To determine the prevalence of biliopancreatic reflux (BPR) in patients with biliary pancreatitis (BP) undergoing elective cholecystectomy with intraoperative cholangiography (IOC) in comparison with a control group of symptomatic cholelithiasis (CG).
Patients and methodsRetrospective review of 107 consecutive BP cases. BPR was determined by IOC and liver function tests (LFT) were recorded at admission (A), 48h, and preoperative examination (P). LFT analysis between A and P were analyzed between groups with respect to BPR, time interval to cholecystectomy within the same group and by determination of observed value/maximum normal value ratio (OV/MNV).
ResultsBPR incidence was 38.3% in BP in comparison with 5% in CG (P=.0001) it was independent from interval time to cholecystectomy, in contrast with Odditis, suggesting an anatomical condition for CCBP and a functional one for Odditis. LFT analysis showed no differences in relation to BPR incidence. LFT excluding AP and GGT returned to normal values with significant differences in OV/MNV when BPR was present which points to an increased cholestasis in BPR group. US dilatation of CBD was noted in 10.3% and was associated to CCBP.
ConclusionsBPR in BP increases cholestasis and contributes to confusion in the estimation of common bile duct stones increasing ERCP-EE rates. US and biochemical markers of CBDS show a low specificity due to BPR-CCBP which suggests that MRI-cholangiography is a mandatory exploration before ERCP-EE examination.
Estudio de la prevalencia de reflujo biliopancreático (RBP)/canal común biliopancreático (CCBP) en pacientes con pancreatitis biliar (PB) sometidos a colecistetomía (CST) y colangiografía intraoperatoria (CIO) y análisis de la cinética de pruebas funcionales hepáticas (PFH) en comparación con un grupo control (GC) de colelitiasis sintomática.
Material y métodosEstudio retrospectivo de 107 pacientes consecutivos con PB. Se determinó la existencia de RBP-CCBP en la CIO y se analizaron las PFH al ingreso (AI), a las 48 horas y en el examen preoperatorio (AP). La variación analítica se analizó entre grupos según existencia de RBP-CCBP y entre el AI y AP, según intervalo ingreso-intervención (III) y dentro del mismo grupo mediante determinación de la ratio valor observado-valor máximo normal (VO/VMN).
ResultadosLa incidencia de CCBP fue de 38,3% en PB vs 5,0 en GC (p=0,0001) y fue independiente del III a diferencia de la odditis apuntando a una alteración anatómica para la primera y funcional para la segunda. Las variaciones analíticas no muestran diferencias entre grupos en función de la existencia de CCBP, pero con ausencia de diferencias al analizar la ratio VO/VMN en FA y GGT, lo que indica un mayor grado de colestasis en los pacientes con RBP-CCBP. La incidencia de dilatación de vía biliar US fue del 10,3% asociándose a CCBP.
ConclusionesEl RBP-CCBP en PB genera un mayor grado de colestasis e incertidumbre en la estimación de coledocolitiasis asociada y excesiva sobreindicación de ERCP-EE. Los marcadores US y bioquímicos de coledocolitiasis tienen una baja especificidad en PB por la existencia de CCBP lo que obliga a incluir a la colangiografía por RMN como exploración previa a la ERCP-EE.
Biliary pancreatitis (BP) is triggered by the onset of biliopancreatic reflux (BPR) secondary to transient lithiasic obstruction of the opening of the common bile duct and the Wirsung duct at the papilla of Vater. This combined mouth or biliopancreatic common channel (BPCC) occurs in 67% the patients1 while an independent opening of the ducts occurs in the rest of the population.
BPR demonstration and therefore the existence of BPCC through intraoperative cholangiography (IOC) or trans-Kehr intraoperative cholangiography2 occurs in 7%–50% of the patients who undergo a cholangiography3 with an increase in the prevalence of BP up to 87%.4
BPCC allows the gallstones of small size (microlithiasis) to produce a transient ampullary obstruction, which is initially mechanical and subsequently inflammatory, and at the same time, generates BPR causing BP,5 without the need of the existence of choledocian occupation maintained for BP development or maintenance.
Our study had two purposes. First, to assess the incidence of BPR and BPCC in patients with BP who undergo cholecystectomy and routine IOC, in order to analyze the possible differences attributable to its presence in patients with BP translated in terms of alterations in the liver function tests (LFT) and assess the possible importance of its existence. Secondly, to analyze the kinetics of LFT alterations in order to establish a selective indication of preoperative explorations before cholecystectomy in patients with BP.
