Atherosclerotic cardiovascular disease (ACVD) is the major adverse outcome in the evolution of several metabolic conditions. For around several decades, the cardiovascular continuum has been used as a fantastic tool to explain the evolution of ACVD from the onset of risk factor, to clinical outcomes, and to death. Nowadays, metabolic diseases such as obesity, prediabetes, and type 2 diabetes have been increasing enough to become serious public health problems and notorious contributors to the morbidity and mortality rates due to ACVD, including arterial hypertension. Other conditions seem to increase the list, such as: physical inactivity with its metabolic cluster, sarcopenia, and non-alcoholic fatty liver disease (NAFLD). Moreover, obesity in childhood has been growing at an exponential rate so the excess of adiposity in children and adolescents will translate into an excess of cardiometabolic risk in adults. Several longitudinal studies confirm the strong association of paediatric obesity with the persistence of adult obesity, as well as the future development of cardiometabolic conditions, such as prediabetes, diabetes, obesity, increased risk of arterial hypertension, and ACVD. Therefore, it is time to conceptualise the cardiometabolic continuum as a tool of an early, wider and preventive intervention in order to reduce the morbidity and mortality due to ACVD.
La enfermedad cardiovascular aterosclerótica (ECVA) es el principal desenlace de la evolución en una serie de condiciones metabólicas. Desde hace varias décadas, el continuo cardiovascular es una herramienta extraordinaria para explicar la evolución de la ECVA desde el inicio de los factores de riesgo hasta los desenlaces clínicos y la muerte. Hoy día, enfermedades metabólicas como la obesidad, la prediabetes y la diabetes tipo 2 se han incrementado lo suficiente para transformarse en un serio problema de salud pública y contribuyentes notorias a la tasa de morbimortalidad debido a ECVA, incluyendo la hipertensión arterial. Otras condiciones parecen incrementar la lista, tales como la inactividad física con su pléyade metabólica, la sarcopenia y el hígado graso no alcohólico. Más aún, la obesidad en la infancia y la juventud están creciendo a una velocidad exponencial, de modo que el exceso de adiposidad se traducirá en un exceso de riesgo cardiometabólico en los adultos. Varios estudios longitudinales confirman la estrecha asociación entre la obesidad pediátrica con la persistencia de obesidad en el adulto y el desarrollo futuro de condiciones cardiometabólicas, tales como prediabetes, diabetes, obesidad, mayor riesgo de hipertensión arterial y ECVA. En consecuencia, es el momento de conceptualizar el continuo cardiometabólico como una herramienta de una aplicación preventiva más temprana con la finalidad de reducir la morbimortalidad debido a la ECV.
The concept of the cardiovascular continuum, which emerged at the beginning of the 1990s, is the conclusion of a working group hypothesis that viewed cardiovascular disease (CVD) as a chain of events triggered by numerous related and unrelated risk factors, progressing through various pathophysiological pathways until finally leading to end-stage CVD, where any intervention could slow down the progression of the pathophysiological process.1
In the intervening years, data from experimental and clinical research studies confirmed the underlying pathophysiological mechanisms and, with the development of new therapeutic classes and numerous clinical trials of high methodological quality, established the validity of a cardiovascular continuum and reinforced the notion that any intervention, no matter where in the chain, can modify CVD progression. Further evidence indicates that events leading to disease progression overlap and intertwine, with no linear time sequence.2–4
The cardiometabolic continuum as a conceptDrawing largely from epidemiological, observational, and clinical outcome studies, the close link between metabolic conditions such as type 2 diabetes mellitus (DM2) and obesity with atherosclerosis, hypertension and subsequent CVD outcomes was demonstrated. This is a valid argument for considering these conditions, and others, as cardiometabolic, whose progression can also be explained along a cardiometabolic continuum.
