Shoulder arthroscopy is the standard technique for performing procedures involving the intertubercular groove. Current techniques continue to produce excessive soft tissue manipulation and neurovascular injury.
Materials and methodsA cross-sectional, observational and descriptive study was conducted on a cohort of 24 shoulders following the standard surgical protocol and using punch dissection. The neurovascular structures with risk of damage by the standard lateral portal were evaluated during the study to establish a secure area for a new arthroscopic portal. Finally, the safety of the new proposed site was evaluated.
ResultsThe presence of 24 venous structures, with a mean diameter was 1.05mm (SD: 0.71) was documented. A tendency was observed in locating these structures in the lower half of the dissecting field for the left shoulders and a hypovascular area between the 7 and 10h circle dissected relative to the right shoulder. The new site was determined at a point 1.5cm anterolateral to the anterolateral border of the acromion at an angle of 60° to the horizontal axis of the acromion and towards the intertubercular groove of the humerus.
ConclusionsThe methodology used in this study is innovative, reproducible and applicable for the study of all existing shoulder arthroscopic portals procedures, as well as any joint. The results provided by this study will be helpful for clinicians to improve tenotomy/tendon tenodesis procedures of the long head of the biceps brachii tendon.
La artroscopia de hombro constituye la técnica de elección para los procedimientos que involucran el surco intertuberositario. Las técnicas actuales continúan produciendo una manipulación excesiva de tejidos blandos y daño a estructuras neurovasculares.
Materiales y métodosEstudio cohorte trasversal, observacional y descriptivo. Se evaluaron 24 hombros, siguiendo el protocolo quirúrgico estándar y utilizando disección en sacabocado. Durante el estudio se evaluaron las estructuras neurovasculares en riesgo próximas al portal lateral estándar, para establecer un área segura en base a la cual se estableció el nuevo portal artroscópico. Por último, se evaluó la seguridad del nuevo portal.
ResultadosDocumentamos la presencia de 24 estructuras venosas próximas al portal lateral estándar, cuyo diámetro promedio fue de 1.05mm±0.71. Se observó una tendencia a localizar estas estructuras en la mitad inferior del campo de disección para hombros izquierdos, así como un área hipovascular entre las 7 y las 10h respecto al círculo disecado, para los hombros derechos. El nuevo portal se determinó en un punto localizado 1.5cm anterolateral al borde anterolateral del acromion con una angulación de 60° respecto al eje horizontal del acromion y en dirección al surco intertuberositario del húmero.
ConclusionesLa metodología utilizada en el presente estudio es innovadora, reproducible y aplicable para el estudio de todos los portales artroscópicos existentes en el hombro y en general en cualquier articulación. Los resultados proporcionados por este estudio serán de ayuda para el clínico, para mejorar los procedimientos de tenotomía/tenodesis del tendón de la cabeza larga del músculo bíceps braquial.
In recent years shoulder arthroscopy has become the technique of choice for surgical procedures to the shoulder.1 Its results in the treatment of shoulder instability and rotator cuff injury are comparable to open procedures, but with far lower morbimortality.2
The prevalence of injuries to the long head of the biceps brachii tendon is estimated at 25 cases per 100,000 inhabitants in the general population.3 This prevalence is higher in people of the third age, and medium and high performing athletes.3 Recent studies estimate that it will increase in years to come, due to the demographic transition taking place in the Western world.3
The long head of the biceps brachii tendon is often the source of shoulder pain, due to the great variety of pathological changes that can affect it.4–6 Surgical treatment of these conditions can be limited to the surgical removal of the intra-articular portion of the tendon (tenotomy), followed or otherwise by its reinsertion using different materials to another portion of bone, usually in the intertubercular groove of the humerus (tenodesis).6–8 This technique is currently the subject of debate amongst orthopaedic surgeons worldwide.9
Techniques with the current minimally invasive portals, for performing tenotomy/tenodesis procedures on the long head of the biceps brachii tendon continue to involve excessive manipulation of the soft tissues and are frequently a cause of local and regional complications to the area. No portal has been described as yet which fulfils the characteristics of visualisation, safety and access to the intertubercular groove. A new arthroscopic portal is required which will enable precise visualisation of the long head of the biceps brachii tendon in the intertubercular groove of the humerus; this would minimise the dissection of soft tissues during these procedures on the long head of the biceps brachii tendon.