Material and MethodsRetrospective case study of patients with a diagnosis of BP and subsequent scheduled cholecystectomy subject to IOC. The study included 107 patients with BP as the first episode during a period of 48 months. Exclusion criteria were the following: recurrent BP, pancreatitis post-endoscopic retrograde cholangiopancreatography (ERCP), chronic alcoholism, hypertriglyceridemia, hypercalcaemia or use of pancreatitis associated drugs. BP was diagnosed in patients with abdominal pain and elevated amylase greater than 3 times the standard level (amylase >380). Liver function tests at the time of admission (LFTA) were performed in all patients, including the urgent laboratory test at admission, and after 48h, in order to establish the Ransom-Inrie criteria.6 Patients who were subject to ERCP and sphincterotomy (ERCP-ES) and those who presented severe BP with necrosis, abscess, pseudocyst or organ failure were excluded.
Urgent abdominal ultrasound was performed in all cases as well as abdominal CT with contrast in selected cases. The presence of bile duct dilatation (BDD) by ultrasonography was established according to Bachar parameters in relation to the age ranges.7
All patients received initial medical treatment and, after a variable period, they underwent scheduled surgery, either at admission or later on, prior preoperative laboratory test with complete liver profile (PLFT).
A series of 80 patients were used as a control group (CG) and were submitted to elective cholecystectomy and IOC, for uncomplicated symptomatic cholelithiasis; such patients were randomized during the study period and underwent surgery in the same week as BP cases.
IOC was reviewed by 2 of the authors (Planells Roig and Peiró Monzó), excluding from the study the cases where there was no consistency between them as to the existence of BPR. Biliopancreatic reflux/Biliopancreatic common channel (BPR-BPCC) was defined as the existence of retrograde filling of the Wirsung duct during IOC secondary to BPCC (length >2.5mm in cholangiographies). Findings of BPR and odditis (BPR-BPCC-O) were defined when there was BPR-BPCC and absence of contrast in the duodenum without choledocholithiasis, after the bile duct instrumental exploration. The diagnosis of choledocholithiasis (CBDS) was considered when confirmed by bile duct instrumental exploration.
The study of the laboratory values included the admission exam (LFTA) and the pre-surgical exam (PLFT). The following values were considered as pathological values: bilirubin >1.5mg/dl, ALP >140mg/dl, SGOT >65U/l, SGPT >77 U/l, GGT >70.
Since the biochemical data does not follow a normal distribution,8 the statistical study is presented as the mean and the Mann Whitney test is used to compare group of patients in the continuous variables. Paired Wilcoxon test was used to compare the differences within each group. Chi-square test with Yates correction was used in discrete variables. A result with P<.05 was considered significant. The analysis of OV/MNV ratio (observed value/maximum normal value) was used to compare the variations of the different function tests (increases of the reference value), which allows to contrast the maximum independent enzyme impact regardless of the type of analytic determination.8
ResultsNo significant differences were found with respect to the distribution by age and gender. The average age was 59.9 (14.3) in the group of BP vs 55.9 (13.5) in the CG, P=.059 (−8.070; 0.150) although the difference in ages was significant when CBDS cases were excluded in both groups, 55.5 (13.8) in the CG compared to 59.7 (14.5) in the BP group (P=.035–8.605; 0.157). Distribution by gender was of 17 men (21.3%) and 63 women in the CG vs 35 men (32.7%) and 72 women in the BP group (Chi S 2.955, P=.058 F). In the BP group without CBDS, the average age of patients with BPR-BPCC-O was 58.8 (13.9) compared to the group without BPR 60.6 (15.2) (P=.536). There were no differences in the distribution by gender, and the BPR-BPCC-O incidence was 57.6% in men and 47.8% in women.
From the 107 patients with BP, 74 underwent surgery in an interval of 8 weeks after the acute episode. The interval admission/intervention (III) in this group was of 2.2 (1.3) weeks in 59 cases and 6.0 (1.1) weeks in 10 cases. There were 22 cases (29.7%) of readmission due to BP in this group. In patients who underwent surgery after 8 weeks (No.=33), the readmission rate was of 5 cases (15.2%) where surgery was performed at an interval lower than 12 weeks 7 and greater than 12 weeks 26.