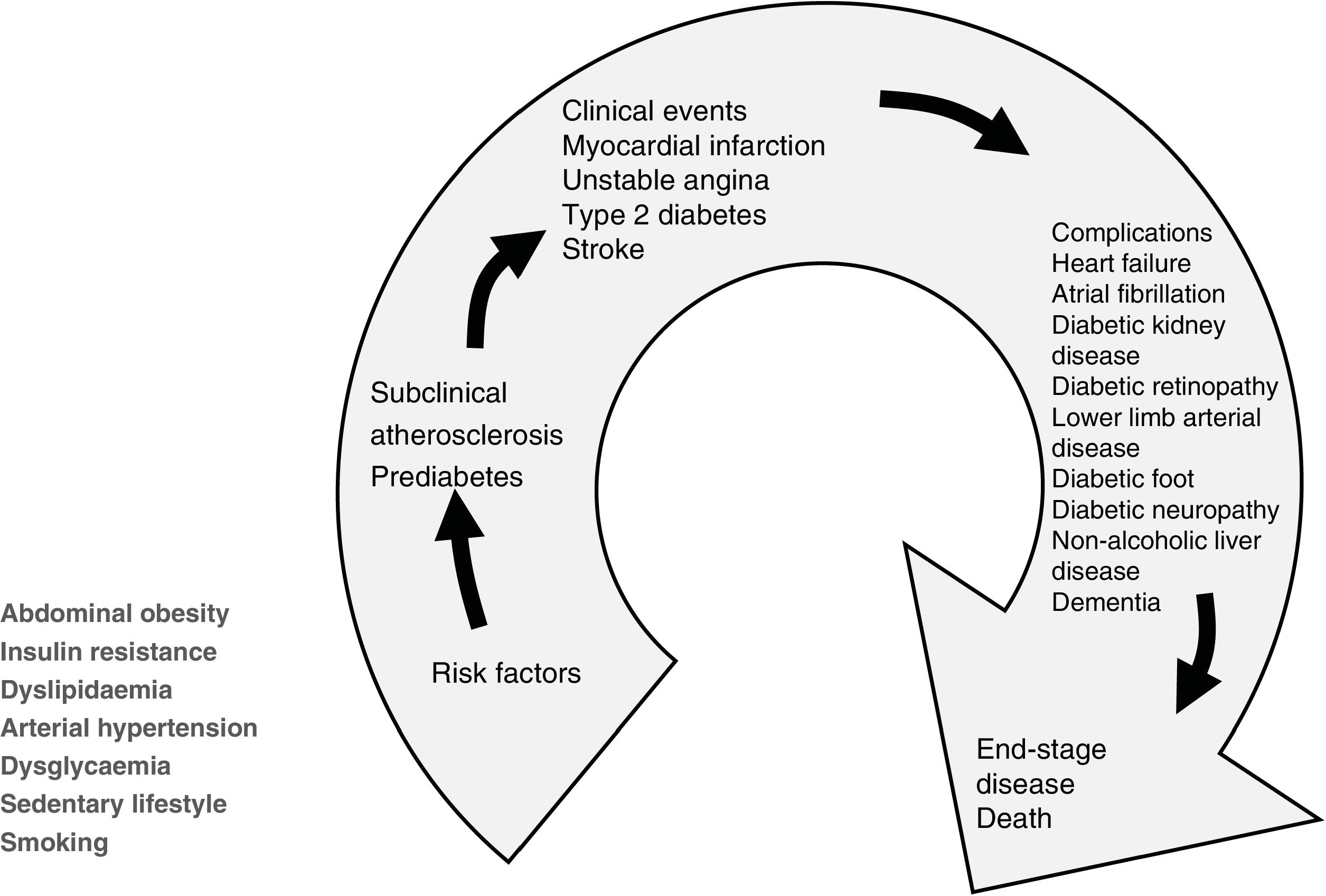
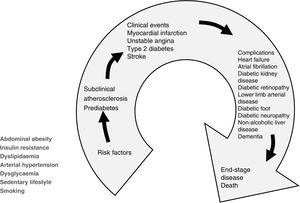
Cardiometabolic patients commonly have more than one cardiovascular risk factor (CVRF), such as dyslipidaemia, high blood pressure, sedentary lifestyle and even smoking. Therefore, the most appropriate preventive approach is through the optics of the cardiometabolic continuum, as shown in Fig. 1, because it reflects the series of concatenated events that cover the transition from the onset of cardiovascular risk factors, including metabolic CVRFs, to the development of a clinical condition, cardiovascular, metabolic or both, with the possible inclusion of further disease in the course of progression to the final outcome.
The cardiometabolic continuum. In addition to cardiovascular risk factors, several metabolic conditions of particular impact on the cardiovascular system and ACVD events, such as insulin resistance, central obesity, dysglycaemia and sedentary lifestyle, which may go unnoticed, must be considered at the beginning of the continuum.
The group of cardiometabolic diseases originally comprised obesity, pre-diabetes and DM2, to which subclinical atherosclerosis, physical inactivity or, worse, a sedentary lifestyle with its array of metabolic disturbances and sarcopenia have recently been added. Non-alcoholic fatty liver disease has also recently been added to the group.
It is not uncommon for several of these conditions, whose pathophysiological substrate is insulin resistance, to coexist, with or without arterial hypertension. This is the fatal combination that fosters progression of atherosclerosis and atherosclerotic cardiovascular disease (ACVD).
It is also of interest to consider that all these conditions foster the development of intellectual impairment and dementia,5,6 an end point that is appearing at younger ages and in greater numbers of people.
Of course, as in the cardiovascular continuum, any intervention, positive or negative on the cardiometabolic continuum, would change the progression and outcomes of ACVD in one way or another.
We briefly consider these entities separately and how they fit into the cardiometabolic continuum.
