Benign multicystic mesothelioma is a rare benign tumour derived from the peritoneal mesothelium.
The aim of this paper is to present a case of this rare tumour and review the clinical features, diagnosis and treatment of this disease.
Clinical caseThe case is presented of a 22-year-old female diagnosed with multicystic mesothelioma after an urgent resection of intra-abdominal tumour in the context of acute abdominal pain. In the subsequent follow-up, the patient had a recurrence of the lesion, and at 2 years was treated by further resection.
ConclusionsBenign multicystic mesothelioma is a benign tumour of unknown origin, and with a non-specific clinical manifestation. The most effective treatment is surgical, although there is a high tendency to local recurrence.
El mesotelioma multiquístico benigno es un tumor benigno infrecuente, que deriva del mesotelio peritoneal.
El objetivo del trabajo es presentar un caso clínico de esta rara entidad y realizar una revisión de la presentación clínica, diagnóstico y tratamiento.
Caso clínicoPaciente mujer de 22 años, que se diagnostica de mesotelioma multiquístico tras una resección urgente de una tumoración intraabdominal, en el contexto de un dolor abdominal agudo. En el seguimiento posterior presentó una recidiva de la lesión a los 2 años, que se trató mediante resección.
ConclusiónEl mesotelioma multiquístico benigno es un tumor benigno cuya etiología es desconocida, la manifestación clínica es inespecífica. El tratamiento más eficaz es quirúrgico, aunque presenta gran tendencia a la recidiva local.
Benign multicystic mesothelioma is a rare benign tumour, characterised by the formation of intra-abdominal multilocular cystic masses and its main structure arises from the peritoneal mesothelium. It is a rare disease, first described in 1979 by Doctors Mennemeyer and Smith, who established its mesothelial origin.1
The aetiology of the entity is not known and its most common form of presentation is in women of child-bearing age.
The clinical manifestation is non-specific, abdominal pain is usual and the presence of a palpable mass.2–4 Occasionally it presents as an incidental finding during a diagnostic test or surgical intervention.
The most effective treatment is surgery, although there is a high tendency for local recurrence.2,4
The aim of this study is to present a clinical case of this rare disorder and to review the clinical presentation, diagnosis and treatment of the disease.
Clinical caseA 22-year-old woman, with no medical or surgical history of interest, attended the emergency department with symptoms of acute abdominal pain in the right iliac fossa. She reported no other associated symptoms. The physical examination found abdominal pain and guarding with mass effect at the level of the right iliac fossa. The laboratory tests showed no disturbances. Abdominal ultrasound was performed, complemented by abdomino-pelvic CT scan for better assessment which radiologically described thickening of the right lateroconal and posterior pararenal fascia and an encapsulated collection with peripheral enhancement of 36.7mm×92.2mm, displacing the caecum medially. These findings were suggestive of an abscess caused by retrocaecal appendicitis (Fig. 1).
Since a complicated appendicitis was suspected, an urgent exploratory laparotomy was performed. We used a 12mm umbilical trocar, a 10mm suprapubic trocar and 5mm trocar in the left iliac fossa. The findings showed a cystic tumour below the lateral peritoneum of the right colon, adjacent to the caecum. The patient presented a normal caecal appendix with pelvic arrangement; no visible disturbances of uterus and uterine annexes.
The cystic tumour of the right lateral colon wall was dissected; we observed that it had a cleavage plane with respect to the colon and was removed in one piece in a bag. An appendectomy was performed and a drain placed in the surgical bed.
The patient progressed well clinically in the post-operative period and was discharged on the third post-operative day.