Cholangiographic FindingsIOC was performed in all patients, it was normal in 105 cases, 78.8% of the patients of the CG and 39.3% of the BP group (Chi S 29.004; P=.000). It failed in 4 cases, 2 in each group (2.1% of the whole series). Incidence of BPR-BPCC was 38.3% in the BP group and only 5.0% in the CG group (Chi S 27.8; P=.000). On the other hand, the incidence of BPR-BPCC-O was 48.6% in the BP group compared to the CG group (0 cases) (Chi S 41.476; P=.000). All cases of odditis13 occurred in the BP group (12.1%). CBDS rate confirmed by the bile duct instrumental exploration was of 14 cases (14/187) similar in both groups, 8.8 in the CG and 6.5 in the BP group (Chi S 0.322; P=.857), and it did not associate any case to BPR-BPCC-O. There were 4 (2.1%) IOC false positive cases and one CBDS false negative case.
BPR-BPCC incidence was of 50.0% in patients who underwent surgery in an interval of 4 weeks, 53.8% in patients operated between 4 and 8 weeks, 50% in patients operated between 8 and 2 weeks and 41.7% in patients operated further after 12 weeks in the BP group.
OdditisIncidence of odditis was 75% in patients who underwent surgery during the first 4 weeks and 25% after this interval, always associated to BPR-BPCC, which suggests more irritation post-BP than morphological alteration, unlike BPR-BPCC, whose temporary distribution does not show any differences based on the surgical interval as described in the previous paragraph.
Ultrasound FindingsMicrolithiasis incidence was greater in the BP group (9.7% vs 2.5%) Chi S 3.819 (P=.045 F). There was evidence of gallbladder wall thickening (chronic cholecystitis) in 22.5% of the control group and 19.4% in the BP group. In 2.9% of the patients with BP there was evidence of scleroatrophic gallbladder. In the BP group, the ultrasound showed BDD in 11 cases (10.3%) where none of them presented CBDS with a BPR-BPCC-O incidence of 7 cases (63.6%).
Laboratory Tests Alteration in Patients With Choledocholithiasis. Biochemical Markers of CholedocholithiasisIn the BP group, incidence of CBDS was of 6 cases in the first 4 weeks and of one case in the following weeks. The analysis of the LFTA and PLFT showed no differences in (TBil, SGOT, SGPT) among patients with and without CBDS, with significant differences only in the case of alkaline phosphatase and in the preoperative exam 203.6 (103.1) in patients with CBDS vs 118.6 (93.4) (P=.017) in patients without CBDS. Differences in the preoperative GGT 280.3 (352.1) vs 112.5 (108.3) did not reach statistical significance.
In the CG, a significant difference was evidenced in the preoperative TBil 2.4 (5.0) in patients with CBDS compared to those who did not present CBDS 0.5 (0.3), P=.002 (0.7374; 3.0471) without differences in the rest of the SGOT, SGPT variables although both ALP and GGT showed greater values but without any significance.
Bilirubin was dichotomized at admission in the BP group with a cut-off of 5mg/dl (indicative values of clear bile obstruction) without evidence of any relation with the BPR-BPCC-O or CBDS existence (in patients with CBDS, 5 of 7 cases presented bilirubin values lower than 5mg/dl); therefore, its usefulness in CBDS prediction was low.
Likewise, TBil was dichotomized at the preoperative laboratory tests with a cut-off of 1.5mg/dl, not allowing to detect 5 of the 7 cases of CBDS, neither showing correlation with the incidence of BPR-BPCC nor BPR-BPCC-O.
Ranson's Criteria and Biliopancreatic Reflux/Biliopancreatic Common ChannelPatients meeting 3 or more Ranson's criteria (No.=41; 38.3%) showed amylase levels at admission greater than 2431.0 (1329.6) vs 1657.4 (1171.4) compared to those meeting less than 3 criteria (No.=66), P=.002 (CI 287.0; 1260.2). In the 10 patients who required admission in the ICU, Ranson's score was of 3.2 (1.3) compared to 2.0 (1.5) in those who did not require admission [P=.015 (0.2024; 2.1151)]. There were no differences in Ranson's score among patients who suffered recurrence/re-admission after the acute outbreak of BP (No.=27).
Incidence of BPR-BPCC-O showed no relation with Ranson's score, 19 cases (46.3%) in patients meeting 3 or more criteria compared to 33 cases (50.0) in patients meeting less than 3 criteria and the score was similar in patients with or without BPR-BPCC-O 1.9 (1.4) vs 2.3 (1.6) (P=.338).