General obesityA positive energy balance between and calorie intake and energy expenditure results in weight gain and obesity, in which several genetic, epigenetic, and environmental factors have been implicated. In most cases no single factor is exclusively responsible and in fact obesity is the sum total of the interaction of these factors and may vary over time according to the subject’s individual characteristics.7
One of the main arguments validating the cardiometabolic continuum is the irrepressibly increasing prevalence of obesity, as summarised below8–11:
- •
Obesity tripled worldwide between 1975 and 2016.
- •
In 2016, more than 1.9 billion adults aged 18 and over were overweight, of whom more than 650 million were obese.
- •
By that year, 39% of adults aged 18 years and over (39% of men and 40% of women) were overweight.
- •
Projections drawn from 182 epidemiological and demographic surveys with 2,240,000 responses indicate that, if past trends continue, the number of poor and overweight people will increase by, on average, 84.4% (range 3.54%–383.4%), most notably in low-income countries.10
- •
In projections for 2030 in the United States,11 nearly one in two adults will be obese (48.9%; 95% confidence interval [CI 95%]: 47.7–50.1). This proportion will be higher in 29 states, but no state will be below 35%. By that year, nearly one in four Americans will be severely obese.
The figures are more worrying in children12:
- •
The proportion of overweight children under 5 years of age increased 20% between the years 2000–2018; the latter year saw a proportion of 1 in 17 weighing more than the global standard.
- •
The Region of the Americas is considered by the WHO to have the highest proportion of overweight children: 1 in 14.
- •
In terms of economic status, the proportion is highest in high- and middle-income countries (1 in 14) and lowest in lower income countries (1 in 32).
In relation to children and adolescents (aged 5–19 years)8,13,14:
- •
Estimated overweight or obese population for 2016: 340 million.
- •
Prevalence in this age group is nearing a five-fold increase: from 4% in 1975 to more than 18% in 2016. Increase observed in both sexes: 18% of girls and 19% of boys.
- •
Whereas in 1975 fewer than 1% of children and adolescents aged 5–19 years were obese, in 2016 there were 124 million (6% of girls and 8% of boys).
- •
Although the prevalence of obesity in children was lower than in adults, childhood obesity, in many countries, is increasing at a faster rate than that observed in adults.14
The burden of disease in the population is a point to consider. The GBD 2015 Obesity Collaborators report,14 conducted on more than 68.5 million people to assess the trends in the prevalence of overweight and obesity in children and adults between 1980 and 2015, found that excess body weight accounted for almost 4 million deaths and 120 million years of life lost to disability. Almost 70% of deaths from high body mass index (BMI) were due to CVD and more than 60% of these deaths occurred in obese subjects. Another interesting conclusion of the report is that the balance of evidence shows that a BMI between 20 and 25 constitutes the minimum level of disease risk.
