with no consumption (RR 2.05, 95% CI 1.17–3.59), whereas this association does not exist in normotensive subjects or those with grade 1 HTN.163 In any case, recent international recommendations on lifestyle changes for the management of HTN suggest a daily consumption of 2–3 cups of unsweetened tea or coffee per day.11
Another analysis from the large prospective UK Biobank cohort found that regular coffee drinking in moderate amounts was associated with a reduced risk of supraventricular arrhythmias, with a 3% reduction for each additional cup per day.164 In the Spanish cohorts of the prospective SUN study and the PREDIMED clinical trial, caffeinated coffee consumption (1–7 cups per week) was associated with a combined 40% reduction in the risk of atrial fibrillation.165
Unfiltered coffee contains cafestol, a diterpene that raises cholesterol, but filtered or instant coffee does not.166 A Norwegian study shows that consumption of filtered coffee is associated with lower CVD and total mortality than unfiltered coffee, although both types of coffee appear to be protective compared with no coffee consumption.167
Tea infusions are rich in flavonoid-type polyphenols, particularly catechins, and also contain caffeine. Black tea is made by oxidising the leaves of the Camellia sinensis plant in a controlled environment, while green tea is made from intact leaves. Regular tea consumption has been associated with better cardiovascular health; a meta-analysis shows that regular consumption of both types of tea is associated with lower CVR and all-cause mortality.168 In another analysis of the UK Biobank cohort, tea consumption ranging from 2 to 10 cups or more per day was associated with a 9%–13% reduction in the risk of all-cause mortality, including CVD, compared with non-tea drinkers.169 There is also evidence from a meta-analysis of 55 RCTs that daily green tea consumption moderately reduces BP, total and LDL cholesterol, increases HDL-C and improves glycaemic profiles.170
In conclusion, regular moderate consumption of up to 5 cups per day of coffee (filtered or instant, caffeinated or decaffeinated) or tea (green or black) in doses of up to more than 10 cups per day is beneficial for cardiovascular health; moreover, moderate coffee consumption is inversely associated with the risk of T2DM and tea reduces the potency of CV risk factors. For these reasons, both beverages are recommended for both healthy individuals and those with risk factors. These beverages are acaloric, except when consumed with excess sugar, which should always be limited or eliminated in the case of obesity, T2DM, or atherogenic dyslipidaemia.
Levels of evidence on the association between coffee, tea, and cardiovascular risk
Alcoholic beveragesAlcoholic beverages are those that contain ethanol (ethyl alcohol). Depending on how they are produced, they can be either produced by fermentation, such as wine, beer, or cider, whose alcohol content does not exceed 15 °, or by distillation, such as spirits (whisky, cognac, gin, vodka, or rum) and liqueurs flavoured with fruit, herbs, or spices (alcohol content between 20 ° and 60 °). The effects of alcoholic beverages on health have been a source of controversy and debate, there are both proponents and opponents of their consumption, even in moderation. In any case, it is clear that excessive consumption is harmful, as it is causally linked to numerous health problems, from accidents to alcoholic liver disease, chronic pancreatitis, cardiomyopathy, or neurodegenerative diseases. Numerous epidemiological studies and the systematic analysis of the Global Burden of Disease Study 2020171 suggest that moderate consumption of all types of alcoholic beverages reduces all-cause mortality and, in particular, cardiovascular mortality by about 20% compared with non-drinkers, but this benefit increases from a level of between 20 g and 30 g of ethanol per day, which is represented by the typical J curve. This report indicates that the benefits of moderate alcohol consumption are globally apparent in adults of both sexes from the age of 40 years, but in younger individuals, particularly males, excessive alcohol consumption predominates and associated mortality increases, so that between the ages of 15 and 39 years, any amount of alcohol is considered harmful.171 A recent systematic review of 56 cohort studies involving more than 1.5 million participants confirms the association between moderate consumption of alcoholic beverages and a reduction in cardiovascular mortality, which is notable in the case of wine (25% lower compared to beer or spirits).172 This review also suggests an association between moderate alcohol consumption and a lower incidence of myocardial infarction. A large prospective study of more than 300,000 participants derived from the UK Biobank data also suggests an association between moderate consumption of alcoholic beverages and a reduced risk of T2DM, but only when consumed with meals, such as wine,173 highlighting the importance of considering the pattern of drinking, not just the absolute amount. Indeed, another publication from the same cohort concluded that wine consumption (compared to beer and spirits), drinking it with meals (compared to the same amount but without food), and spreading weekly consumption over 3 or 4 days (instead of daily or binge drinking) are associated with lower CVD mortality and incidence.174 On the other hand, although it is controversial, it is still postulated that alcohol, even in moderate amounts, is a carcinogenic agent, especially for the oral mucosa and the oesophagus enhanced by a synergistic effect with tobacco smoking.175
To date, no RCT has been completed to assess the effects of moderate alcohol consumption on hard events such as mortality or CVD incidence. The University of Navarra Alumni Trialist Initiative (UNATI) study, a randomised controlled trial of a dietary intervention with two parallel groups, has recently been launched. It will enrol 10,000 adults, men aged >50 years and women aged >55 years, with a diagnosis of CVD, T2DM, cancer, or depression, who will be advised to consume moderate amounts of red wine (up to 2 glasses per day for men and up to 1 glass per day for women) with meals or abstain from all alcoholic beverages, and will be followed for at least 4 years to assess effects on total and cardiovascular mortality and incidence of CVD, T2DM, and cancer.176
In the past, the type of alcoholic beverage was not considered to be a determinant of its health effect, which was attributed to its ethanol content, but recent evidence suggests that the health effects of fermented beverages (wine and beer) are greater than those of spirits,177,178 although this remains controversial.179 In this context, many RCTs have analysed the short-term effects of different types of beverages on CVR factors.176–178,180 As alcoholic beverages contain ethanol and other compounds, mainly polyphenols, some of the health effects of these beverages are attributed to their alcohol content and some to the effects of the non-alcoholic components. For example, ethanol is thought to significantly increase HDL-C, improve glucose metabolism, and reduce fibrinogen,180–182 whereas beverages with a higher polyphenol content, such as wine, especially red wine, and beer, would have a greater effect on oxidation and inflammation parameters related to atherosclerosis, as well as on angiogenesis.177,182,183
The consumption of dealcoholized wines and beers, which, due to the absence of ethanol, are not associated with an increase in HDL-C, is currently on the rise, they also have a beneficial effect on the cardiovascular system by reducing blood pressure and increasing circulating endothelial and progenitor cells involved in vascular endothelial regeneration.184,185 In recent years, some of the health benefits of consuming alcoholic beverages, especially red wine, have also been attributed to favourable changes in the gut microbiota due to their high polyphenol content.186–188 Finally, it should be noted that a single RCT conducted in Israel evaluated the effect of long-term moderate wine consumption on CVR factors.189,190 In this study, 150 ml of red wine, 150 ml of white wine, or 150 ml of water were randomly administered daily for 2 years to 3 groups of well-controlled diabetics. Participants receiving red wine had increases in HDL-C and apoA1, and the 2 groups receiving wine showed increased insulin sensitivity, but only if they were slow metabolisers of alcohol.
In summary, although still controversial, moderate consumption of fermented alcoholic beverages (wine and beer) is associated with improvements in CVR factors, mainly increased HDL-C (due to alcohol) and decreased inflammation and oxidative stress (due to polyphenols), and with moderate reductions in total and cardiovascular mortality and the incidence of CVD and T2DM.
Levels of evidence for moderate alcohol consumption and cardiovascular risk
| Evidence | Level |
|---|---|
| • Alcoholic beverages increase HDL-C | Strong evidence |
| • Compared with abstention or heavy drinking, moderate drinking is associated with a reduction in the incidence of CVD, T2DM, and total and cardiovascular mortality | Moderate evidence |
| • Drinking wine in moderation with meals is the least harmful way to consume alcoholic beverages | Moderate evidence |
Alcoholic beverages should always be consumed with meals and as part of a healthy diet, such as the Mediterranean diet. At present, there is evidence that the effects of drinking alcoholic beverages are similar in both sexes (beneficial or harmful, depending on the amount and pattern of consumption). However, as women are more sensitive to alcohol because of their faster absorption, recommendations would be up to 2–3 drinks per day (maximum 30 g of alcohol) for men and up to 1–2 drinks per day (maximum 15 g) for women. Because of their demonstrated capacity to drink to excess, young people should refrain from consuming alcoholic beverages. Men over 65 should also not exceed 20 g of alcohol per day.
