The surgical treatment for low rectal cancer involves an ultra-low anterior resection with complete mesorectal resection and coloanal anastomosis. Two-stage coloanal anastomosis such as the Turnbull–Cutait technique represents an option for patients with low rectal cancer.
Clinical caseA 69 year-old female patient with a diagnosis of adenocarcinoma (T2N1), located 4cm from the anal margin. She received neoadjuvant radiotherapy. An ultra-low anterior resection and total resection of the mesorectum were performed. The intestinal transit was reconstructed by coloanal anastomosis using the Turnbull–Cutait technique.
ConclusionColoanal anastomosis with the Turnbull–Cutait technique represents a primary option for patients with low rectal cancer, avoiding a loop ileostomy, its economic impact and on their quality of life.
El tratamiento quirúrgico para el cáncer de recto del tercio inferior implica la realización de una resección anterior ultrabaja de recto con resección total de mesorrecto y una anastomosis coloanal. La anastomosis coloanal en 2 tiempos según Turnbull-Cutait podría ser una opción en pacientes con cáncer de recto del tercio inferior.
Caso clínicoPaciente femenina de 69 años de edad con diagnóstico de adenocarcinoma (T2N1), localizado a 4cm de margen anal. Recibe radioterapia neoadyuvante. Se realiza una resección anterior ultrabaja y la resección total del mesorrecto. El tránsito intestinal se reconstruye mediante una anastomosis coloanal de tipo Turnbull-Cutait.
ConclusiónLa anastomosis coloanal en 2 tiempos según Turnbull-Cuatit podría ser una opción primaria en pacientes con cáncer de recto del tercio inferior para evitar la realización de ileostomía de protección y su impacto económico y en la calidad de vida.
Surgical treatment for cancer of the lower third of the rectum involves an ultra-low anterior resection with complete mesorectal resection and if sphincter conservation is possible, the reconstruction possibilities are mechanical coloanal anastomosis or manual coloanal anastomosis.1–3 The main disadvantage of coloanal anastomosis is suture dehiscence, an event which is recorded in between 2.9% and 20% of cases.1–3 In half of these cases the patients require surgical reintervention3,4 and a third require a permanent colostomy.5 A protection ileostomy is often performed with a view to limiting the impact of possible coloanal anastomotic dehiscence. Creating this stoma is not without its complications, which present in approximately 10% of cases.6,7
Turnbull was undertaking delayed two-stage transanal anastomoses in 1952, in adults with mid rectal cancer and in children with Hirschprung's disease, in order to avoid end colostomy.8–10 At the same time, Cutait was using the same technique in adult patients with acquired megacolon of Chagas’ disease.10,11
Recently, Turnbull–Cutait's technique has been reintroduced, in order to avoid constructing a permanent colostomy in patients reoperated for colorectal anastomosis, with chronic pelvic infection, persistent rectovaginal or rectourethral fistulae and complex perianal fistulising Crohn's disease.10,11
In 1999, Baulieux et al.12 reintroduced the Turnbull–Cutait technique in patients with low rectal cancer undergoing radiotherapy, in order to avoid suture complications.
In addition, there are other groups who prefer performing this technique in order to avoid a temporary bypass stoma.13
Clinical caseA 69-year-old female patient presenting with chronic diarrhoeal syndrome, and passing 30 evacuations of liquid consistency per day. On targeted physical examination (rectal examination), a rectal tumour was palpated approximately 4cm from the anal verge. A colonoscopy was performed which revealed a hairy polypoid formation occupying ¾ of the intestinal lumen.