Furthermore, obesity and consequent insulin resistance are determinants for the onset of DM2, progression of atherosclerosis and target organ damage, with the early vascular damage that is evident in many patients.15
Abdominal obesity in the cardiometabolic contextWhile general obesity is estimated by BMI (kg/m2), central or abdominal obesity is the best reference for alterations in the cardiometabolic continuum, with abdominal circumference being a valid marker of this ectopic accumulation of intra-abdominal fat in humans.16
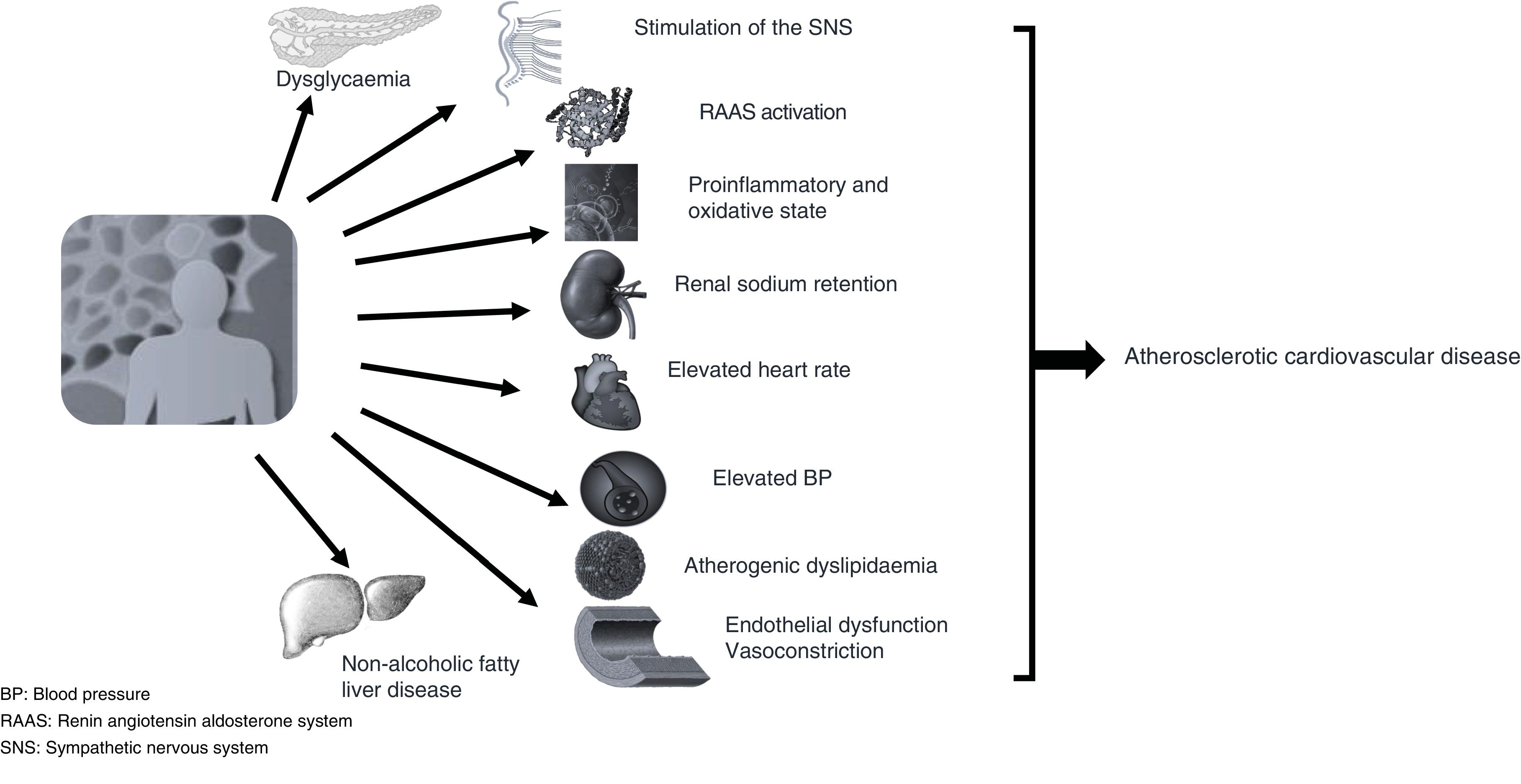
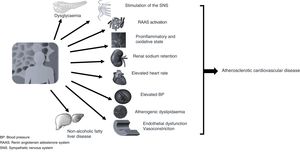
Abdominal adipose tissue usually coexists with insulin resistance and one or more of the CVRFs or other pathophysiological conditions, such as adrenergic or renin angiotensin aldosterone system hyperactivity and even an inflammatory microenvironment typical of the adipocyte, all of which contribute to altering cardiovascular homeostasis by encouraging increased blood pressure, resting heart rate and endothelial dysfunction, which will help drive the development of atherosclerotic lesions (Fig. 2), thereby favouring the development of cardiovascular complications such as left ventricular hypertrophy, atrial fibrillation, acute coronary syndrome, heart failure and thromboembolic disease.17
As with general obesity, the prevalence of abdominal obesity is alarming. In the recent meta-analysis by Wong et al.,18 comprising 288 studies involving 13,233,675 subjects over the age of 15 years, the overall prevalence was 41.5% (CI 95%: 39.9–43.2), with the following characteristics:
- •
The highest prevalence was found in the elderly, in women, in urban residents, in Caucasians and in populations from higher income countries.
- •
In terms of regional variations, the highest prevalence was found in South America (55.1%; CI 95%: 45.8–64.3) and Central America (52%; CI 95% 32.7–72.7).
- •
There was a rapid growth between 1985 and 2014, with the age group between 15 and 40 years experiencing a greater increase (from 16.3% to 33.9%) than subjects over the age of 40 years (43.6%–57.9%). This trend with a doubling in percentages will translate into a higher cardiometabolic risk in the productive segment of the population with serious implications for the burden of ACVD.
- •
In men, the increase was more dramatic (25.3%–41.6%) than in women (38.6%–49.7%).
These data are of great importance for preparing public policies to increase physical activity and improve the quality of nutrition. The same recommendation should be considered for these subjects in the academic curricula of undergraduate and postgraduate medical studies, which are usually neglected.19
On the other hand, this abdominal adiposity accompanies and fosters hyperinsulinaemia and insulin resistance, which can culminate in pre-diabetes and then in DM2, with the well-known entourage of microvascular complications (diabetic renal disease, retinopathy, and neuropathy), some of which may be present at the time of diagnosis of the disease and go unnoticed by the physician.20
Fortunately, being a gradual evolutionary process, some of these cardiometabolic conditions can be reversed or at least slowed in their progression or restricted to subclinical cardiac or arterial damage, which, although difficult to reverse completely, respond well to appropriate therapeutic measures.
