The incidence of splenic artery aneurysm is not well known because it is often asymptomatic.
Clinical caseThe case is presented of a 40-year-old woman diagnosed with a splenic artery aneurysm. She was clinically asymptomatic. A three-dimensional angiographic study was performed. The artery embolisation was rejected, according to the results of the study; thus it was decided to perform a laparoscopic splenic-aneurysmectomy.
ConclusionsSplenic artery aneurysms may present with non-specific symptoms, such as abdominal pain or anorexia. However, 2–10% of aneurysms debut as spontaneous rupture. For this reason treatment is indicated in symptomatic aneurysms or those with rupture risk factors. In these cases there are different possibilities, such as therapeutic embolisation, endovascular stenting or surgery. Surgical approach varies depending on the location of the aneurysm in the splenic artery, enabling aneurysmectomy, splenic-aneurysmectomy, or aneurysm exclusion to be performed.
El aneurisma de la arteria esplénica es una patología cuya incidencia es poco conocida debido a su carácter mayoritariamente asintomático.
Caso clínicoSe comunica el caso de una mujer de 40años clínicamente asintomática diagnosticada de aneurisma de arteria esplénica. Tras cateterizar la arteria esplénica y realizar un estudio angiográfico tridimensional se descarta la posibilidad de embolización. Se decide esplenoaneurismectomía programada por vía laparoscópica.
ConclusionesLos aneurismas de arteria esplénica pueden dar síntomas inespecíficos como dolor abdominal o anorexia. Por otra parte, no debe subestimarse un 2-10% de aneurismas que comienzan con rotura espontánea. Es por esto que el tratamiento está indicado en aneurismas sintomáticos o con factores de riesgo de rotura. En este escenario existen varias posibilidades terapéuticas, como la embolización, la colocación de stent endovasculares o la cirugía. La técnica quirúrgica varía en función de la localización del aneurisma dentro del trayecto de la arteria esplénica, pudiendo realizarse aneurismectomía, exclusión aneurismática o esplenoaneurismectomía.
The splenic artery aneurysm includes all dilatations of said artery, which are greater than 1cm in diameter. Although the true prevalence of this entity is unknown and approximately 90% of these cases are asymptomatic, it is undoubtedly significant since it accounts for 60% of digestive arterial aneurysms.1
Clinical caseThis is the report of the case of a clinically asymptomatic 40-year-old woman patient who was diagnosed with splenic artery aneurysm. This was incidentally discovered during a routine check-up conducted by her primary care physician.
Upon examination, there was no abdominal pain, and no tumours or megalies were felt. She was referred to the interventionist radiology service for her therapeutic assessment. Upon catheterisation of the splenic artery and conduction of a three-dimensional angiographic study, a maximum fusiform dilatation of 23mm in diameter (Fig. 1) was confirmed. Thus, the possibility of embolisation was rejected.
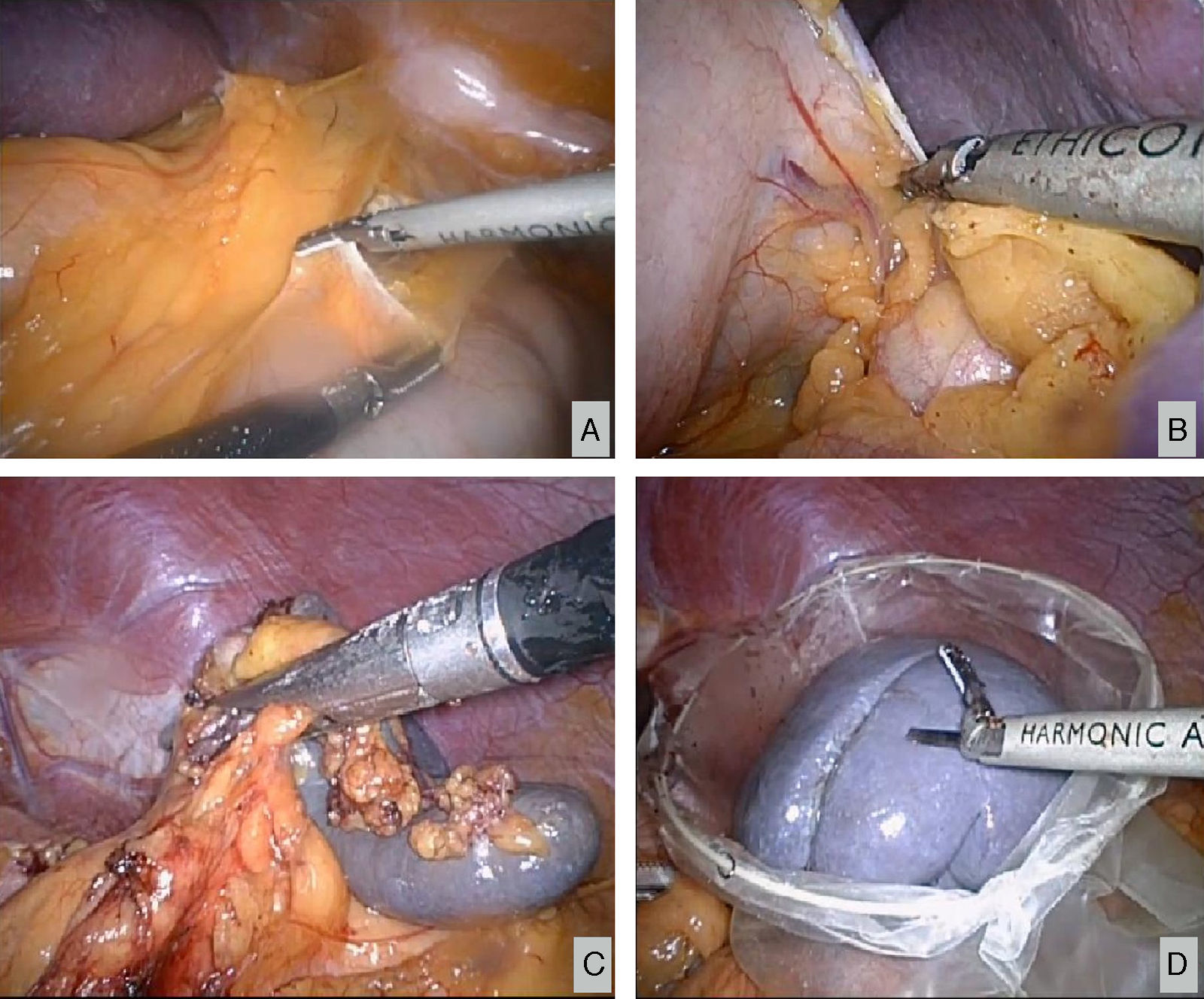
It was decided to perform a laparoscopic splenoaneurysmectomy (Fig. 2). For that purpose, a Hasson trocar was placed at the umbilical level and two 5 and 12mm trocars were inserted in a subcostal position, with the cleavage of the splenic angle and the opening of the epiploic transcavity (Fig. 2A), the placement of 2 metallic clips on the splenic artery in a position proximal to the aneurysm, and the section of short gastric vessels (Fig. 2B). Finally, the section of the splenic pedicle was conducted using an Endo GIA stapler with vascular load, and the surgical piece was extracted and placed in a bag (Fig. 2C and D).