Severe Biliary Pancreatitis and Biliopancreatic Reflux/Biliopancreatic Common Channel-OIncidence of BPR-BPCC-O was greater in patients who required admission in the ICU (13.7%) compared to those who did not present it (4.1%), although not reaching a statistical significance but the need for urgent surgery due to cholangitis was significantly greater in patients with BPR-BPCC-O (12.5%) compared to those patients without BPR-BPCC-O (1.7%), Chi S 4.994; P=.036 (F).
Admission Laboratory Tests (Liver Function Tests) and Biliopancreatic Reflux/Biliopancreatic Common Channel-OLFTA from patients with BP, excluding the cases of associated CBDS, by virtue of the existence of BPR-BPCC-O in the IOC, showed no evidence of significant differences.
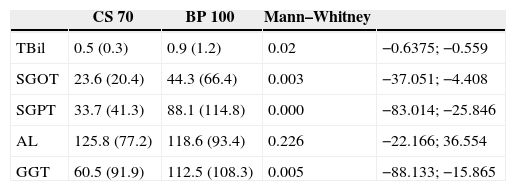
Preoperative Laboratory Tests. Control Group vs Biliary PancreatitisPreoperative liver function tests between CG and BP group, excluding patients with CBDS, showed significant differences between both groups as shown in Table 1.
Preoperative Laboratory Tests (PLFT) in Patients of the Control Group vs PB Group Excluding the Cases With CBDS.
| CS 70 | BP 100 | Mann–Whitney | ||
|---|---|---|---|---|
| TBil | 0.5 (0.3) | 0.9 (1.2) | 0.02 | −0.6375; −0.559 |
| SGOT | 23.6 (20.4) | 44.3 (66.4) | 0.003 | −37.051; −4.408 |
| SGPT | 33.7 (41.3) | 88.1 (114.8) | 0.000 | −83.014; −25.846 |
| AL | 125.8 (77.2) | 118.6 (93.4) | 0.226 | −22.166; 36.554 |
| GGT | 60.5 (91.9) | 112.5 (108.3) | 0.005 | −88.133; −15.865 |
CS: elective cholecystectomy by uncomplicated symptomatic cholelithiasis without associated choledocholithiasis; BP: biliary pancreatitis without associated choledocholithiasis.
Due to such difference, the interval influence between the BP acute episode and the surgical intervention was analyzed, (III) as regards the laboratory alterations of the BP group depending on the week of intervention, showing a tendency towards analytical normalization by week 4. Therefore, the cohort value was used to assess PLFT alterations.
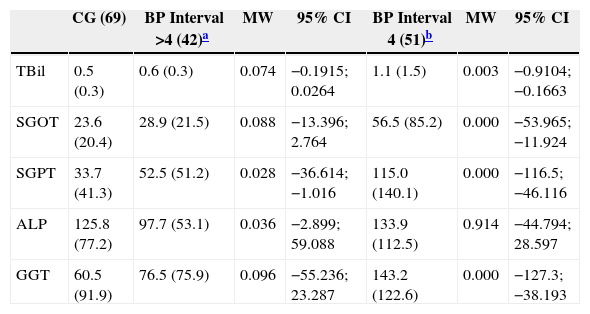
Patients who underwent surgery in an interval of 4 weeks were submitted to surgery 1.9 (1.3) weeks after such interval. Incidence of BPR-BPCC-O was similar based on III, and were 52.9% and 43.5%, respectively. In any of the 2 intervals (>0–4 weeks) LFTs show significant differences in the BP group based on III with the CG (Table 2), the greater as well as the lower the interval (Table 3), which generates a clear uncertainty in the assessment of the possibility of CBDS since in patients with BP, the laboratory alteration persists significantly with a biochemical pattern suggesting a potential existence of CBDS, though such alteration diminishes with time.