Sugar-sweetened and artificially sweetened beveragesSugar-sweetened beveragesWestern diets tend to be high in simple carbohydrates such as sucrose, glucose, fructose, and lactose. Sugar-sweetened beverages are a major source of added sugars in the diet, not only soft drinks, but also dairy products and industrial juices, whose intake provides a low (and temporarily shorter) satiation associated with an incomplete compensatory reduction in subsequent dietary energy intake; their palatability also favours greater consumption, with a consequent increase in dietary calorie intake (Table 3). Due to their characteristics and processing, sugar-sweetened beverages fall squarely into the category of ultra-processed foods that are harmful to health191 (see "Ultra-processed foods" section).
Amount of calories and percentage of recommended daily calories of some beverages.
There is strong evidence from cohort studies and RCTs supporting an aetiological role of habitual consumption of sugar-sweetened beverages in relation to obesity, which is an independent risk factor for cardiometabolic and related diseases, such as CVD and T2DM, as well as some cancers and all-cause mortality.192 Given the role of sugar-sweetened beverages in the current obesity pandemic and their impact on other chronic diseases, there are active policies aimed at reducing their consumption at a global level; an important initiative is the increase in taxes on these beverages, which, by increasing their cost, has had the effect of reducing sales in countries where this measure has been implemented.193 This document only discusses the proven effects of the excessive addition of sugars to beverages, not their natural presence in foods.
There is growing scientific evidence of the harmful effects of excessive consumption of sugar-sweetened beverages, supported by observational studies, reviews, and meta-analyses,15,17,56,194–196 and reflected in international consensus and clinical practice guidelines. According to the most recent meta-analysis, which synthesised data from 70 prospective studies,56 higher consumption of sugar-sweetened beverages is significantly associated with the risk of HTN, T2DM, CHD, CVD, total mortality, and fatal CVD, with RRs ranging from 1.09 (CHD) to 1.27 (T2DM), with a linear dose-response relationship between consumption and the incidence of these diseases.
Avoidance of sugar-sweetened beverages is one of the 10 recommendations on diet and CVD prevention made by the AHA in its position paper of 2021.4 The previous 2017 consensus document by Pérez-Martínez et al. on lifestyle recommendations for the prevention and management of metabolic syndrome194 already pointed in the same direction, as do the current recommendations of the American Diabetes Association, which, in addition to the adverse effects of sugar-sweetened beverages on glucose metabolism, obesity, metabolic syndrome, and T2DM, point to their aetiopathogenic role in non-alcoholic fatty liver disease, a risk factor for cirrhosis and liver cancer.197,198 A recent meta-analysis linked sugar-sweetened beverage consumption to the risk of several types of cancer, particularly breast, hepatocellular, colorectal, and prostate, although the evidence is limited.199 In conclusion, consumption of sugar-sweetened beverages is an important indicator of an unhealthy diet.
Artificially sweetened beveragesThe challenge of replacing sweetened beverages in the general population is enormous. More than 50% of Americans consume at least one sweetened beverage per day, amounting to more than 178 calories per day for men and 118 calories per day for women. Repeated drinking creates a habit where it is difficult to return to drinking water as the primary source of fluid, as people become accustomed to the added pleasure of the taste of sugary drinks.
As an alternative to consuming sugar-sweetened beverages, low-calorie sweeteners are presented as a source of sweet taste without caloric intake. The combination of a caloric advantage over traditional sugars and certain associations with improved metabolic management has led to increased regular consumption, especially as their status as "additives"
has allowed them to bypass food safety studies by major health authorities such as the US Food and Drug Administration and EFSA. This, together with observational studies showing a beneficial effect on weight loss and body fat percentage, has given them a dominant position among soft drink consumers, who now consume them more than the original sugar-based versions. The general public perception of the consumption of these sweeteners is that they are safe and even healthy compared to added sugar. Indeed, a recent meta-analysis supports the safety of these sweeteners, at least on body weight and cardiometabolic risk factors, albeit with a low to moderate level of evidence.200 However, plausible evidence has recently been presented for a possible association between low-calorie sweeteners and obesity, metabolic syndrome, T2DM, and CVD.16
For example, results from a recent RCT suggest that certain sweeteners (saccharin, aspartame, stevia, and sucralose) may alter gut microbiota and glucose tolerance in healthy individuals.201 A large French prospective observational study involving almost 100,000 participants followed for 9 years showed a statistically significant association between the consumption of different sweeteners (aspartame, acesulfame potassium, and sucralose) and the risk of CHD.202 In this vein, another recent study of 3 large prospective cohorts followed for 3 years described an association between a specific sweetener (erythritol) and major adverse cardiovascular events, defined as the composite of CVD death, CHD, and CVA.203 The authors identified increased platelet activation, which persisted even 2 days after exposure to the sweetener, as a possible pathogenesis of the adverse effect of the sweetener. Indeed, data from large cohort studies and several meta-analyses of prospective studies suggest (although with lower levels of evidence) that increased consumption of both sugar-sweetened and artificially sweetened beverages is associated with the risk of CVD, especially CVA, T2DM, and all-cause mortality.17,56,192,195,196,202–205
In summary, current evidence supports the harmful effects of sugar-sweetened beverage consumption, while recent evidence on artificial sweeteners casts doubt on the appropriateness of previous recommendations to replace sugar-sweetened beverages with artificially sweetened ones. While they have a beneficial effect on calorie intake, there is increasing evidence of the harmful effects of sweeteners, which opens up an interesting debate on the need for safety studies not only on these additives in beverages, but also on others present in today's foods, such as colourings, flavourings, etc. Sugar-sweetened beverages are a regular part of the diet of many people around the world and can account for up to 20% of daily calorie intake. Replacing these drinks with water would be essential to reduce energy intake and the risk of obesity, T2DM, and related diseases. If this is not accepted, artificially sweetened beverages provide lower caloric intake, although in this case the patient should be informed of the recent data linking their consumption with the development of CVD, T2DM and all-cause mortality, making them as undesirable as the sugar-sweetened beverages they are intended to replace.
Levels of evidence on the consumption of sugar-sweetened and artificially sweetened beverages, and cardiovascular risk
| Evidence | Level |
|---|---|
| • Frequent consumption of beverages with added sugars promotes insulin resistance, obesity, metabolic syndrome, and incidence of T2DM, while increasing CVR | Strong evidence |
| • Consumption of beverages with added sugars should be avoided, not only soft drinks but also industrial juices and milk drinks. Replacing consumption of sugar-sweetened beverages with water or unsweetened infusions would be important to reduce energy intake and CVR, obesity, metabolic syndrome, and T2DM | Moderate evidence |
| • Recent evidence suggests an increase in cardiovascular and all-cause mortality and the risk of CVA, CHD, and T2DM with increased consumption of artificially sweetened soft drinks, so it does not seem appropriate to recommend their consumption | Moderate evidence |
Sodium is an essential mineral involved in regulating the osmolarity of most extracellular fluids and is essential for cellular homeostasis. Like other minerals such as calcium, vitamin D, and hormones such as thyroxine, sodium has a J-curve relationship with its physiological function, so that both deficiency and excess are detrimental to cellular physiology. Numerous epidemiological studies have shown a direct and dose-dependent relationship between excess salt (sodium chloride) intake and the development of adverse health outcomes, particularly increased systolic blood pressure and CVA.146
Based on the available evidence, the World Health Organisation (WHO) published the first global report on sodium intake reduction in 2023, recommending that dietary sodium intake should be reduced to less than 2 g/day in adults (equivalent to 5 g/day of salt), with lower values in children.206 HTN can be prevented by reducing salt intake207 and dietary sodium restriction is an essential component of lifestyle recommendations for the management of HTN.12
A significant proportion of the salt we consume comes from prepared foods, as the food and drink industry has a vested interest in using excessive amounts of table salt or other sodium salts (nitrites, citrates, alginates, glutamates, etc.) to preserve food, enhance flavour, and increase thirst, often leading to the consumption of industrial beverages. Based on some observational studies, sometimes promoted by the food industry, it has been postulated that a higher CVR is associated with a diet with lower salt intake and that there is a J-curve that could define the relationship between salt intake and CVD. These findings have been refuted due to methodological concerns, in particular inadequate estimation of salt intake based on spot urinary sodium analysis and probable reverse causality, and in no way justify the claim that lower sodium intake could increase CVR.208,209 The most reliable marker of salt intake is 24 -h urinary sodium excretion, preferably in repeated analyses; the same method can be used to measure potassium excretion as a sodium antagonist. In a landmark study using aggregated individual data from 6 large prospective North American cohorts of healthy individuals, sodium and potassium were measured in 24 -h urine several times during a mean follow-up of 8.8 years.210 Comparing urinary sodium and potassium extremes, the HRs of CVD for the higher biomarker level were 1.60 (95% CI 1.19–2.14) for sodium excretion and .69 (95% CI .51–.91) for potassium. A dose-response effect was observed, such that each 1 g daily increase in sodium excretion was associated with an 18% increase in CVR, while each 1-g/day increment in potassium excretion was associated with an 18% reduction in risk.210 The results of this study highlight the adverse effects of excessive sodium intake and the beneficial effects of potassium intake.