Physical inactivityAs with the growth of obesity, inadequate physical activity has become a major cardiometabolic risk factor, especially in children and adolescents. Several WHO reports in recent years have raised concerns about children and adolescents failing to meet physical activity goals.21 The recent publication by Guthold et al.22 on insufficient physical activity among adolescents analyses data from 1.6 million students aged 11–17 years and shows that, overall, in 2016 81.0% (uncertainty interval [II] 77.8–87.7) of participants were not active enough, with a lower percentage among males (77.6% [76.1–80.4]) than females (84.7% [83.0–88.2]). Moreover, the prevalence of insufficient physical activity declined significantly between 2001 and 2016 for males (from 80.1% to 77.6%), but not for females (85%.1–84.7%), regardless of the countries’ economic status.
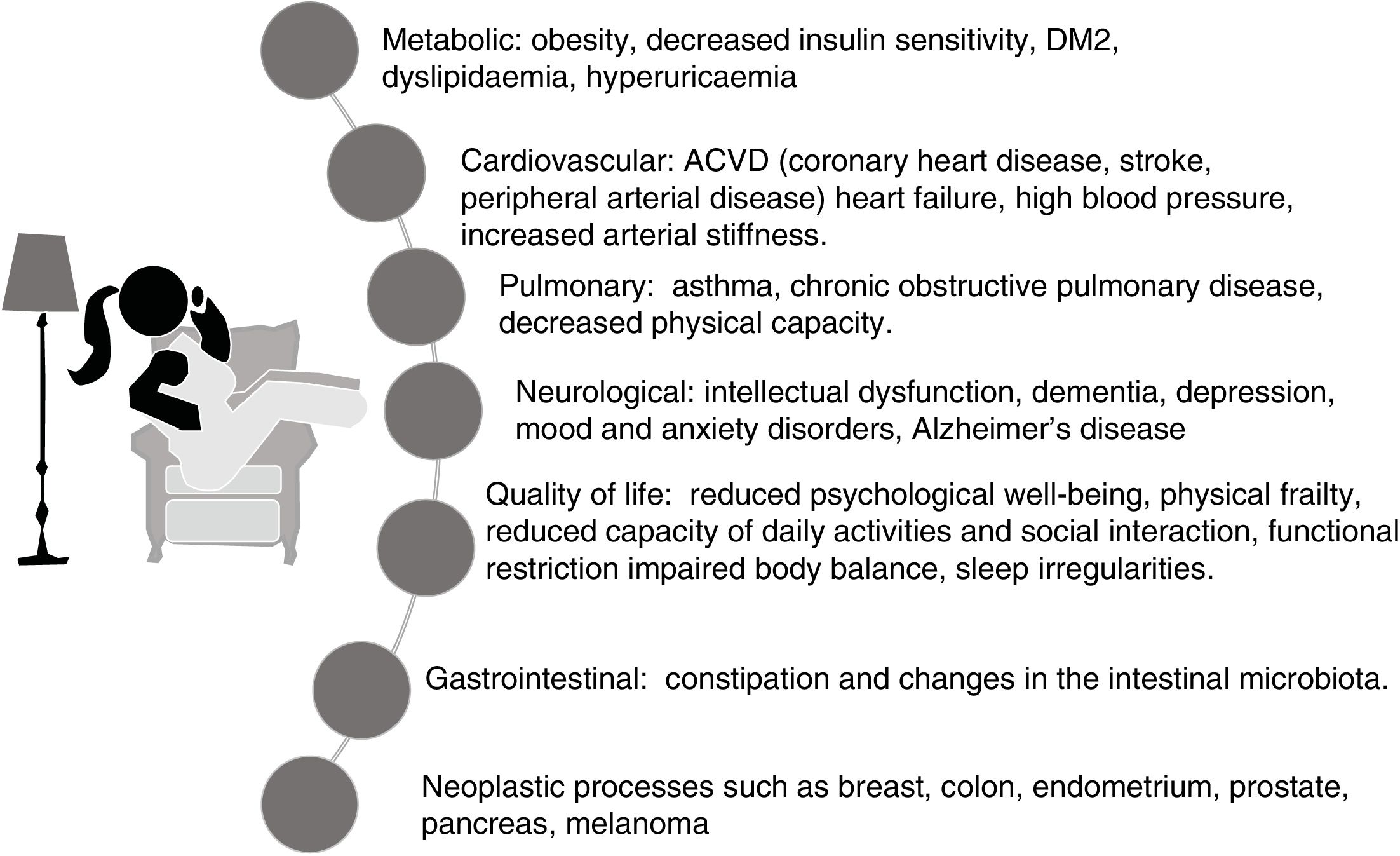
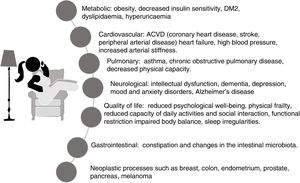
The harmful effects of sedentary lifestyles, a behaviour that has become an aspect of contemporary lifestyles and certainly not well publicised, involve almost all structures or systems of the body,23–27 and in most cases dependent on each other. These are summarised in Fig. 3.