Preoperative Laboratory Variations (PLFT) Between the Control Group (CG) and the Biliary Pancreatitis Group Without CBDS According to the Intervention Interval.
| CG (69) | BP Interval >4 (42)a | MW | 95% CI | BP Interval 4 (51)b | MW | 95% CI | |
|---|---|---|---|---|---|---|---|
| TBil | 0.5 (0.3) | 0.6 (0.3) | 0.074 | −0.1915; 0.0264 | 1.1 (1.5) | 0.003 | −0.9104; −0.1663 |
| SGOT | 23.6 (20.4) | 28.9 (21.5) | 0.088 | −13.396; 2.764 | 56.5 (85.2) | 0.000 | −53.965; −11.924 |
| SGPT | 33.7 (41.3) | 52.5 (51.2) | 0.028 | −36.614; −1.016 | 115.0 (140.1) | 0.000 | −116.5; −46.116 |
| ALP | 125.8 (77.2) | 97.7 (53.1) | 0.036 | −2.899; 59.088 | 133.9 (112.5) | 0.914 | −44.794; 28.597 |
| GGT | 60.5 (91.9) | 76.5 (75.9) | 0.096 | −55.236; 23.287 | 143.2 (122.6) | 0.000 | −127.3; −38.193 |
CG-CBDS: control group excluding patients with choledocholithiasis.
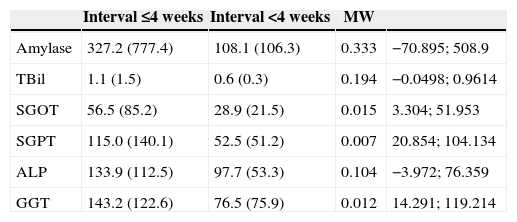
Preoperative Laboratory Variations (PLFT) Biliary Pancreatitis/Intervention Interval (III).
| Interval ≤4 weeks | Interval <4 weeks | MW | ||
|---|---|---|---|---|
| Amylase | 327.2 (777.4) | 108.1 (106.3) | 0.333 | −70.895; 508.9 |
| TBil | 1.1 (1.5) | 0.6 (0.3) | 0.194 | −0.0498; 0.9614 |
| SGOT | 56.5 (85.2) | 28.9 (21.5) | 0.015 | 3.304; 51.953 |
| SGPT | 115.0 (140.1) | 52.5 (51.2) | 0.007 | 20.854; 104.134 |
| ALP | 133.9 (112.5) | 97.7 (53.3) | 0.104 | −3.972; 76.359 |
| GGT | 143.2 (122.6) | 76.5 (75.9) | 0.012 | 14.291; 119.214 |
The analysis of OV/MNV ratio (observed value/maximum normal value) (maximum normal value/determined value ratio) which allows to evidence the variation with respect to the normal value and therefore the comparison of the variations of the different function tests between them showed no significant differences between patients who underwent surgery in an interval >0<4 weeks and the existence of BPR-BPCC-O (Mann Whitney) when LFTA and PLFT were analyzed.
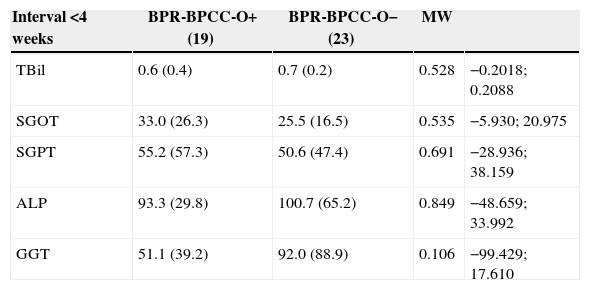
Differences in LFT were not only evidenced between the CG and BP groups but also in the BP group based on III (Table 3). These analyses evidenced differences in the LFT, although they were only significant in the case of SGOT, SGPT and GGT. This fact suggested a residual inflammatory alteration or a different analytical behaviour based on the existence of BPR-BPCC-O. The hypothesis that the PLFT alterations were secondary to BPR-BPCC-O was initially ruled out when analysing the same compared to the incidence of BPR-BPCC, as it was similar in both intervals (intervention >0<4 weeks) (Table 4) not showing significant differences in the PLFTs. At this point, the conclusion derived from the kinetic analysis of the PLFTs alterations should be the BPR-BPCC-O has no analytical translation and that analytical alterations should be attributed to other factors secondary to BP.