Other studies highlight the beneficial effects of reducing dietary sodium. A meta-analysis of RCTs confirms the direct relationship between dietary sodium reduction and BP reduction, which is greater in older populations and those with higher BP. It also shows that short-term studies underestimate the effect on BP of sodium reduction.211 A large prospective study of 176,570 adults from the UK Biobank shows that people who never or rarely add salt to their food have a 23%, 26%, and 37% lower risk of CVD, CHD, and heart failure, respectively, than those who always or very often add salt to their food.212 Participants who added salt to their meals less often and followed a DASH-type diet, which is low in sodium and high in potassium due to the abundance of vegetables and has been shown to lower blood pressure213 (see related section), had a lower CVR.212 Other studies provide consistent evidence that reducing dietary salt reduces BP, CVR, chronic kidney disease, and all-cause mortality.214 According to a large American epidemiological study, excessive sodium intake is considered the first of 10 dietary factors responsible for cardiometabolic disease mortality (CHD, CVA, and T2DM).215 In line with WHO recommendations,206 the World Hypertension League has developed a consensus document to reduce global dietary sodium intake by an average of more than 2 g/day (equivalent to 5 g/day of salt).216
A relevant issue is the different individual behaviour of BP in relation to salt intake, which may increase very much in some individuals and very little in others. This heterogeneity allows people to be classified as salt-sensitive or salt-resistant. The former are thought to have a hypersensitivity of the renin-angiotensin system, so that prolonged salt intake induces renal vasoconstriction and increased tubular reabsorption of sodium, favouring an increase in blood pressure. This salt sensitivity increases progressively with age, is more common in hypertensives, and its heritability is higher in the Black population. Salt sensitivity is thought to have a genetic basis, but there is insufficient data to attribute it to variability in known genes. Knowing whether an individual is salt-sensitive or salt-resistant is clinically relevant because salt sensitivity itself is as strong an independent risk factor for cardiovascular morbidity and mortality as HTN.217 Diagnosis requires assessment of the BP response in repeated measurements after periods of salt overload and salt restriction. In any case, the best public health approach would be to implement public health programmes to limit salt intake at the population level.206,216
A low-salt diet (<5 g/day) should be recommended for the whole population and, more justifiably, for hypertensive patients and their relatives, bearing in mind that to calculate the total amount of salt it is necessary to multiply the sodium content of foods by 2.5. Limiting the consumption of salty foods such as pre-cooked foods, canned foods, salted foods, processed meats, and fizzy drinks is particularly effective. Low-sodium seasonings (Table 4) are available for culinary preparation and to enhance the palatability of foods and can be a healthy alternative to salt. Spices and herbs are sources of antioxidants due to their richness in phenolic compounds and are integrated into healthy culinary traditions such as the Mediterranean diet.
A feasible way to reduce salt intake is to replace salt with potassium-rich salts. An RCT conducted in China in 20,995 people with a history of CVA or over 60 years of age and with HTN in a rural setting, followed for 4.7 years, showed that the group using a salt substitute (75% sodium chloride and 25% potassium chloride) had a 14% reduction in the incidence of CVA, a 13% reduction in total CVD, and a 12% reduction in total mortality compared with the control group who continued to use table salt, with no detectable hyperkalaemia.218 A recent meta-analysis concluded that most studies of replacing salt with high potassium substitutes were conducted in Asian populations and included participants with high and very high CVR, and therefore the evidence for recommending widespread use in other populations is limited.219
In developed countries, about 80% of dietary salt comes from processed and fast foods. In these countries, the strategy to reduce sodium intake should focus on persuading food industry managers to reduce the amount of sodium they add to their products in a gradual and sustainable way, and on advising consumers not to add salt to foods. Ingredients can be added during food processing to improve palatability and shelf life, and are a significant source of sodium in foods ready for immediate consumption that we do not usually identify as high in sodium. For example, many ice creams and chewing gums contain sodium ascorbate (E-301), and biscuits and other confectionery usually contain sodium sorbate (E-201). It should also be remembered that for many people, bread is the main source of sodium in the diet, so it is advisable to choose low-salt varieties.
Levels of evidence on salt intake and cardiovascular risk
| Evidence | Level |
|---|---|
| • Excessive sodium intake is directly associated with HTN, CVD, and cardiometabolic mortality. A low-salt diet (<5 g/day) should be recommended; to calculate the amount of total salt, multiply the sodium content of foods by 2.5 | Strong evidence |
| • Effective measures to reduce dietary sodium intake include limiting consumption of pre-cooked, canned, salted, cured, carbonated and other ultra-processed foods | Strong evidence |
Processing is the manipulation of raw foods to make them suitable for consumption or storage, using techniques to improve their nutritional quality, preservation, safety, and palatability. Since time immemorial, processing has been common to most of the foods we consume and includes any action that begins with preparation and ends with cooking. Cutting damages tissues and brings enzymes and substrates that were normally separated by membranes into contact with each other, which can cause oxidative reactions such as browning of many fruits and vegetables, especially apples, mushrooms, aubergines, etc. It also promotes glucosinolate degradation reactions that produce isothiocyanates, compounds with anti-tumour properties. When cut, the tissues are exposed to atmospheric oxygen, which favours lipid oxidation and rancidity due to spontaneous reactions and loss of moisture.32 With regard to culinary preparation and preservation, several methods are available, the most important being the application of cold or heat and dehydration. Other processes used to a greater or lesser extent, such as fermentation, salting, brining, pickling, curing, smoking, or syruping, are aimed at increasing the shelf life and improving the organoleptic qualities of the food. Finally, packaging can also affect the quality of the food.
Recently, there has been unprecedented scientific interest in the characteristics of food processing inherent to industrial mass production in Western civilisation and the possible health consequences of its consumption. In this context, the concept of ultra-processed foods has been developed, derived from the NOVA classification system, which has undergone several changes in recent years and attempts to systematise the degree of processing of foods and their ingredients.220 According to the NOVA definition, ultra-processed foods are industrial formulations produced by a series of physical, chemical, or thermal changes that alter the natural characteristics of the food; many ultra-processed foods are typically high in total fat, simple sugars and sodium, and high in energy density, and usually contain substances not commonly used in food preparation, such as hydrolysed proteins, modified starches, and hydrogenated oils with industrial trans fats. In general, ultra-processed foods are low in protein, fibre, and micronutrients.191 The aim of the food industry is to obtain low-cost, ready-to-eat products that, in addition to being easy to prepare, have an attractive presentation, pleasant taste and preservation conditions that allow them to be stored and consumed for long periods of time, using flavourings, sweeteners, colourings, stabilisers, emulsifiers, binders, agglomerators, etc.