There were no events during the post-surgical period, and the patient showed oral tolerance the same day during the afternoon. The patient was released from the hospital after 3 days.
DiscussionMost splenic artery aneurysms are asymptomatic or present non-specific symptoms (abdominal pain, anorexia, nausea, vomiting, etc.), so they are diagnosed by chance during the performance of imaging tests.1,2
Nevertheless, it must not be underestimated that about 2–10% of aneurysms begin with spontaneous rupture.3 In these cases, patients present acute pain in the epigastrium, left hypochondrium, left shoulder (Kehr's sign) and haemodynamic instability. The haemorrhage may stop in the epiplonic transcavity or move from Winslow's hiatus to the peritoneal cavity, which results in shock (“double rupture” phenomenon). In some cases, the splenic vein rupture results in arteriovenous fistula and portal hypertension.4,5 Thus, a high-output arteriovenous fistula may produce the “mesenteric steal syndrome”, which results in small intestine ischaemia.
Therefore, the treatment is indicated in symptomatic aneurysms or aneurysms with rupture risk factors, aneurysms greater than 2cm in diameter, pseudoaneurysms,6 portal hypertension, portocaval shunt, pregnancy, medial arterial fibrodysplasia or atherosclerosis.
In the rest of the cases, the progression of the disease must be strictly monitored by means of regular check-ups involving a computed tomography or an ecosonography every 6–12 months.
If an active therapeutic approach is adopted, the digital angiography3,4,7 or the multi-cut computed tomography7,8 must be assessed for the precise location of the aneurysm and exclude other visceral aneurysms. In this case, there are several therapeutic options, such as embolisation, endovascular stent placement or surgery.
Embolisation is considered the first line of treatment for asymptomatic aneurysms9,10 in patients with surgical difficulties or for pseudoaneurysms.6,11 It is contraindicated in splenic hilum aneurysms or arterial tortuosity cases.12
Endovascular stents are aimed at excluding the aneurysmal arterial segment, which allows for a non-turbulent blood flow. Therefore, these stents are the primary indication in pseudoaneurysms with layer rupture.9 Unlike embolisation, stents have a lower risk of splenic infarction and are preferred when arterial access to the spleen is required for the treatment of hypersplenism.
Although the indications of each procedure are currently under review,13–15 it is considered that the size of the aneurysm and the arterial tortuosity are limiting factors for embolisation and stent placement. In these cases, surgery is preferred. This depends on the location of the aneurysm in the course of the splenic artery.16,17 If it is located in the proximal third, an aneurysmectomy will be conducted; if it is located in the medial third, aneurysmal exclusion is preferred; and, if it is located in the distal third, a splenoaneurysmectomy will be carried out.
The aneurysmectomy consists on the ligature of the splenic artery proximally and distally to the aneurysm. Afterwards, the aneurysm is resected. The vascularisation of the spleen continues through the short vessels of the stomach.
In aneurysms located in the medial third, the aneurysm is simple ligated in its proximal and distal ends, thus resulting in aneurysmal exclusion. In the distal third of the splenic artery and splenic hilum, a splenoaneurysmectomy must be conducted. This consists of the resection of the spleen and the aneurysm from its hilum, as it occurred with the above-mentioned patient.
ConclusionThis report describes the case of an asymptomatic splenic artery aneurysm for which surgical treatment was indicated. The procedure for the therapeutic approach of this pathology is currently under review. Although it seems that embolisation would be the procedure of choice for asymptomatic cases, the size of the aneurysm and the arterial tortuosity are limiting factors for vascular access.
Moreover, we want to highlight the laparoscopic approach as a minimally invasive procedure of choice for the surgery of the splenic artery aneurysm.
Conflict of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: Colsa-Gutiérrez P, Kharazmi-Taghavi M, Sosa-Medina RD, Gutiérrez-Cabezas JM, Ingelmo-Setién A. Aneurisma de arteria esplénica. A propósito de un caso. Cir Cir. 2015; 83: 161–164.