Preoperative Laboratory Variations in Biliary Pancreatitis, Intervention Interval and BPR-BPCC-O.
| Interval <4 weeks | BPR-BPCC-O+ (19) | BPR-BPCC-O− (23) | MW | |
|---|---|---|---|---|
| TBil | 0.6 (0.4) | 0.7 (0.2) | 0.528 | −0.2018; 0.2088 |
| SGOT | 33.0 (26.3) | 25.5 (16.5) | 0.535 | −5.930; 20.975 |
| SGPT | 55.2 (57.3) | 50.6 (47.4) | 0.691 | −28.936; 38.159 |
| ALP | 93.3 (29.8) | 100.7 (65.2) | 0.849 | −48.659; 33.992 |
| GGT | 51.1 (39.2) | 92.0 (88.9) | 0.106 | −99.429; 17.610 |
| Interval ≤4 weeks | BPR-BPCC-O+ | BPR-BPCC-O− | MW | |
|---|---|---|---|---|
| TBil | 1.1 (1.9) | 1.0 (0.9) | 0.122 | −0.7841; 0.9508 |
| SGOT | 58.2 (94.4) | 54.4 (74.5) | 0.681 | −43.806; 51.455 |
| SGPT | 92.7 (130.3) | 140.0 (148.9) | 0.107 | 124.279; 29.707 |
| ALP | 134.7 (92.6) | 132.9 (136.6) | 0.773 | −70.754; 74.256 |
| GGT | 141.5 (112.9) | 144.9 (134.9) | 0.986 | −90.364; 83.541 |
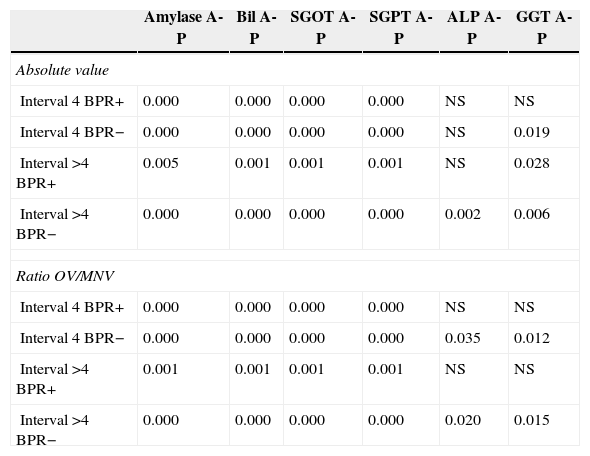
However, when analysing the differences between LFTA and PLFT (Wilcoxon) within the same groups based on the interval to the intervention and the existence of BPR-BPCC-O, excluding patients with CBDS, both in absolute values as with the OV/MNV ratio (Table 5), it was evidenced that in patients with BPR-BPCC-O, decrease (normalization) in LFT values between the acute episode and intervention was significant in all variables except from ALP and GGT, both in patients who underwent surgery during the first 4 weeks as well as in patients who belatedly underwent surgery. Even more, when analysing OV/MNV ratio in patients with BPR-BPCC-O, the decrease in LFT was not significant in ALP and GGT, both markers of cholestasis both at 4 weeks and in an greater interval, and it was significant in the group without BPR-BPCC-O, which would indicate that the existence of BPR-BPCC produces a higher degree of cholestasis, persistent in time, and that the existence of alterations in the PLFT may indicate the existence of BPR-BPCC-O or its biochemical consequence in the absence of CBDS.
Analysis of the Different Preoperative-Admission Laboratory Tests by Intervals and Existence of BPR-BPCC-O. Wilcoxon Test. Observed Value/Maximum Normal Value Ratio Analysis.
| Amylase A-P | Bil A-P | SGOT A-P | SGPT A-P | ALP A-P | GGT A-P | |
|---|---|---|---|---|---|---|
| Absolute value | ||||||
| Interval 4 BPR+ | 0.000 | 0.000 | 0.000 | 0.000 | NS | NS |
| Interval 4 BPR− | 0.000 | 0.000 | 0.000 | 0.000 | NS | 0.019 |
| Interval >4 BPR+ | 0.005 | 0.001 | 0.001 | 0.001 | NS | 0.028 |
| Interval >4 BPR− | 0.000 | 0.000 | 0.000 | 0.000 | 0.002 | 0.006 |
| Ratio OV/MNV | ||||||
| Interval 4 BPR+ | 0.000 | 0.000 | 0.000 | 0.000 | NS | NS |
| Interval 4 BPR− | 0.000 | 0.000 | 0.000 | 0.000 | 0.035 | 0.012 |
| Interval >4 BPR+ | 0.001 | 0.001 | 0.001 | 0.001 | NS | NS |
| Interval >4 BPR− | 0.000 | 0.000 | 0.000 | 0.000 | 0.020 | 0.015 |
A: admission; P: preoperative; Ratio OV/MNV: ratio between the obtained value and the maximum normal value in the liver function test performed.