Foods and beverages classified as ultra-processed include a variety of widely consumed products, (Table 5) which have in common that they are industrially produced.191 It is obvious that most of these foods and beverages fall under the well-known concept of "junk food" or "fast food" and are among the foods traditionally discouraged as unhealthy.3 For this reason, many experts are sceptical about the nutritional value of the concept of ultra-processed foods.19,221–225
Ultra-processed foods of industrial origin.
|
There has been a marked increase in the consumption of these foods in Western diets, replacing other fresh or minimally processed foods in the regular diet and representing a significant calorie intake due to their usually high energy density, although there is controversy about their influence on weight gain.19 Data from Spain are not as alarming, but indicate a progressive increase in the contribution of these foods to the normal diet, which, according to the latest estimates, represents about 30% of the daily energy of the total population, with higher consumption in children and adolescents and in overweight people.226 Despite its limitations and the fact that there is as yet no evidence of causality of these foods in the risk of chronic non-communicable diseases,19 the NOVA definition of ultra-processed foods has been used in numerous nutritional epidemiological studies and derived meta-analyses, with generally consistent results regarding their adverse impact on health. Data from the most recent systematic review (of 45 meta-analyses, with almost 10 million participants) of exposure to ultra-processed foods and their effects on health variables227 show evidence (generally low quality) of an association between increased consumption and all-cause and CVD mortality, and the incidence of CVD, T2DM, obesity, HTN, and metabolic syndrome, with hazard ratios ranging from 1.20 to 1.50. A recent analysis of 3 large cohorts in the US and UK confirms the association between higher consumption of ultra-processed foods and a 16%–17% increased risk of all-cause and CVD mortality.20 In a mediation analysis, this study suggests that biomarkers of liver function and inflammation largely mediate all-cause and CVD mortality.
However, there is great heterogeneity in the set of foods classified as ultra-processed by the NOVA classification 191,220 and although their overall consumption is associated with a higher risk of T2DM, there are specific subgroups of these foods (wholegrain cereals, yoghurt, and other dairy desserts) that are not harmful but protective against the risk of T2DM.22 One of the criticisms of the global view of ultra-processed foods is that energy-dense foods high in hydrogenated fats and simple sugars are classified in the same way as foods high in fibre and micronutrients, which are not only not harmful but are healthy, and therefore avoidance may be counterproductive and contribute to poor nutrition, especially in food-insecure populations.19,21
Food processing is becoming increasingly widespread and there are processes that preserve its nutritional value and others that promote its deterioration and the production of harmful products. It is therefore advisable to choose fresh or frozen foods that have undergone minimal processing and to avoid eating foods that have undergone high temperatures, especially processed meat products. Furthermore, it is not advisable to consume foods containing salt, nitrates, added fats and/or sugars, as there is a high risk that the added fats are partially hydrogenated and rich in TFAs. It is therefore advisable to avoid ultra-processed foods and instead encourage the consumption of fresh, unprocessed, or minimally processed foods.
Levels of evidence on processed and ultra-processed food consumption and cardiovascular risk
| Evidence | Level |
|---|---|
| • Processing causes foods to lose beneficial nutrients, especially when they have been subjected to high temperatures | Strong evidence |
| • Frequent intake of ultra-processed foods promotes all-cause mortality and the development of cardiometabolic risk factors, CVD, and T2DM | Moderate evidence |
| • Ultra-processed foods should be avoided where possible and consumption of fresh, unprocessed, or minimally processed foods should be promoted instead | Moderate evidence |
In recent decades, dietary pattern analysis has emerged as the most accurate way to study the relationship between diet and health. This type of analysis assesses the effect of the diet as a whole, rather than examining the role of individual nutrients or foods. By encompassing all foods and beverages and their nutrient components, with possible synergies and antagonisms between them, dietary patterns are better suited to studying associations between diet and health or disease.228,229 Research on dietary components and patterns that may influence cardiovascular prevention and the underlying mechanisms has grown exponentially in this quarter of the 21 st century; for example, until the end of 1999 there were 357 entries on the Mediterranean diet in PubMed, and from that date to the present there are 11,314 entries (1,320 in 2023 alone). Furthermore, there is an abundance of epidemiological studies using diet quality indices to determine whether adherence to certain dietary patterns (e.g., the Mediterranean diet) or adherence to current dietary guidelines is associated with a lower risk of disease or premature death.
There are many personal and cultural factors involved in the dietary patterns of each individual. However, populations living in the same cultural and geographical environment are influenced by circumstances that homogenise their resources and food preferences, with the result that different geographical environments have shaped a fairly common traditional dietary pattern, although this is currently being challenged by the increasing availability of natural or processed foods from any remote part of the world, which are changing traditional consumption patterns towards a diet richer in processed, ready-to-eat products. Below we will briefly review some of the main dietary patterns defined in the Western world. We will not discuss the dietary patterns prevalent in parts of Asia such as India, Japan, Thailand, etc. due to their low prevalence in our environment, etc.
Mediterranean dietIn our environment, the predominant geographical and cultural dietary pattern is the Mediterranean diet, a plant-based diet that includes plenty of vegetables, fruits, legumes and nuts; olive oil as the main cooking fat; fish and seafood; fat-free poultry and fermented dairy products (yoghurt and cheese); wine in moderation during meals; and low consumption of red and processed meats, processed foods in general, sweets and sugary drinks.230 This is the most studied and best known dietary pattern in the world. Until relatively recently, this was the traditional diet in Mediterranean countries, but adherence in this geographical area analysed over the last 10 years has been low or moderate, regardless of gender or age, indicating a progressive loss of the Mediterranean diet in adults231 as well as in children and adolescents.232 It is clear that there is currently ample room for improvement in the Mediterranean diet in our country.
There is consistent evidence of the health benefits of this dietary pattern, in particular for its association with reduced incidence of CVD and T2DM and their risk factors, reduced cardiovascular mortality, and incidence of cancer and neurodegenerative diseases, and improved cognitive function, with a wealth of data derived from prospective studies31 and their meta-analyses,233,234 apart from those provided by the two flagship RCTs conducted in Spain, the PREDIMED5 and CORDIOPREV6 studies, the results of which are summarised below. The umbrella review by Dinu et al.233 provides a quantitative synthesis of 19 meta-analyses of RCTs conducted to assess the effects of the Mediterranean diet on intermediate factors and concludes, with a low level of evidence, that this dietary pattern may be more effective than a control diet in reducing body weight and adiposity, lowering total cholesterol and raising HDL-C, improving glycaemic control and reducing inflammation, but lacks measurable effects on BP and LDL-C.