Prediabetes and subclinical atherosclerosisIt is well known that DM2 is preceded by a prolonged asymptomatic stage, characterised by hyperglycaemia (between 100 to 125 mg/ml), insulin resistance and early reduction in insulin secretion capacity, and may coexist with dyslipidaemia and elevated blood pressure.28,29
According to the American Diabetes Association (ADA)28 and European guidelines,29 any of the following three defining criteria are appropriate:
- •
Fasting blood glucose between 100 mg/dl (5.6 mmol/l) to 125 mg/dl (6.9 mmol/l), a condition referred to as impaired fasting blood glucose, or
- •
Glucose tolerance test: 2 h with a 75 g glucose load, 140 mg/dl (7.8 mmol/l) to 199 mg/dl (11.0 mmol/l), a condition called abnormal glucose tolerance, or
- •
Glycosylated haemoglobin (A1c) between 5.7% to 6.4% (39–47 mmol/mol).
It is important to clarify that the risk is continuous, extending below the lower end of the range and becoming disproportionately higher at the upper ends of the range.
Prediabetes should not be labelled as a clinical entity, but rather as a condition of increased risk that is of some significance due to its connotations28–32:
- •
Its high prevalence: it may exist in one in three adults, and in about half of those over 65 years of age. In the young US population, one in five adolescents and one in four young adults have pre-diabetes.
- •
Without changes in lifestyle, one third of people with pre-diabetes may develop DM2 within 5 years.
- •
It implies an increased risk of ACVD, with rapid progression of atherosclerosis.
- •
A substantial percentage of patients already have impaired vision, impaired renal function, impaired sensation and/or impaired blood supply to the lower limbs, all expressions of microvascular damage31 that usually go unnoticed or are not given due attention.
- •
The coexistence of other conditions such as obstructive sleep apnoea syndrome, hepatic steatosis or non-alcoholic fatty liver disease, intellectual impairment or periodontal disease is not uncommon in these patients.33
Effective preventive treatment can eliminate or delay the onset of DM2, with lifestyle changes such as healthy eating and increased regular and vigorous physical activity to lose 5%–7% of body weight, if necessary.28,29 These lifestyle changes can more than halve the risk of DM2.
Identifying subjects with prediabetes widens the window of opportunity to initiate strategies to reduce the likelihood of the disease and cardiovascular and renal risk; the earlier and more effective the better. On this aspect, the notorious increase in the prevalence of prediabetes among adolescents (12–18 years) needs to be highlighted, reaching 18.0% (CI 95%: 16.0–20.1), and 24.0% (CI 95%: 22.0–26.1) in young adults (19–34 years), which constitutes a ratio of one in five adolescents and one in four young adults.32 Moreover, compared to their peers without prediabetes, they showed higher non-HDL cholesterol levels, systolic blood pressure, abdominal adiposity and lower insulin sensitivity.