In 1976, studies on gallstones in stool of patients with BP9 generated the “migratory stone” theory, revealing that the CBDS rate was10,11 63%–75% (at 48h after admission), decreasing to 5% when the acute episode had finished. Recent studies (ERCP) confirm that the incidence of CBDS in the first 48h is 70%12 reaffirming the pathogenesis of the BP by transient occlusion of the ampulla of Vater by biliary sludge or gallstones13 that, in most of the patients, spontaneously pass into the duodenum.14
BPCC-BPR determined by IOC occurs in 7%–50% of patients undergoing cholecystectomy3 increasing in BP up to 87%,4 and is 5% in patients with uncomplicated symptomatic cholelithiasis4,10,15–18; it has no relationship with the pressure applied to contrast material during IOC.19 In our country, the reported incidence is 6%–48.1%,20,21 achieving in our series a 51.0% in BP in contrast to 14.6 of CG.
The BPCC-BPR is not related to choledocian obstruction.18,19 In patients with CBDS and BPR the trans Kher IOC does not evidence disappearance of the BPR,10,21–23 which indicates absence of relation between BPR, choledocholithiasis and the choledochus diameter.15 Furthermore, the ampullary cholangio-manometry in patients with BP shows a reduced diameter of the BPCC originating either primary or secondary BPR.23 Finally, in patients with BP and choledochotomy on a T-tube, an elevation of trypsinogen and an increase of amylase in choledochal drainage have been shown reflecting the functional obstruction of the sphincter of Oddi and the existence of retrograde reflux through the BPCC in the absence of CBDS.24
Patients with microlithiasis (<3mm) are more likely to develop BP while acute cholecystitis is more common in larger gallstones.9,21 The BDD is normal in patients with BP without CBDS (10.3% in our series). In this group, gallstones are usually 3–7mm sized in diameter9,21 and the BDD is secondary to the distal transient obstruction originating retrograde biliary pressure increase,20 and its morphological translation is the BD dilation by ultrasonography and the cholangiographic BPR as in our study, where the existence of BDD is associated with a high incidence of BPR-BPCC-O in the absence of CBDS.
The high incidence of BPCC (67%–80%), though not absolute in BP, could demonstrate that the BPCC is transient in relation to the passage of the gallstone and subsequent inflammatory papillary oedema25,26,32,33 with following functional normalization by reversing the BPR. On the contrary, our study shows that the prevalence of BPR is similar in patients who underwent surgery before and after 4 weeks, remaining constant throughout different time intervals considered for surgery, which points to an anatomical rather than transient functional alteration.
Odditis is related to repeated episodes of lithiasic migration in patients with BP and its incidence is high in patients who suffered BP, being its translation uncertain as it could be assumed either as a morphological substrate of the BP aetiology or a morphological consequence of the biliopancreatic confluent “irritation”.9 In our series, odditis seems to be more an “irritative” process since it concentrates in 75% of cases surgically treated during the first 4 weeks, as opposed to the existence of BPR-BPCC that remains constant over time.
The incidence of CBDS in BP and early ERCP reaches 55.9%.27,28 However, routine IOC in patients with previous BP without BD dilation and LFT normalization shows a much lower incidence of CBDS, of 8.5%,29 and a 5.1% residual lithiasis rate which decreases to 2.8% when no IOC is performed.28 This disparity in the incidence of CBDS depending on the admission-intervention interval points to the necessity to establish an indication of time interval for ERCP-MRCP or LC practice based on the estimation of probability of associated CBDS.
Although BP has been considered as a clinical indicator of CBDS, its PPV is low (0.26).30 In general, elevations in TBil, ALP and SGPT along with the existence of BDD are considered CBDS markers.30 However, in BP, the low specificity of ultrasound and biochemical markers can cause unnecessary ERCP,27,31 since both ALP and GGT have low PPV and NPV. Moreover, SGOT, SGPT and bilirubin in the early phase of the BP are not useful in the prediction of CBDS.27 Transient elevation of transaminases is related to biliary aetiology of pancreatitis, mainly SGPT (PPV 80%–90%),32 by transient occlusion of the ampulla of Vater33 whose biochemical translation is the bilirubin and SGOT/SGPT elevation, and stabilises after the disimpaction.34 Moreover, the initial rising of the LFT in the BP follows a proven kinetics of normalization35 or increase33 and bilirubin26 follows a crescendo-decrescendo pattern35 in relation to whether papillary obstruction is transient (mechanical by the passage of sludge or gallstone or inflammatory by papillary oedema) or prolonged, being the interval of biochemical normalization essential for the indication of complementary examinations of the BD as MRCP36 or ERCP as well as to define the timing of cholecystectomy.