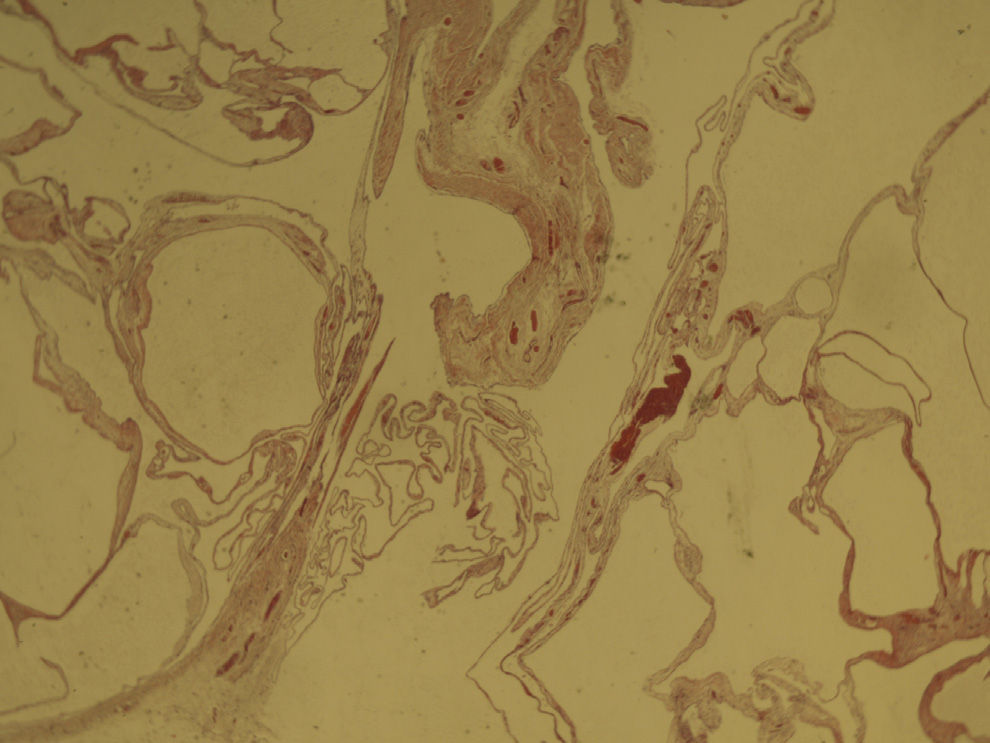
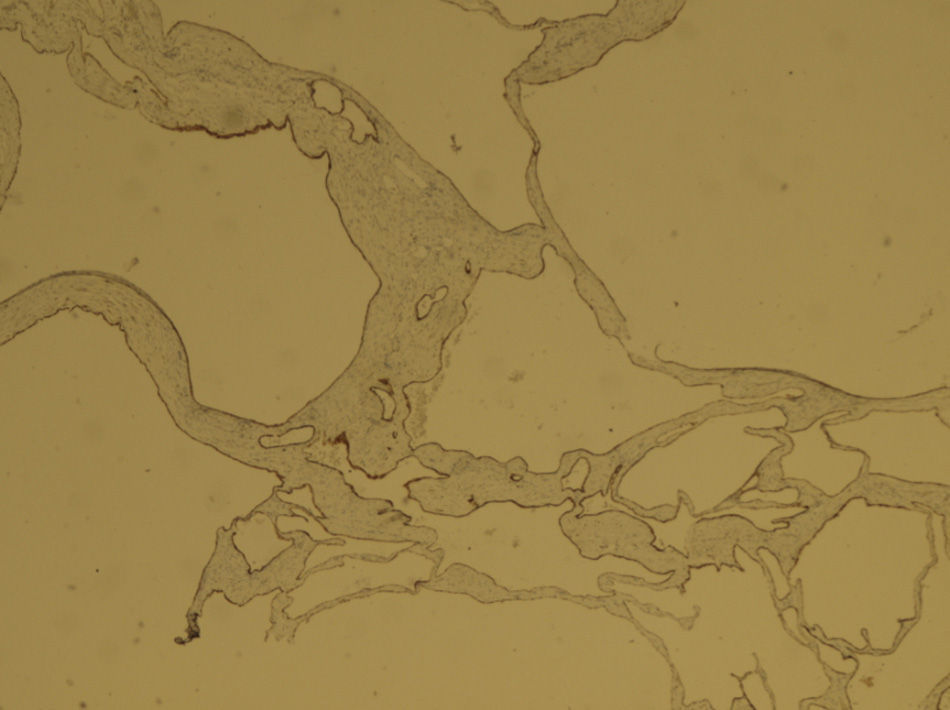
The patient was followed up in the surgery 3 weeks later and the pathology report found an irregular fragment of polycystic appearance, 4cm in diameter, with findings compatible with benign multicystic mesothelioma, with wide areas of mesothelial coverage and deposits of fibrin and thrombus, and foci of haematic extravasation. There was no associated inflammation of the caecal appendix.
A pancolonoscopy was performed and described as normal.
An abdominopelvic CT scan was performed, showing no signs of recurrence, and follow up by CT scan at one year was arranged.
The follow-up CT scan at one year showed no signs of recurrence. However, the subsequent CT follow-up (2 years after removal of the tumour) revealed a small ovoid structure in contact with the posterior wall of the ascending colon, with fluid attenuation, approximately 33.5mm in diameter, suggestive of recurrence of the tumour (Fig. 2).
The patient was scheduled for laparoscopic surgery and the findings revealed an extracolonic cystic tumour on the right parietocolic gutter. The tumour was resected and completely removed in a bag.
The post-operative period was uneventful and the patient was discharged 3 days after surgery.