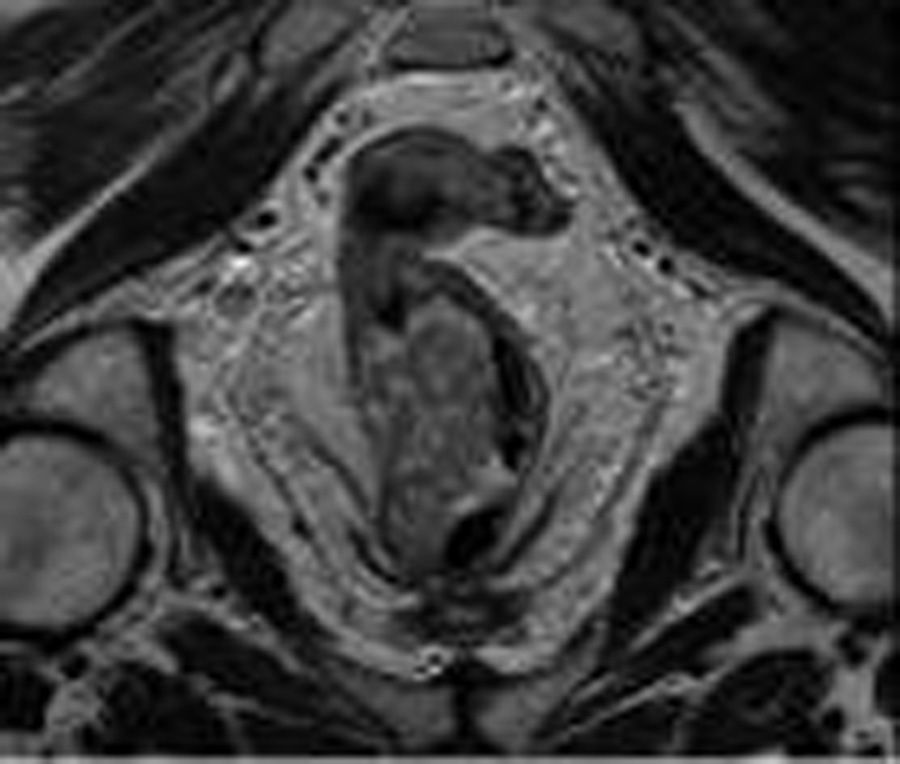
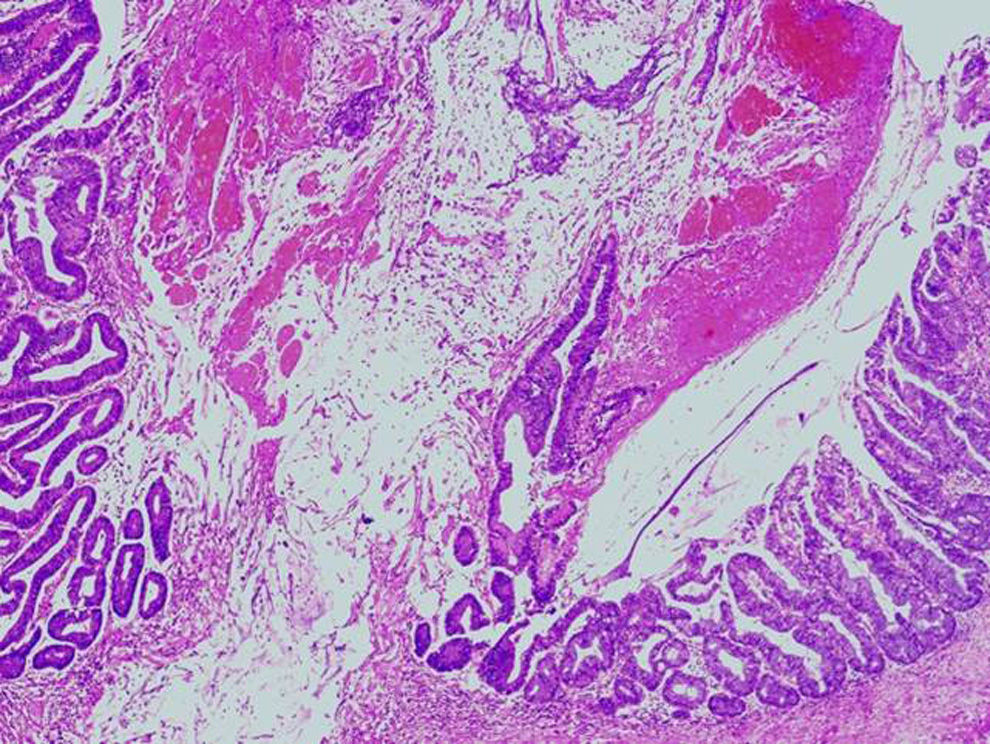
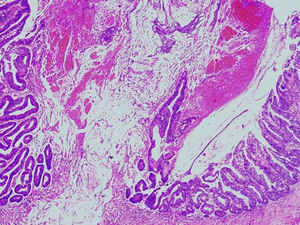
The patient was referred to the Colorectal Surgery Unit of the Hospital Vall d’Hebron where the study protocol was completed. Rigid rectoscopy was performed that revealed a non-stenosing lesion 4cm from the anal verge. Endorectal ultrasound showed a polypoid lesion ultrasonically degenerated down to the muscularis propria with pathological adenopathies, stage T2N+. Rectal magnetic resonance showed the lesion in the lower rectum on the right lateral side of 23mm×27mm, infiltrating the most cranial fibres of the internal sphincter, with a suspicious mesorectal lymph node, stage T2N1 (Fig. 1). Thoraco-abdominal axial computed tomography revealed the aforementioned lesion and metastatic disease was ruled out. Histopathological study of the lesion reported a tubulovillous adenoma with high grade epithelial dysplasia (Fig. 2).