The LFTs alteration (in particular ALP and TBil) causes uncertainty in the prediction of CBDS and does not allow to discriminate cases with CBDS or absolute values, or with the determination of the OV/MNV ratio of the LFTs.8 If we also consider that ultrasound parameters as diagnosis of CBDS and/or BDD, which in the acute phase can occur in 9% and 31% of BP patients respectively, show a low PPV and NPV,27,31,37 uncertainty in the estimation of probability of CBDS will provoke an excess of preoperative explorations, such as ERCP or MRCP and would seek the presence of other generating mechanisms of laboratory alterations observed in PB in the absence of CBDS38 as the existence of BPR-BPCC.
In our study, as well as in that of Fumino,39 there are no evident statistically significant differences in the LFTs at admission among patients with BP based on the existence of BPR-BPCC. Conversely, analysis of LFTA and PLFT variations evidences significant differences in TBil, SGOT, and SGPT both in patients either with or without BPR-BPCC, but not in ALP and GGT. The analysis of the OV/MNV ratio at admission and preoperative stage confirms that the variations are not significant in the BPR-BPCC group in ALP and GGT, i.e., there is no substantial normalization between the values at admission and the preoperative values, thus it can be concluded that, in patients with BPR-BPCC, there would be a greater biliary evacuation difficulty translated into a greater degree of cholestasis, an absence of major differences between the 2 points of analytical determination and therefore a lower normalization or a crescendo pattern in this group. In consequence, the existence of alterations in the PLFT must not be taken as a single value, but comparatively analyzed with the values at admission to estimate their degree of normalization and thus be attributed to BPR-BPCC or CBDS.
Thus, in patients with a decrescendo pattern of the LFTs and defined as high ultrasound risk of CBDS (suspected CBDS or BDD), the preoperative study of BD should be restricted to MRCP that would also allow to exclude the IOC during the LC, while in patients with a crescendo pattern without normalization of the LFTs, in which the presence of BPCC-BPR could explain the non-analytic normalization or incomplete normalization, MRCP should precede ERCP40 and not be indicated as a first line exploration of the bile duct. In either case, the indication for ERCP must be restricted to MRCP findings regarding false positives and negatives resulting from biochemical markers and US of CBDS in BP, and should not be considered as first line scan.
The main contribution of our study, although limited by its retrospective nature, has been the determination of the kinetics of laboratory alterations in patients with BP depending on the interval to the intervention and the existence of BPCC-BPR-O, which allows to demonstrate that there is a greater cholestatic pattern responsible for the over-indication of complementary examinations in patients with BPCC for the uncertainty that it creates in relation to the existence of bile duct occupation. In addition, even though the sample is reduced, we have evidenced an association between serious BP requiring the admission in ICU and the existence of BPR-BPCC, which could be secondary to the greater degree of cholestasis in these patients and, therefore, the greater probability of cholangitis. On the other hand, our study identifies odditis as an irritant process with its frequency diminished in time as opposed to the BPR-BPCC which is stable over time. We have proved a high prevalence of BPR-BPCC in patients with BP in addition to demonstrating persistent laboratory alterations after the acute episode of BP with progressive normalization as from week 4. Laboratory alterations in the LFTs after the acute episode of BP generate that preoperative CBDS exclusion cannot be based on liver profile but that it will require complementary imaging studies, such as MRCP. The ERCP-ES must be indicated only after image scans with MRCP. Intraoperative IOC in patients with previous BP should be performed only in a selective manner and not routinely when MRCP is uncertain, or after ERCP-ES. The implementation of a prospective study to calculate the reduction or normalization estimated in the LFTs depending on the presence of BPR-BPCC would allow identification of patients with normalization or absence of LFT without risk of associated CBDS.
Conflict of InterestThe authors declare that there are no conflicts of interests.
Please cite this article as: Planells Roig M, Ponce Villar Ú, Peiró Monzó F, Coret Franco A, Orozco Gil N, Bañuls Matoses Á, et al. Pancreatitis biliar. Cinética de pruebas funcionales hepáticas y canal común biliopancreático - reflujo biliopancreático. Cir Esp. 2015;93:326–333.