The cardiovascular benefits of greater adherence to the Mediterranean diet tend to be more pronounced in cohort studies compared with other diets or healthy foods. For example, in the recent meta-analysis by Rosato et al.234 of 29 observational studies, comparisons of higher versus lower adherence to the Mediterranean diet showed an RR: .81, 95% CI .74–.88 for total CVD, .70, 95% CI .62–.80 for CHD, and .73, 95% CI .59–.91 for CVA. In other meta-analyses of prospective studies, greater adherence to the Mediterranean diet was associated with a 17% (95% CI, 10%–23%) reduction in risk of T2DM235 and each 2-point increase in a Mediterranean diet score was associated with a 10% (95% CI, 9%–11%) reduction in total mortality, with a stronger beneficial effect, i.e., greater longevity, in Mediterranean countries.236
The Mediterranean diet has been studied in 2 large RCTs focussing on CVD, all conducted in Spain. The first, PREDIMED, conducted in almost 7,500 participants with elevated CVR but in primary prevention, showed that a Mediterranean diet supplemented with EVOO or nuts, compared with the recommendation to limit all dietary fat, reduced the incidence of CVD by 30% after almost 5 years of follow-up.5 The recognition of the high quality of the evidence provided by the PREDIMED study has been translated into recommendations by various scientific societies, such as the AHA,3 the AHA together with the American Stroke Association,237 and the European Society of Cardiology (ESC),238 which consider the Mediterranean diet to be the first effective dietary model for cardiovascular prevention and promotion of brain health, although it is recognised that it has only a modest effect on intermediate risk factors. The more recent CORDIOPREV RCT, also conducted in Spain, which included 1,002 patients who had suffered an acute myocardial infarction and observed a 28% reduction in the risk of new cardiovascular events with a Mediterranean diet supplemented with EVOO over 7 years compared with a low-fat diet (HR: .72; 95% CI: .54–.96), is also worth highlighting).6
Precisely because it is a dietary pattern that is well known to us, the Mediterranean diet is the easiest to promote and defend among our population, which makes it easier for health professionals to recommend it. However, its precise definition is not without its difficulties, particularly because of the cultural differences between the various Mediterranean peoples. The most widely accepted definition was proposed by Walter Willett, together with his colleagues from Harvard University and renowned Greek nutritional epidemiologists, who in 1995 had the good sense to present the diet in the form of a pyramid, with the healthiest foods at the bottom and the most probably harmful foods at the top, which is a practical and understandable way to disseminate it.239 A group of nutrition researchers from Mediterranean countries reinterpreted the original Mediterranean dietary pyramid by adding Mediterranean lifestyle components, such as biodiversity and sustainability of the food consumed, culinary activities, regular physical activity, adequate rest, conviviality, and commensality (eating together with family or friends).230 (Fig. 2)
DASH dietThe Dietary Approaches to Stop Hypertension (DASH) diet, described almost 3 decades ago,240 is a dietary pattern that promotes the intake of fruits, vegetables, legumes, whole grains, and nuts in combination with a reduction in SFA-rich foods such as whole meats and dairy products, sweets, and sugary drinks. This dietary pattern, which is low in salt and high in complex carbohydrates, has been shown to be particularly helpful in controlling blood pressure. A DASH diet with additional salt restriction improved its antihypertensive effect.241
A meta-analysis of 30 RCTs showed that a DASH-type diet reduced systolic and diastolic BP, with a greater antihypertensive effect in participants with sodium intake >2,400 mg/day than in those with lower sodium intake.242 The combination of the DASH diet and low sodium intake results in greater reductions in systolic and diastolic blood pressure (–8.9/–4.5 mmHg), than either dietary intervention alone.243 The DASH diet is also effective on other cardiometabolic risk factors, with significant reductions in body weight (–1.59 kg), body mass index (–.64 kg/m2), total cholesterol (–5.12 mg/dl) and LDL-C (–3.53 mg/dl), but no effect on HDL-C, triglycerides, or blood glucose.244
As expected from its effects on risk factors, the DASH diet has also been associated with a reduction in chronic diseases. A meta-analysis of prospective studies suggests that this dietary pattern is associated with a significant reduction of about 20% in CVD, T2DM, cancer, neurodegenerative diseases, and all-cause mortality.245 Data from a large prospective Swedish study with a mean follow-up of 22 years suggest that the DASH diet is associated with a lower risk of heart failure, with an RR: .83, 95% CI: .78–.89, for the top quintile of adherence compared with the bottom quintile.246 In contrast, in a follow-up cohort of individuals with a history of acute myocardial infarction, increased adherence to the DASH diet was not associated with a reduction in cardiovascular and total mortality247; the authors argue that the increased use of antihypertensive drugs by patients in secondary prevention may have played a role in the lack of favourable dietary results.
Dietary and lifestyle guidelines to optimise control of HTN and improve cardiovascular health recommend both the low-sodium DASH diet and the Mediterranean diet, with similar levels of evidence.11 The AHA also recommends the DASH diet, along with the Mediterranean and vegetarian diets, for cardiovascular prevention because of their beneficial effects on risk factors and CVD incidence.3
Vegetarian dietsVegetarian diets, based on a diet without animal products, are becoming increasingly popular for personal, ideological, and cultural reasons, as well as for their sustainability and lower carbon footprint. This dietary pattern includes different models, from the vegan diet, which completely restricts animal products, to the lacto-ovo-vegetarian or pesco-vegetarian diets, which allow the consumption of the foods that give them their name. Vegetarian diets have a higher fibre intake than conventional diets, but there are limitations, especially in the strictest diets. The main limitation is the risk of vitamin B12 deficiency, which is found in meat, fish, and dairy products, and therefore people on these diets need to take regular supplements. Zinc and iron may also be deficient and should be supplemented in children and pregnant women on strict diets.248
Adhering to a vegetarian diet based on minimally processed plant foods has been associated with reduced cardiometabolic risk factors and reduced risk of developing several chronic diseases, including HTN, CVD, T2DM, cancer, and dementia.248 In a recent meta-analysis of 20 RCTs, vegetarian diets improved cardiometabolic risk in participants with high CVR compared with omnivorous diets, with significant reductions in body weight, LDL-C, and HbA1c, but not systolic BP.249 In terms of lipid profile, a recent meta-analysis of 30 RCTs concluded that vegetarian diets reduced total cholesterol, LDL-C, and apoB by an average of 13, 12, and 13 mg/dl, respectively, compared with omnivorous diets.250
A meta-analysis of prospective studies suggests, although with a low level of evidence, that the vegetarian/vegan diet is protective for CHD mortality, but not for cerebrovascular and all-cause mortality.251 Another recent meta-analysis of 13 cohort studies with almost 850,000 participants concludes that a vegetarian diet is associated with a lower risk of total CVD (RR: .85, 95% CI: .79–.92) and CHD (RR: .79, 95% CI: .71–.88), but not CVA.252
It is of utmost importance to define which vegetarian dietary patterns confer better health outcomes and which components are detrimental. In contrast to natural, fresh, and seasonal plant foods, there has been an increase in recent years in the industrial processing of ultra-processed plant products that may contain simple sugars and hydrogenated fats (confectionery, sweets, sugary drinks, vegetables preserved in brine, tropical oils, etc.), the health effects of which are opposite to those of traditional vegetarian diets.248 The AHA recommends the minimally processed vegetarian diet alongside the DASH and Mediterranean diets to achieve the nutritional goals of reducing CVR.3
MIND dietJust over a decade ago, a group of nutrition and dementia experts evaluated the effects of diet as a preventive measure for age-related cognitive decline and developed a dietary scoring system based on the Mediterranean and DASH diets, which they called the Mediterranean-DASH Diet Intervention for Neurodegenerative Delay (MIND).253 The components of the MIND diet include 10 healthy food groups (green leafy vegetables, other vegetables, nuts, berries, whole grains, fish, seafood, poultry, olive oil, and wine) and 5 food groups considered unhealthy (red meat, butter/margarine, cheese, pastries/sweets, and fast food). In fact, the only major difference between the MIND diet and the Mediterranean diet is that the MIND diet favours the consumption of green leafy vegetables, such as lettuce and spinach, and berries or forest fruits, such as strawberries and blueberries.
In the initial study, greater adherence to the MIND diet was associated with improved age-related cognitive decline.253 A systematic review of different types of studies, mainly cross-sectional epidemiological studies, shows that the MIND diet is associated with improved cardiometabolic profile, such as waist circumference, blood pressure, glycaemic control, lipid profile, and inflammation, but the effects on CVD incidence were inconclusive.254 Data from a large prospective North American cohort support the MIND diet as a strategy to reduce cardiometabolic risk in both primary prevention and in patients with established atherosclerotic cardiovascular disease.255 Recent evidence is conflicting regarding the intended purpose of the MIND diet. In a recent meta-analysis of 11 prospective cohorts with almost 225,000 participants and more than 5,200 incident cases of dementia, the highest tertile of the MIND diet score was associated with lower risk of dementia, with a pooled HR of .83 (95% CI .76–.90).256 However, an RCT that recruited 604 healthy individuals with a mean age of 70 years, but who were overweight, had a suboptimal diet and a family history of dementia, and assigned them to 2 discrete calorie-reduced dietary intervention groups, one to the MIND diet and one to a control diet, for 3 years, observed no change in cognitive function or brain structure as assessed by MRI in a sub-sample of participants.257 Therefore, there is a lack of high-level evidence on the effectiveness of the MIND diet in slowing cognitive decline.