Subclinical atherosclerosis is the long silent or asymptomatic period in the natural history of atherosclerotic disease which, although present, has not yet been reflected in a clinical adverse event. Although CVRFs are useful in predicting the likelihood of an outcome in population groups, their accuracy in estimating overall cardiovascular risk in an individual varies considerably and usually underestimates it.34 Therefore, it is not uncommon for an episode of sudden death to be the first clinical manifestation of atherosclerosis. This fact, coupled with the high morbidity and mortality of ACVD, and the evidence that the earlier preventive measures are implemented, the better the outcome, has led to the search for tools or markers for early detection of ACVD in asymptomatic patients.35
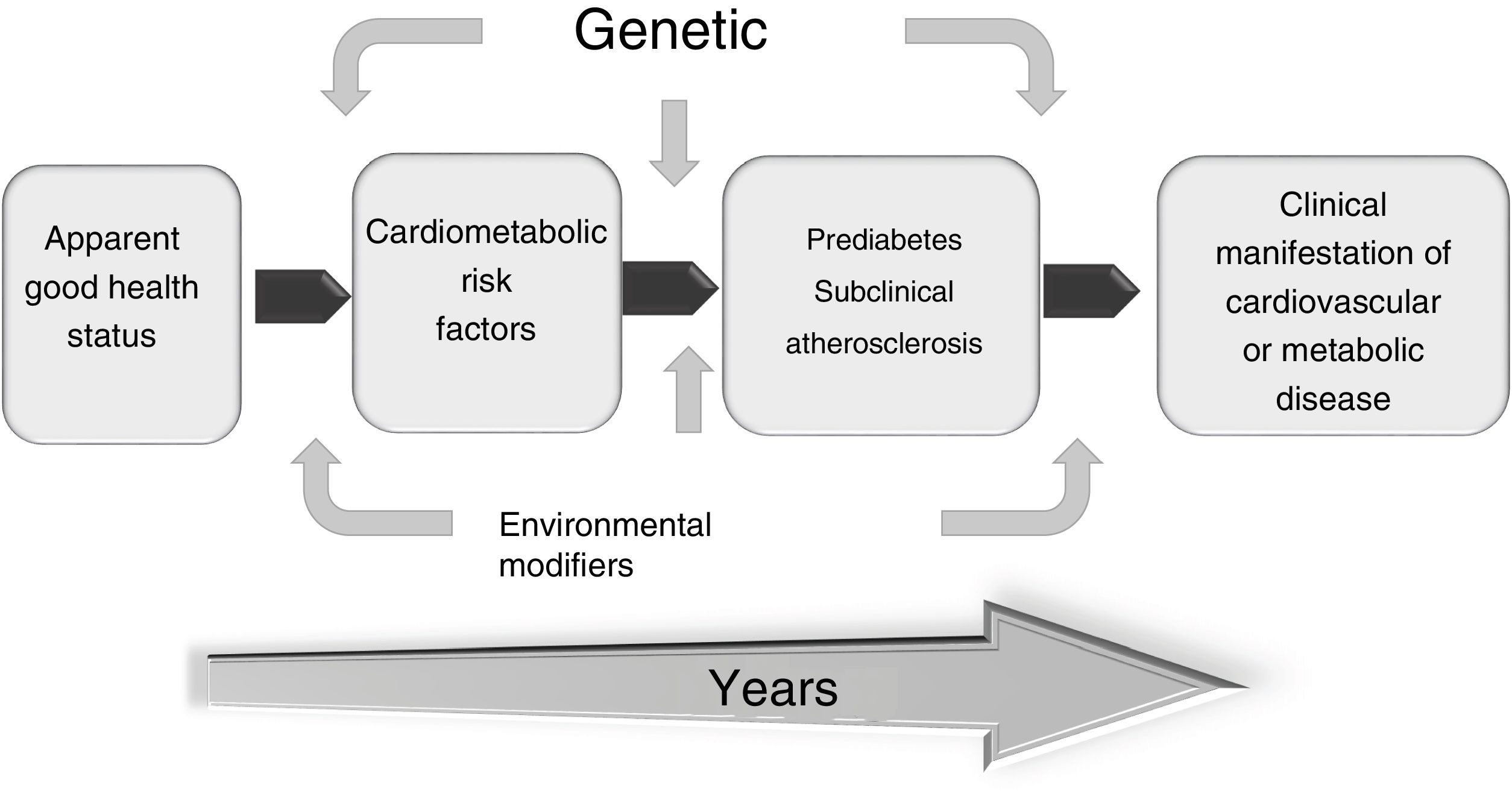
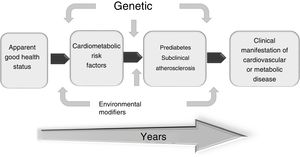
The search for versatile and non-invasive diagnostic procedures has resulted in the development and validation of certain techniques (carotid ultrasound, determination of coronary calcium, ankle-brachial index, etc.) to assess the disease in its early stages to better identify vulnerable patients and implement appropriate treatment. Therefore, intervening in this subclinical phase is crucial to prevent cardiovascular clinical events more effectively (Fig. 4).
In summary, both prediabetes and subclinical atherosclerosis are therapeutic windows that must be exploited to implement effective strategies to minimise or eradicate the potential future impact of ACVD.
Atherogenic dyslipidaemiaAtherogenic dyslipidaemia is of paramount importance among the CVRFs because of the relevance of the lipid triad of low HDL-C, high triglycerides (TG) and a higher proportion of small, dense LDL particles, which give it its greater atherogenic power.36 This lipid triad is emerging in a high proportion of the population of many countries, especially the Latin American subcontinent.
This condition can be reversed by adopting a healthier lifestyle with better quality food, increased physical activity and loss of excess weight. If these measures fail, pharmacological treatment at the necessary dosage should be used. Atherogenic dyslipidaemia is unlikely to disappear despite intensive treatment, the patient should be made aware by the physician that it is only controlled.37
Another recently reported actor is hepatic steatosis, very frequent in subjects with abdominal obesity and/or DM2 and secondary to the increased flux of free fatty acids from lipolysis.38 This fatty liver may function either as a target of existing metabolic abnormalities and/or as an amplifier of atherogenesis through the release of inflammatory, haemostatic, and oxidative stress-promoting components.39
The consequences of cardiometabolic conditions on overall health can be summarised as follows40,41:
- •
Increased risk of concomitant diseases, especially ACVD, as atherosclerosis is ubiquitous. Patients with vascular involvement in one arterial territory usually have atherosclerotic lesions in other arteries.
- •
High frequency of arterial hypertension and arrhythmias, such as atrial fibrillation.
- •
Impact on and damage to target organs: kidney, brain, and liver.
- •
Impaired quality of life, depending on the degree of disability.
- •
High mortality, especially sudden cardiac death, which is the first manifestation of the disease in a high percentage of cases.