The patient underwent 28 presurgical radiotherapy sessions (primary tumour with 50.4Gy, pelvic chains with 45Gy).
An elective surgical procedure was performed in which the lower rectal tumour was resected by proctectomy, and complete mesorectal dissection by transanal minimally invasive surgery (TAMIS), using the GelPOINT device (Applied Medical, Rancho Santa Margarita, CA, USA), preserving the sphincters. Mobilisation of the descending colon and mesorectal dissection were assisted by abdominal laparoscopy.
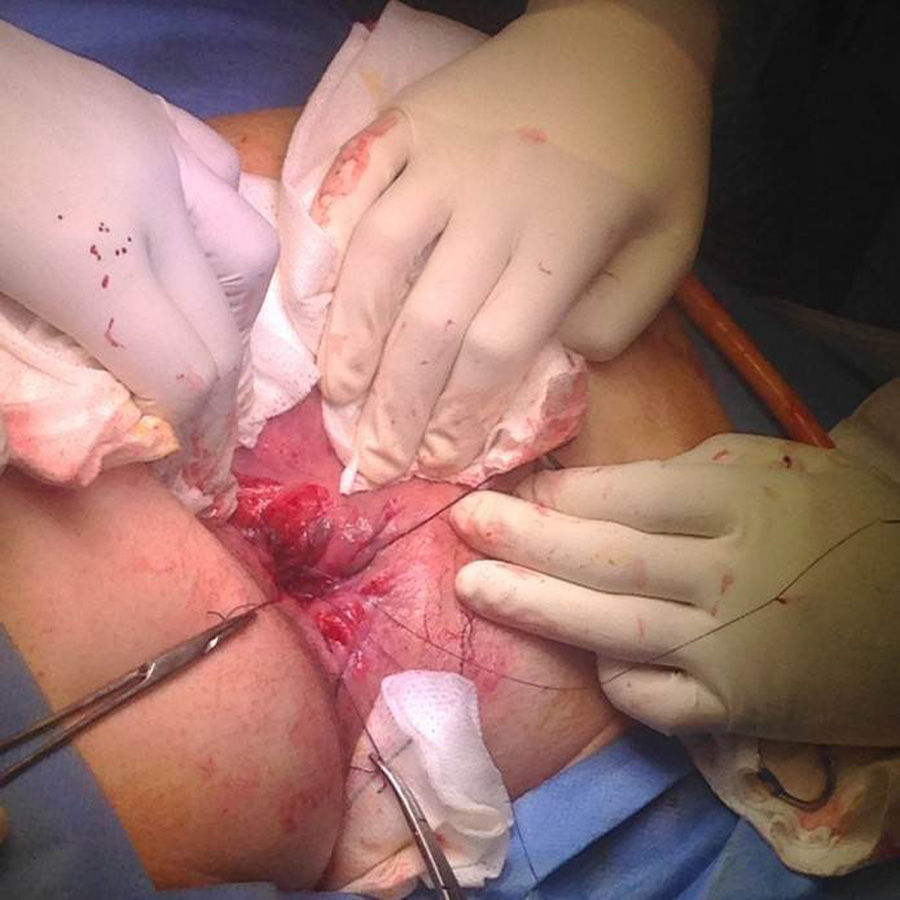
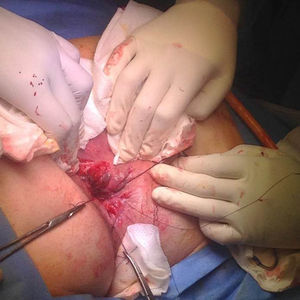
A Turnbull–Cutait-type anastomosis was made, once the intersphincteric resection had been completed, the rectum and the colon were extracted, the colon and sigmoid were resected, leaving a left colonic stump of approximately 10cm pulled through the anal canal, fixing the colon with two single stitches at the level of the anal canal (Fig. 3). After the perineal phase had been completed, the abdominal phase was completed with a suction drain in the pelvis, thus concluding the first surgical stage.