The Nordic DietThe Nordic Diet is a dietary pattern that emphasises local, seasonal, organic, and sustainably grown food sources in the Nordic countries and limits processed foods, red meat, and refined sugars. Staple foods include whole grains (especially rye, barley, and oats), fruit (especially berries), root vegetables (such as beets, carrots, and turnips), fatty fish (such as salmon, tuna, and mackerel), legumes, and low-fat dairy products. It includes a wide range of local and wild foods such as seaweed, mosses, fresh herbs, or berries that are particularly rich in antioxidants, such as cranberries, rather than citrus or tropical fruits that are not native to their environment.258
The concept of the Nordic Diet is nothing more than a rediscovery of the traditional diet of the Nordic countries, which was considered healthy because of its richness in plant products and oily fish, and associated with greater environmental sustainability. The contribution of diet to global warming depends on both the production and processing of food and its transport, making local foods the most appropriate. In prospective cohort studies, greater adherence to the Nordic diet has been associated with a reduced risk of CVD, T2DM,259 and CHD.260
Other healthy eating patternsIn recent years, certain dietary patterns have become more popular, with less scientific evidence than those discussed above, but with some interest from the point of view of cardiovascular protection. The Atlantic diet is confined to certain regions of Spain (specifically Galicia, Cantabria, and the Basque Country) and northern Portugal, and more widely to French Brittany and some areas of the United Kingdom, which constitute the current great natural reserve of the Atlantic. This model emphasises the high consumption of fish (sea and river), shellfish (molluscs and crustaceans), vegetables, dairy products, and whole grains. In contrast to the Mediterranean diet, it is characterised by a higher consumption of meat and fish, and a lower consumption of EVOO and nuts. In 2010, the first evidence of the benefits of the Atlantic diet was published, showing that it was inversely associated with the incidence of non-fatal myocardial infarction.261 Similarly, in a recent study involving 4 cohorts and 35,917 participants from southern, central, eastern and western European countries, the Atlantic diet was associated with lower all-cause, cardiovascular and cancer mortality.262 Therefore, with the necessary caution, it is a dietary pattern that could be recommended in these geographical areas.
Another interesting dietary model that has emerged in recent years is time-restricted dieting, popularly known as "intermittent dieting". In this context, intermittent fasting has been developed as a less demanding alternative to continuous fasting for weight loss.263 These diets involve alternating periods of fasting or restrictive fasting with periods of normal eating, allowing you to eat what you want. They can be classified according to whether the reference period is the week, fasting every other day; fasting for 2 consecutive or non-consecutive days with normal eating for the remaining 5 days (the 5:2 diet); or a very low-calorie diet for 5 days followed by periods of at least 10 days without restriction. In the second type of intermittent fasting, the reference period is the day, and food is eaten only during a specific period of the day (usually 8 or 10 h). After 8−12 hours of fasting, the liver begins to break down fatty acids to produce ketone bodies, which the body uses as an alternative energy source to glucose to maintain the function of vital organs. Because of the risk of hypoglycaemia, intermittent fasting can be dangerous for people with diabetes. Current evidence suggests that intermittent fasting is no more effective than conventional calorie restriction for weight loss, although it has been shown to have a cardiometabolic benefit on certain intermediate markers, which reverses on resumption of a normal diet.264 In any case, there is a lack of clinical evidence from RCTs to confirm its long-term benefits.
Levels of evidence on healthy diet and cardiovascular risk
| Evidence | Level |
|---|---|
| • The Mediterranean diet reduces the incidence of CVD (AMI and CVA) and T2DM | Strong evidence |
| • The DASH diet reduces blood pressure, LDL-C, and CVD incidence | Moderate evidence |
| • A vegetarian diet improves cardiometabolic risk and is associated with lower CHD mortality | Moderate evidence |
| • The MIND diet improves cardiometabolic risk and is associated with reduced risk of dementia | Weak evidence |
| • The Nordic diet is associated with reduced risk of CVD and T2DM | Moderate evidence |
Healthy dietary patterns are plant-based, low in SFAs, cholesterol, sodium, and simple sugars, and high in fibre, non-sodium minerals, and unsaturated fats. The various healthy diets reviewed have many components in common, such as the Mediterranean, DASH, MIND, and vegetarian diets, which emphasise the consumption of fruits, vegetables, whole grains, legumes, and nuts, with fish (except in most vegetarian diets) and a reduction in full-fat dairy products and meat. Consistent evidence of health benefits from numerous prospective studies and from the two flagship RCTs on cardiovascular prevention, PREDIMED5 and CORDIOPREV,6 make the Mediterranean diet the basis for the prevention and treatment of CVD in Mediterranean cultures.
Precision and personalised nutrition in the 21 st centuryIt is well known that the response of CVR factors, or CVD risk per se, to dietary changes can vary widely between individuals, due to interactions between their phenotype, genotype, physiology, and gut microbiota, as well as other lifestyle variables, behaviours, socioeconomic status, and environmental exposures. This has led to the emerging concept of "precision nutrition", which has seen significant advances in scientific understanding over the last decade and aims to develop dietary recommendations tailored to the specific biological characteristics and circumstances of each individual.24,265,266 The concept of precision nutrition partly overlaps with that of "personalised nutrition", which is based on similar premises and proposes that individualised nutritional recommendations (tailored to each person) will be more effective in reducing the potency of CVR factors and disease risk than generic dietary advice.267
Precision nutrition relies on both nutrigenetics (the study of the influence of genetic variability on dietary response) and nutrigenomics (the study of the influence of diet on gene expression). The knowledge that the human genome is sensitive to the nutritional environment, which modifies it through epigenomic, transcriptomic, proteomic, and metabolomic processes, is highly relevant to precision nutrition, but its development requires complex and poorly available high-throughput "omics" techniques.268 On the other hand, nutrigenetics deals with genetic polymorphisms by identifying single nucleotide variants (SNPs), for which genome-wide association studies (GWAs) have been an important advance in identifying new variants of potential interest for CVD expression. A recent publication contains a list of 16 SNPs with a relatively high frequency in the population, their adverse health effects, the recommended dietary intervention to limit them, and very useful dietary instructions for carriers.25 This is practical personalised medicine; there are known deleterious SNPs both in general medicine, such as TBI-CC, associated with lactate deficiency, and in the cardiovascular setting, APOE4 being the best example. Other genetic markers, such as DNA copy number variations or endogenous microRNAs,269–271 whose expression can be modulated by diet and which may have a variable influence on cardiometabolic alterations, are being incorporated into this scenario. Another area of interest that has also seen significant development in recent years is nutritional epigenetics, which may help to explain the non-gene sequence-dependent mechanisms by which nutrients and other environmental factors help to modulate gene expression and disease development. In this way, a personalised dietary model could delay or even reverse these epigenetic changes and thus modify the expression of disease.272 Several studies are currently underway to understand how nutrients regulate gene expression, focusing, among other things, on "omics" analyses which, together with the application of bioinformatics techniques and artificial intelligence, will make it possible to integrate all the necessary information into large mega-databases aimed at designing personalised diets.273
The association between circadian rhythm disorders and CVD may also play a role. Recent studies suggest that internal disruption or desynchronisation of the circadian system may contribute to clinical manifestations such as obesity, dyslipidaemia, HT, T2DM, and CVD. An interesting aspect is that these circadian rhythms are modulated by genetic factors. Thus, studies on polymorphisms in clock genes and their interactions with diet open the door to the development of new therapies based on chrono-nutrition.274 Therefore, the chronobiological characterisation of the individual can also be useful in order to implement an appropriate diet according to the genetic characteristics of each person.