The evidence clearly shows that strict adherence to treatment (pharmacological treatment and therapeutic changes in lifestyle habits, especially a heart-healthy diet and daily physical activity routine), reflected in excellent metabolic control (glycaemia, A1c, LDL-C and TG) and blood pressure control, can reduce the probability of a vascular event or progression to DM2 by more than 50%, ensuring a better quality of life.42
DiscussionFrom the abundant documentation on cardiometabolic health from numerous observational, epidemiological, interventional, and clinical studies, the most effective strategy appears to be early detection and treatment of the risk factors that trigger the cardiometabolic continuum as the only way to slow, halt or delay the onset and/or progression of ACVD. Therefore, the emphasis should be on primary prevention (avoiding the occurrence of risk factors) or primary prevention (avoiding the damage caused by risk factors present), with primary care physicians, general practitioners or physicians who do not specialise in the cardiometabolic approach as the bulwark, since most patients with a cardiometabolic disorder first come under their care. Hence the importance of viewing the condition as a continuum, as it is easily assimilated by the doctor and understandable for the patient as a dynamic vision of the problem marked by its progression over time.
Clearly, the cardiometabolic continuum would help us understand the complexity of pathophysiological and clinical disturbances, encourage patient adherence to therapeutic strategies, and avoid possible deviations from the pathway. It is essential is for the physician to understand the pathophysiology of cardiometabolic conditions as a tangle of intertwined mechanisms that, by one route or another, lead to clinical events. Therefore, therapeutic intervention must be more energetic and comprehensive than is generally thought, since it is not a question of a single risk factor, but of several of greater or lesser relevance, which will always contribute to some extent to the progression of this type of condition.
The uncontrolled growing prevalence of overweight and obesity, especially in childhood and adolescence, will surely force a change in the undergraduate medical curricula to include academic preparation in the cardiometabolic area, especially in nutrition, where a deficit in this knowledge has been identified in several published evaluations.19
We must realise that childhood obesity has gone from a rare event to common occurrence, and its repercussions can be traced into adulthood; therefore, we must stop viewing obesity as a matter of numbers. It is essential that it is seen as a complex disease whose negative burden does not disappear completely with weight loss; in fact, children with obesity are five times more likely to remain obese than adults, with all the concomitant cardiometabolic problems.43 Therefore, as the prevalence of childhood obesity increases, a commensurate rise in the future burden of ACVD is to be expected. Thus, public policies aimed at reforming/eliminating the obesogenic environment in children and adolescents are crucial for health in future years and are an excellent investment.
Another important aspect of obesity is deterioration in the quality of health. According to the study by Nyberg et al.,44 mild obesity is associated with a loss of one in 10 years, and severe obesity with a loss of one in four years of potentially disease-free years during young and late adulthood. Moreover, this greater loss of disease-free years as obesity becomes more severe occurs equally in both sexes, in smokers and non-smokers, in the physically active or inactive and across the socio-economic scale.
Regarding physical inactivity, it is clear that sedentary behaviours are an aspect of contemporary lifestyle and show a close relationship with several risk factors, in addition to cardiometabolic risk factors, such as bone health with a tendency to osteopenia or intellectual impairment. Unlike physical activity programmes, which involve investments in time, transport, infrastructure and logistics, a reduction in sedentary behaviour can be achieved at very low economic cost through simple micro-interventions, with no time limit, aimed at further reductions in sedentary lifestyles and introducing activities with higher energy expenditure.
Healthcare professionals, especially in primary care, general practitioners or specialists not trained in the cardiometabolic area, need to fully understand the pathophysiology of these disorders to be able to intervene biologically and behaviourally to ensure adequate therapeutic coverage and to minimise the likelihood of a clinical outcome, which may eventually be fatal.
In recent years, the term “cardiometabolic multimorbidity” has been coined for the coexistence of two or more such entities, such as hypertension, obesity, pre-diabetes, DM2 and ACVD. This has become progressively more common globally, with an extraordinary public health impact due to high mortality, morbidity, and economic cost.45 In these cardiometabolic entities this coexistence is more the rule than the exception.
Applying the cardiometabolic continuum requires the ability to interact with patients in clear and understandable language and to educate them about the benefits of existing approaches, and the risks of non-adherence or using unproven drugs or strategies. Patients must be clearly advised that the goal is not only to control altered blood glucose, lipid, or weight, but also to prevent ACVD, the ultimate fate of these conditions when not treated early and intensively enough.
FundingThis research study received no specific grants for agencies in the public, commercial or non-profit sectors.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank Lic. Pedro M. Arocha Silva for his thorough review and editing of this manuscript and Ana María Reyes for the elaboration of the corresponding images.
Please cite this article as: Arocha Rodulfo JI. Aproximación al continuo cardiometabólico. Descripción narrativa. Clin Investig Arterioscler. 2021;33:158–167.