The patient was moved to a general ward, vascularisation of the pulled-through colonic stump was checked daily. She was given a liquid diet and complete parenteral nutrition in order to avoid faeces passing through the pulled-through colonic stump via the anus.
In the second surgical stage (7 days postoperatively), after placement of an anal retractor, the pulled-through colonic segment was sectioned at the level of the anal verge. A manual end-to-end coloanal anastomosis was made with single 3-0 polyglycolic acid sutures, including the entire colonic wall thickness and the musculature of the anal canal (Fig. 4). After the anastomosis had been completed (Fig. 5), good passage through the anastomosis was checked by rectal examination.
The patient was discharged from the department with no complications on the second postoperative day; she was followed-up as an outpatient. Seven months after the surgical treatment she presented no complications and is free of disease.
DiscussionAfter the development of suture and staple anastomosis techniques, interest was lost in the Turnbull–Cutait two-stage coloanal anastomosis procedure. However, it has resumed its role in conventional surgery of middle or low rectal cancer, both as elective treatment and as treatment of the complications of other sutures.10,13–16
In a retrospective study by Jarry et al.3 which included 100 patients with rectal tumours located at a mean distance of 5cm from the anal verge, treated surgically by total mesorectal excision plus two-stage coloanal anastomosis using the Turnbull–Cutait procedure, they describe a mortality of 3% and an overall postoperative morbidity of 36%. All the patients had a bypass ileostomy. Of the patients studied, 10 presented pelvic sepsis. Anastomotic dehiscence was observed in 2 cases and a rectovaginal fistula in one case. Two patients presented ischaemia of the pulled-through colon and 7 required reoperation for problems directly associated with the anastomosis. In terms of long-term complications, stenosis of the anastomosis was found in 15 patients, prolapse of the colic mucosa in 2, and a rectovaginal fistula in one. These outcomes can be explained because, on completing the first stage of the coloanal anastomosis using the Turnbull–Cutait technique, the colonic stump pulled through the anus was not sutured. Adherences and subsequent scarring of the tissues between the pelvis and the displaced stump that form between the first and second stages prevent the formation of an anastomotic fistula.3,10 Studies such as that by Remzi et al.16 mention that the Turnbull–Cutait technique significantly reduces the rate of anastomotic dehiscence and pelvic abscess compared to conventional coloanal anastomosis.
Recently, Biondo et al.13 performed a study to establish the rate of postoperative morbidity and mortality in patients operated using the Turnbull–Cutait procedure with delayed coloanal anastomosis. None of the patients were given a loop ileostomy; of the 17 patients included in the study, 6 patients (35.3%) presented one or more postoperative complications (paralytic ileus, wound infection, intra-abdominal collection, presacral collection, urinoma due to Bricker's procedure leakage and ischaemia of the pulled-through stump).
ConclusionTwo-stage coloanal anastomosis using the Turnbull–Cutait technique could be a primary option for patients with low rectal cancer, avoiding a loop ileostomy, its economic impact and impact on their quality of life.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: de León-Rendón JL, Vallribera-Valls F, Caspari C, Espín-Basany E. Técnica de Turnbull-Cutait en cáncer de recto inferior: reporte de un caso. Cir Cir. 2016;84:425–428.