In recent years, the concept of precision nutrition has become particularly relevant in the health field. Several RCTs have been conducted comparing these diets with general dietary recommendations, and their results suggest that dietary habits improve significantly in participants assigned to receive precision nutrition.275 A recent RCT comparing precision diets with general healthy dietary recommendations shows only a small improvement in some CVR factors with the intervention diet over 18 weeks.276 Identifying and promoting the optimal diet and lifestyle for each individual based on their genetic traits may be critical in the prevention and treatment of chronic diseases, especially CVD, but all experts point out that, with the exception of dietary advice to counteract the adverse effects of a few known SNPs, such as APOE4,270 personalised and precision nutrition is still at a very early stage of development and much more scientific evidence is needed before it can be applied on a large scale beyond experimentation.265–267
Dietary Pattern SustainabilityIn recent decades, the impact of the food sector has been highlighted as one of the main causes of global warming, accounting for over 20% of global greenhouse gas production and therefore a key factor in the deterioration of planetary sustainability. In addition, water and land use, food production, processing and transport, and excessive fossil fuel consumption are threatening climate stability. It is estimated that about 80% of this effect is due to the livestock sector, with the production of red meat and meat products being the food-related process that most undermines the planet's natural systems.277–279 In recent years, various movements promoted by organisations such as the EAT-Lancet Commission,26 in line with the objectives of the WHO's 2030 Agenda for Sustainable Development, have highlighted the urgent need to transform the food system by adopting a new model that, in addition to the traditional concept of being healthy for the human population, is also healthy for the planet. In this regard, scientists from around the world, led by Walter Willett of Harvard University, have proposed a "Planetary Health Diet" model intended to preserve the planetary ecosystem and reduce noncommunicable diseases, including CVD.26 This dietary model would be a flexible vegetarian diet based on plant-based foods, with a variety of fruits and vegetables, legumes, whole grains, nuts, and only small amounts of animal protein. This dietary model would limit as much as possible the consumption of red meat and its derivatives, ultra-processed foods, meat or otherwise, and the vast majority of pre-cooked foods that contain products such as added sugars or trans fats, which are a very important source of greenhouse gas production. A simple alternative to start the fight against global warming is to encourage the consumption of seasonal and local foods, avoiding those produced in distant places and transported over long distances. The aim is to avoid around 11 million premature deaths per year and to achieve food security and healthy and sustainable diets across the planet by 2050.280 From a practical point of view, and given the complexity of transferring these recommendations to our environment in a simple and effective way, the diet must be flexible and adaptable to the geographical conditions of each population, their own culinary traditions, and personal preferences.
In our environment, we start from the principles of the Mediterranean diet, mentioned by the EAT-Lancet Commission as a benchmark diet for its health benefits and low environmental impact,26 and which has been hailed as an environmentally friendly dietary pattern for three decades.281 It is worth noting the recent publication of a pyramid of the Mediterranean diet with a focus on sustainability282 and evidence is beginning to emerge of how adherence to this dietary pattern translates into a lower environmental impact, particularly through reduced meat consumption.283,284 In our environment, animal protein sources are still an important part of the usual diet and their reduction is a priority objective of the planetary health diet.26,280,285–287 It has been suggested that in order to address the climate emergency and improve the health of the planet, fish consumption should also be reduced, as it generates significant amounts of greenhouse gases, especially when it comes from trawling, transport from distant oceans in refrigerated ships, and recirculating fish farms.287 However, adapting to a planetary health diet model is not easy. Calculations have recently been made of how much a person spends on food per day, and how much more it would cost to adapt to the planetary health diet, depending on the geographical region. The results vary widely, e.g., in sub-Saharan Africa it would be 70% and in South Asia 65%, while in other areas it would be less costly (North America 4% and Europe/Central Asia 10%).288 The challenge of sustainably producing food for the 9 billion people expected to inhabit the planet by the middle of the century is enormous, with the need to control greenhouse gas emissions, conserve dwindling water supplies, preserve diminishing biodiversity, and end hunger in a world in the throes of climate change.
In short, as health professionals, we are faced with a challenging scenario: on the one hand, we must educate the population about the diet of the future, with a broad base of plant products and a substantial reduction in animal protein; on the other hand, we must promote research that will allow us to scientifically determine the benefits or harms of such a diet and, within its parameters, which model is best suited to each geographical region.
Dietary adherence: tactics for improvementIn 2003, the WHO defined adherence to therapies as "the extent to which a person's behaviour, taking medication, following a diet, and/or executing lifestyle changes, corresponds with agreed recommendations from a health care provider".289
The impact of poor adherence is that it compromises the effectiveness of therapy, resulting in both poor primary or secondary prevention of CVD and increased costs to the healthcare system. It has been shown that adherence tends to decrease over time.289 Therefore, increasing and maintaining adherence is a challenge that needs to be addressed from the outset of interventions to improve cardiovascular health. Given the effectiveness of general dietary changes in reducing the potency of risk factors (BP, blood glucose, LDL-C, triglycerides, markers of inflammation or oxidation, etc.), dietary recommendations and adherence are as important or more important than pharmacological prescriptions. In any case, the beneficial effects of diet on risk factors are very useful in cardiovascular prevention.
In this context, several strategies have been proposed to achieve a high level of dietary adherence, which were described in the SEA 2018 document on lifestyle and cardiovascular prevention.1 In view of the new perspectives presented in the current document (SEA 2024), which propose increasing adherence to prescribed diets, there is a need for benchmarks to assess the degree of adherence to the recommendations.290 To assess adherence in our setting, the Mediterranean diet is established as a dietary pattern, whose cardioprotective effects in the primary and secondary prevention of CVD have been amply demonstrated in two large RCTs carried out in Spain.5,6 Questionnaires with different scores can be used to assess adherence to the Mediterranean diet.291 The most commonly used in our setting is the 14-item Mediterranean Diet Adherence Screener (MEDAS), developed for the PREDIMED study,292 (Table 6) validated in several countries and endorsed by the AHA.293 According to the MEDAS, adherence to the Mediterranean diet is classified into 3 categories: high or very high, with 10 points or more; moderate to fair, with 6–9 points; and low, with 5 points or less out of a possible 14. (Table 6)5,292 Other widely used questionnaires to assess adherence to the Mediterranean diet are that proposed by Trichopoulou et al., with 9 variables294 and that by Panagiotakos et al., with 11 foods assigning 5 possible scores of frequency for each.295 Extent of adherence is particularly relevant for determining the cardiovascular benefit, since in prospective studies the percentage reduction in CVR is higher in individuals with a higher adherence score to the Mediterranean diet, both in primary and secondary prevention296; in the case of the PREDIMED study, the cardiovascular benefit of the Mediterranean diet occurred in the context of a 2-point increase in MEDAS.5
Mediterranean Diet Adherence Score (MEDAS) – PREDIMED study.
| 1. Do you use olive oil as the principal source of fat for cooking?Yes = 1 point |
| 2. How much olive oil do you consume per day (including that used in frying, salads, meals eaten away from home, etc.)?4tbsp or more = 1 point |
| 3. How many servings of vegetables do you consumer per day? (Garnish and side servings =½ serving) a full serving = 200 g2 or more (at least one in salad or raw) = 1 point |
| 4. How many pieces of fruit (including fresh-squeezed juice) do you consume per day?3 or more per day = 1 point |
| 5. How many servings of red meat, hamburgers, or sausages do you consume per day? (serving: 100−150 g)Less than one per day = 1 point |
| 6 How many servings of butter, margarine, or cream do you consumer per day? (Serving: 12 g)Fewer than one per day = 1 point |
| 7. How many carbonated and/or sugar-sweetened beverages do you consume per day?Fewer than one per day = 1 point |
| 8. Do you drink wine? How much do you consumer per week?7 or more glasses per week = 1 point |
| 9. How many servings of legumes do you consume per week? (a plate or serving of 150 g)3 or more per week = 1 point |
| 10. How many servings of fish/seafood do you consumer per week? (plate, piece or serving: 100−150 g of fish or 4−5 pieces or 200 g of seafood)3 or more per week = 1 point |
| 11. How many times to you consume commercial (not homemade) pastry such as cookies, (not homemade) custards, sweets, or cakes per week?Less than 2 per week = 1 point |
| 12. How many times do you consume nuts per week? (serving = 30 g)3 or more times per week = 1 point |
| 13. Do you prefer to each chicken, turkey, or rabbit instead of beef, pork, hamburgers, or sausages?(chicken: a piece or serving of 100−150 g)Yes = 1 point |
| 14. How many times per week do you consume boiled vegetables, pasta, rice, or other dishes with a sauce of tomato, garlic, onion, or leeks sautéed in olive oil (sofrito)?2 or more times per week = 1 point |
To increase adherence to dietary recommendations, the characteristics of the patient, the healthcare professional, and the healthcare system must be taken into account. The 2021 ESC Guidelines for Cardiovascular Prevention propose the following strategies238:
- a)
In patient care, it is well known that the focus of consultation is clinician-patient communication and connection. To improve adherence, it is necessary to:
- •
Focus on the patient.
- •
Listen attentively.
- •
Identify and resolve barriers and difficulties (cultural, ethnic, religious, socioeconomic, etc.) that may make adherence to recommendations difficult.
- •
Set goals together with the patient.
- •
Connect with the person’s story.
- •
Explore emotions.