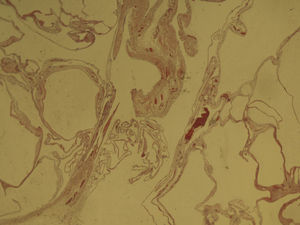
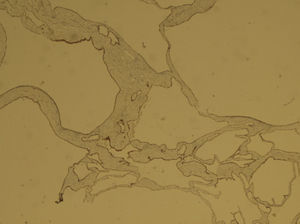
The patient was followed up as an outpatient. At 3 weeks post surgery, the pathology report gave a macroscopic description: fragment of adipose laminar tissue, measuring 3cm×3cm, presenting an elevated nodule with a maximum diameter of 2cm, multiloculated on cut section. The microscopic description indicated a mass formed by multiple cysts lined with a single layer of cubic or flattened cells, of basal nuclei, whose wall comprised a fibro adipose stroma with mild vascular congestion and foci of chronic and non-specific inflammatory changes (Fig. 3). There were no cell proliferations or atypias. The cells lining the cystic cavities presented positive immunophenotype for cytokeratins AE1-E3 and calretinin (Fig. 4), which demonstrate the primary mesothelial origin of the tumour. Conclusion: recurrence of benign multicystic peritoneal mesothelioma.
Cystic peritoneal mesothelioma is a lesion of unknown aetiology. It was first described in 1979 by Doctors Mennemeyer and Smith,1 who established its mesothelial origin using an electronic microscope, as previously it had been labelled cystic lymphangioma. Some authors claim that it is a benign neoplastic tumour, while others interpret it as a peritoneal lesion secondary to intra-abdominal inflammation, previous abdominal surgery, endometriosis and pelvic inflammatory disease.2
It presents principally in women of child-bearing age, which indicates the possible relevance of female sex hormones in the etiopathogenesis of this disorder.3
The clinical signs are non-specific and abdominal pain, palpable mass2–4 and symptoms due to compression of the abdominal organs are usual. In many cases it is asymptomatic and is an incidental finding during a radiological test or surgical intervention.3,4
The diagnosis is approached by ultrasound and abdomino-pelvic CT scan, which shows multiloculated cystic tumours, not dependent on the abdominal organs. Laparoscopy remains the most precise diagnostic tool.4 In our case, initial exploratory laparoscopy revealed an extracolonic multicystic lesion with a normal appendix, while the radiological tests indicated complex appendicular disease.
Differential diagnosis of peritoneal cystic mesothelioma is established with benign lesions such as: cystic lymphangioma, endosalpingiosis, endometriosis, retroperitoneal cysts of Müllerian type and adenomatoid tumours2–4 and with malignant lesions such as: malignant mesothelioma and clear cell ovarian carcinoma.
Macroscopically, the appearance of the lesion is typical with multiple cysts of different sizes with serous or serosanguineous content and dispersed across the peritoneal surface.
The cysts are distinguished microscopically because they are lined with mesothelial cells with vascular stroma, with acute and chronic inflammatory infiltrate, and areas of squamous metaplasia. Mesothelial cells are immunohistochemically positive for calretinin and are occasionally oestrogen and progesterone receptor positive.3
One case has been reported of the malignant transformation of a cystic mesothelioma.5
The only effective treatment is surgery; complete removal of the lesions and follow-up is essential, as recurrence rates of up to 50% have been reported.2 For this reason, new adjuvant treatments have been tested such as pelvic peritoneal sclerosis with a solution of 1% tetracycline, hyperthermic peritoneal perfusion with cisplatin6 and even peritonectomy with adjuvant intraperitoneal chemotherapy.7 The detection of oestrogen and progesterone hormone receptors in some tumours2 has led some authors to use hormone therapy with gonadotropin-releasing hormone agonists and anti-oestrogenic agents, such as tamoxifen,8 to treat and prevent recurrence of the disease.
ConclusionAfter reviewing the literature with regard to this very rare condition, we conclude that the treatment of choice is surgery to remove all visible lesions. Tetracycline sclerosis and hormone therapy are indicated only if multiple recurrences are detected. Intraperitoneal infusion of chemotherapy agents and peritonectomy are indicated for cases of more serious multiple recurrence.
Neither the size of the cysts nor the extension of the lesion appear to influence prognosis.2 The fundamental problem is recurrence which, according to the literature review, can reach 50%.2 Only one case of malignant transformation has been reported,5 in a case with multiple recurrences.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: García-Mayor Fernández RL, Fernández-González M, López-Rodríguez A, Martínez-Almeida Fernández R. Mesotelioma multiquístico peritoneal benigno recidivante: abordaje de esta entidad tan poco frecuente. Cir Cir. 2016;84:499–502.