In some cases, particularly with older patients, a family member or close relative may be involved in the consultation. One aspect to consider is that women have a lower awareness of their specific CVR, and therefore a lower perception of the need for treatment, than men. This fact justifies further efforts to improve awareness, risk assessment and treatment in women.
The following tools are available for obtaining clinical information from the patient:
- 1)
The OARS (Open-ended questions, Affirmation, Reflective listening, and Summarising) principle helps patients to present their perceptions, and clinicians to summarise.
- 2)
The SMART (Specific, Measurable, Achievable, Realistic, Timely) principle may help with setting goals for behavioural change.
- 3)
Tools are also available to facilitate dietary adherence, such as verbal cues, written materials, use of the internet, handheld devices, smartphone apps, and even cookery classes.
- 4)
Health professionals should consider their knowledge of nutrition and ability to communicate it, the opportunity (physical, social, or environmental) and the perceived motivation of the patient to change their behaviour. To address motivation to change, multidisciplinary behavioural approaches that combine the knowledge and skills of different caregivers are recommended. In assessing motivation to change, it is useful to identify the individual's attitude through the stages of behaviour change. To this end, the Prochaska and Diclemente model can be used to identify patients who are less receptive to change and to stimulate research into the causes of low receptivity.297
- 5)
Society can contribute to the reduction of CVD by raising awareness of the benefits of a healthy diet.
It is essential to implement dietary prescription whenever a patient comes to the clinic for risk factor management. Once the patient's CVR has been stratified, it is advisable to assess their level of adherence to a healthy diet using a MEDAS-type questionnaire, (Table 6) to identify aspects of their diet that can be improved and to agree on a modification plan adapted to their needs and preferences.4,296,298 Subsequent consultations should assess compliance with the proposed changes and encourage adherence, emphasising the benefits of the dietary changes on anthropometric parameters (weight, waist circumference) or biochemical parameters (glycaemic profile, lipid profile, etc.), blood pressure, or quality of life in general, leading to a reduction in CVR. Fig. 3 shows the algorithm proposed in the 2019 SEA/SEMEGEN consensus document for the prescription of lifestyle changes in cardiovascular prevention.4
Lack of adherence is one of the main reasons why dietary recommendations fail. The challenge is therefore to increase and maintain adherence and to overcome the difficulties of motivating each patient to change, not only to adopt the appropriate diet, but also to adopt a healthy lifestyle to improve general health and cardiovascular health in particular.
These considerations are aimed at achieving high dietary adherence, as this is associated with a reduction in the potency of CVR factors and a reduction in cardiovascular events, both in the high-risk population, as in the PREDIMED study5,299 and in patients with a history of CVD, as in the CORDIOPREV study.6,300 Of course, beneficial changes require the involvement of healthcare professionals, patients, and the community.
Levels of evidence on adherence to a healthy dietary pattern
| Evidence | Level |
|---|---|
| • High adherence to a healthy diet has a beneficial effect on CV risk factors and CVD reduction, both in the general or high-risk population and in patients with a history of CVD | Strong evidence |
| • A 2-point increase in the MEDAS score is associated with a significant reduction in cardiovascular risk | Strong evidence |
The aim of this document is to provide health professionals with an update of the knowledge on the relationship between diet and CVR, based on the latest available evidence, in order to provide key dietary recommendations on the main food groups and dietary patterns that can be transferred to people receiving advice on cardiovascular prevention.
One aspect considered is the modification of the traditional concept of the basic nutritional unit of the diet from nutrients to foods, integrated into a dietary pattern, which in our setting is the traditional Mediterranean diet, with proven benefits in reducing CVR. Tables 7 and 8 summarise the main dietary recommendations for cardiovascular prevention and the desirable frequency of consumption. Fig. 1A and B illustrate the relationship between the main food groups and dietary patterns and CVR.
Key food consumption recommendations for cardiovascular prevention.
| Edible fats of plant origin |
| - Use extra virgin olive oil in cooking and at the table |
| Fruit and vegetables |
| - Five servings of fruit and vegetables a day (one or more servings can be juices with no added sugar) |
| Tubers |
| - Potatoes as desired, preferably with vegetables or in casseroles |
| Cereals |
| - At least one serving of cereal (bread, rice, or pasta), preferably unrefined |
| Meat |
| - Unprocessed meat up to a maximum of 3 times per week, preferably poultry, lean red and white meat, with visible fat removed before cooking |
| Eggs |
| - Eggs are safe to eat and up to one egg per day can form part of a healthy diet |
| Fish |
| - Fish or seafood, fresh or frozen, at least 3 times a week, 2 portions should be oily fish |
| Dairy products |
| - At least 2 servings a day of dairy products, whole or skimmed, fermented or non-fermented, with no added sugar |
| Nuts |
| - A handful of nuts (equivalent to about 30 g), preferably raw, every day or at least 3 times a week, avoiding salted nuts |
| Cocoa and chocolate |
| - Cocoa or dark chocolate (with at least 50% cocoa content) with no restrictions |
| Coffee and tea |
| - Up to 5 cups of coffee per day (filtered or instant, full, or decaffeinated) or tea in any quantity (green or black), limiting added sugar and artificial sweeteners as much as possible |
| Alcoholic beverages |
| - If a regular drinker, wine in moderation with meals |
| Sugary and sweetened drinks |
| - Avoid drinks with added sugar and artificially sweetened drinks, not only soft drinks but also industrial juices and milk drinks |
| Salt |
| - Reduce salt intake in cooking and at the table, and limit the consumption of processed, canned, cured, salted, sausages, carbonated drinks, and other ultra-processed foods |
| Processed foods |
| - Avoid ultra-processed foods and choose fresh, unprocessed, or minimally processed foods instead |
Desirable frequency in the form and amount of food consumption.
| Consumption frequency | Daily | Maximum 3 times per week | Not recommended or occasional |
|---|---|---|---|
| Edible fats | Virgin olive oil | Spreadable margarine | Frying with seed oils, margarine, or butter |
| Cereals | Bread, preferably wholemeal. Pasta, rice, maize, other | Pastries, cakes, biscuits, etc. | |
| Fruit and vegetables | Five servings combining the different types of fruit and vegetables, including natural juices (no added sugar) | Commercial fruit juicesFruit in syrup | |
| Legumes | Beans, chickpeas, lentils, etc., boiled | Cooked with fats such as chorizo, bacon, etc. | |
| Tubers | Potatoes and sweet potato, cooked with vegetables | Commercial crisps | |
| Nuts and peanuts | Raw or roasted (30 g–45 g) | Salted | |
| Eggs | Whole eggs are not advised against | ||
| Fish and seafooda | Oily or whiteSeafood (crustaceans and molluscs)Preserved naturally or in olive oil | Preserved in vegetable oils | Commercially fried, salted, smoked |
| Meatsb | Poultry and rabbits | Lean red meats | Processed meats, sausages |
| Dairy products | Whole or skimmed milk and yogurt (without sugar).Cheese of any kind | Butter, cream | Cured cheeses in hypertensive patients |
| Chocolate | Dark with ≥70% cocoa | Dark with<70% cocoa | Milk and white chocolate |
| Coffee and tea | Unlimited tea and coffee up to 5 per day, no sugar or artificial sweeteners | ||
| Sugary drinks or drinks with artificial sweeteners | Avoid | ||
| Alcoholic beverages | Limit to 30 g of alcohol in male drinkers and 15 g in women. Preferably fermented beverages (wine, beer) with meals | Non drinkers | |
| Salt | Between 2.5−4 g per day | Salted foods | |
| Preparation of foodc | Preferably boiled, grilled, or sautéed | Fried in virgin olive oil | Avoid smoked, processed and foods fried with seed oils |
DM: diabetes mellitus.
One of the major limitations in implementing the recommendations of this document is the lack of "nutrition culture" or "nutrition literacy" in our environment. On the one hand, it is crucial to educate health professionals about the impact of nutrition as a tool for the prevention and treatment of CVD and for the maintenance of health in general, in order to improve their ability to make decisions in their routine clinical practice. Healthy eating knowledge should be incorporated into health sciences education so that every health professional can pass it on to patients in clinical practice. Strategies should also be considered to help people make informed choices and adopt healthy diets and responsible and sustainable food habits.