The objective of this study was to anatomically determine a new potential arthroscopic portal, in order to perform tenotomy/tenodesis procedures to the long head of the biceps brachii tendon, as well as other procedures involving this area.
Material and methodsAn anatomical, observational, cross-sectional, descriptive and non-comparative study was undertaken, in which 24 shoulders of male cadavers from the Mexican population were dissected. The cadavers had been embalmed beforehand and belonged to the Human Anatomy Department of the Faculty of Medicine of the Universidad Autónoma de Nuevo León. The cadavers’ ages ranged between 18 and 70 (mean 40.4±9.12), their weights were between 52.40 and 96.00kg (mean 69.54±13.6kg), heights between 1.52 and 1.89m (mean 1.67±0.22m) and body mass index between 19.21 and 32.37kg/m2 (mean of 24.88±3.88kg/m2).
Three groups were made, with 8 shoulders in each. The sample size was established by hypothesis testing and the difference of 2 means or with the mean of a reference value, with a zα value of 1.96, two-sided 95% significance level, and a zβ value of 0.84 with a power of 80%; a sample of 8 units was obtained per group, expecting to find a safety of at least 9mm higher compared to the conventional arthroscopic portal, the standard lateral portal.
This study was divided into 3 phases; phase 1 consisted of anatomically evaluating the standard lateral portal and establishing a “safe area” next to it. The new arthroscopic portal was established in phase 2 based on the abovementioned “safe area” and validated by direct arthroscopic visualisation of the tendon. Finally, in phase 3, an analysis was made of the neurovascular structures at risk close to the new suggested portal, using the same methodology as phase 1.
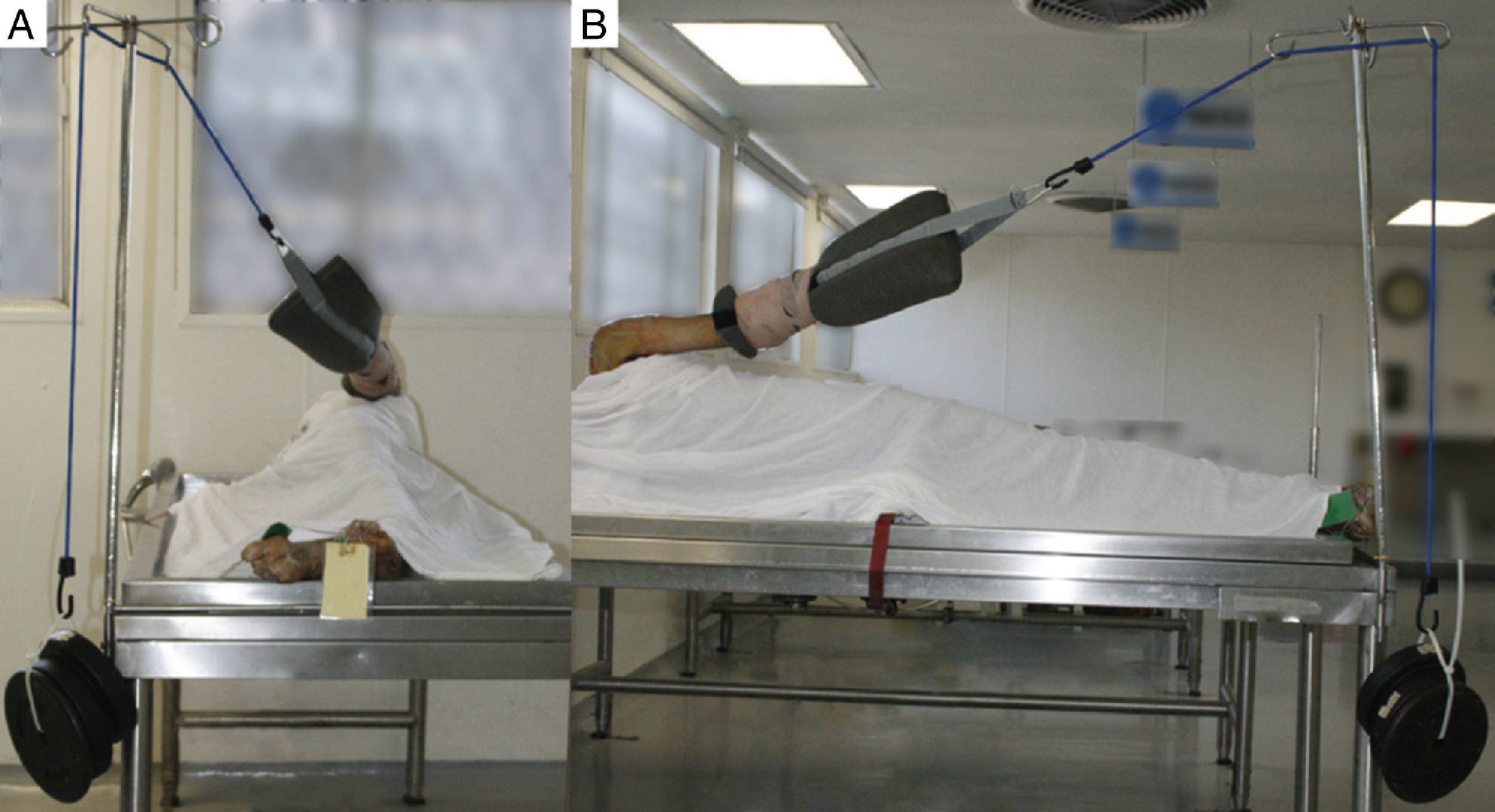
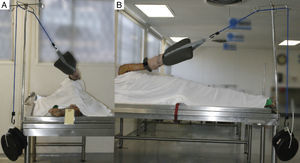
For phase 1, the standard protocol was followed for positioning the cadaver, and for locating, positioning and placing the portals. The cadaver was positioned in the lateral position; the upper limb was placed in abduction at 15° with posterior inclination of 30° and traction applied in a podalic direction (inferior) with a weight of 9.71kg (20 pounds) (Fig. 1).
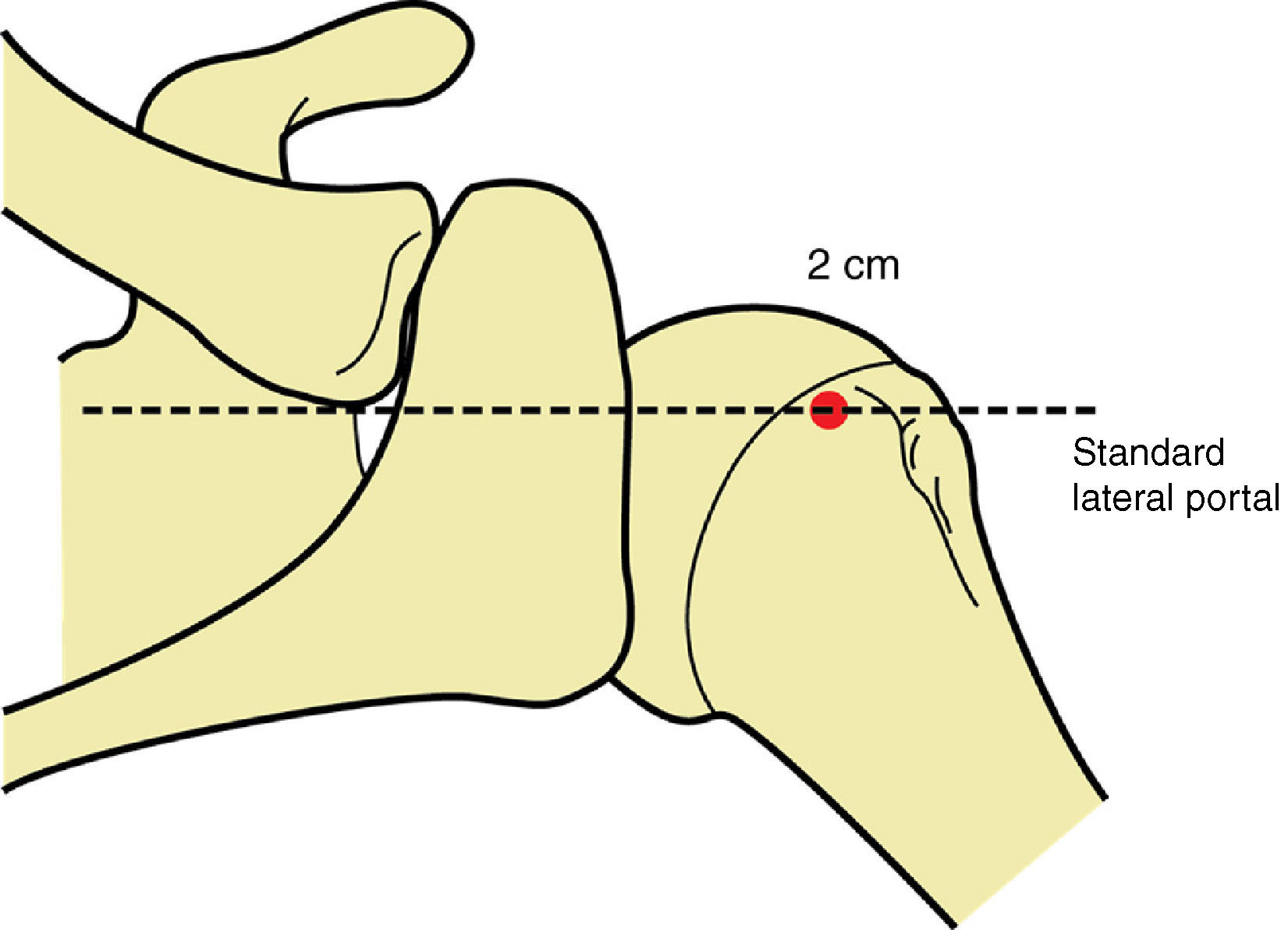
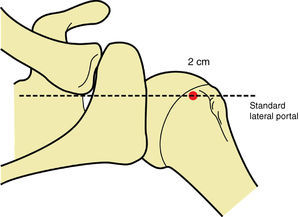
Subsequently the bone references of the acromion, clavicle and acromioclavicular joint were identified and marked using a surgical marker, in order to use them as a reference point for placing the standard lateral portal, which was placed introducing the trocar (Linvatec T4930, 4mm in diameter) in a point located 2cm lateral to the lateral margin of the acromion, aligned with the posterior margin of the clavicle (Fig. 2).1,2,10
Then punch dissections were made (this is an original dissection technique designed by the authors), as this method enables a better connection to be established in situ between the route of the portal and the neurovascular structure which is at risk of injury. This technique consists of dissecting each anatomical plane, within a circumference with a radius of 2.5, taking the trocar as the central point. As the dissections were being made the risk was assessed of injuring any neurovascular structure in all the anatomical planes dissected, until visualising the greater tubercle of the humerus.
The following morphometric characteristics were established for each neurovascular structure found: the diameter of each structure, location in the dissection circle, distance to the trocar (punch) and anatomical plane (topography), where this structure was found.
Each measurement was made by 2 people independently, blinded from each other, using a digital millimetre vernier with 0.01mm precision (Mitutoyo Digimatic Encoders w/Series 500). The position of each neurovascular structure found was documented by standardised photographs of each portal (Nikon D 3200 24 megapixel digital camera), which were digitalised using Adobe Illustrator CS6 for Mac OS10.6. Once they were digitalised, each anatomical plane was superimposed to identify areas at risk with a greater presence of neurovascular structures close to the trocar, as well as areas of safety.
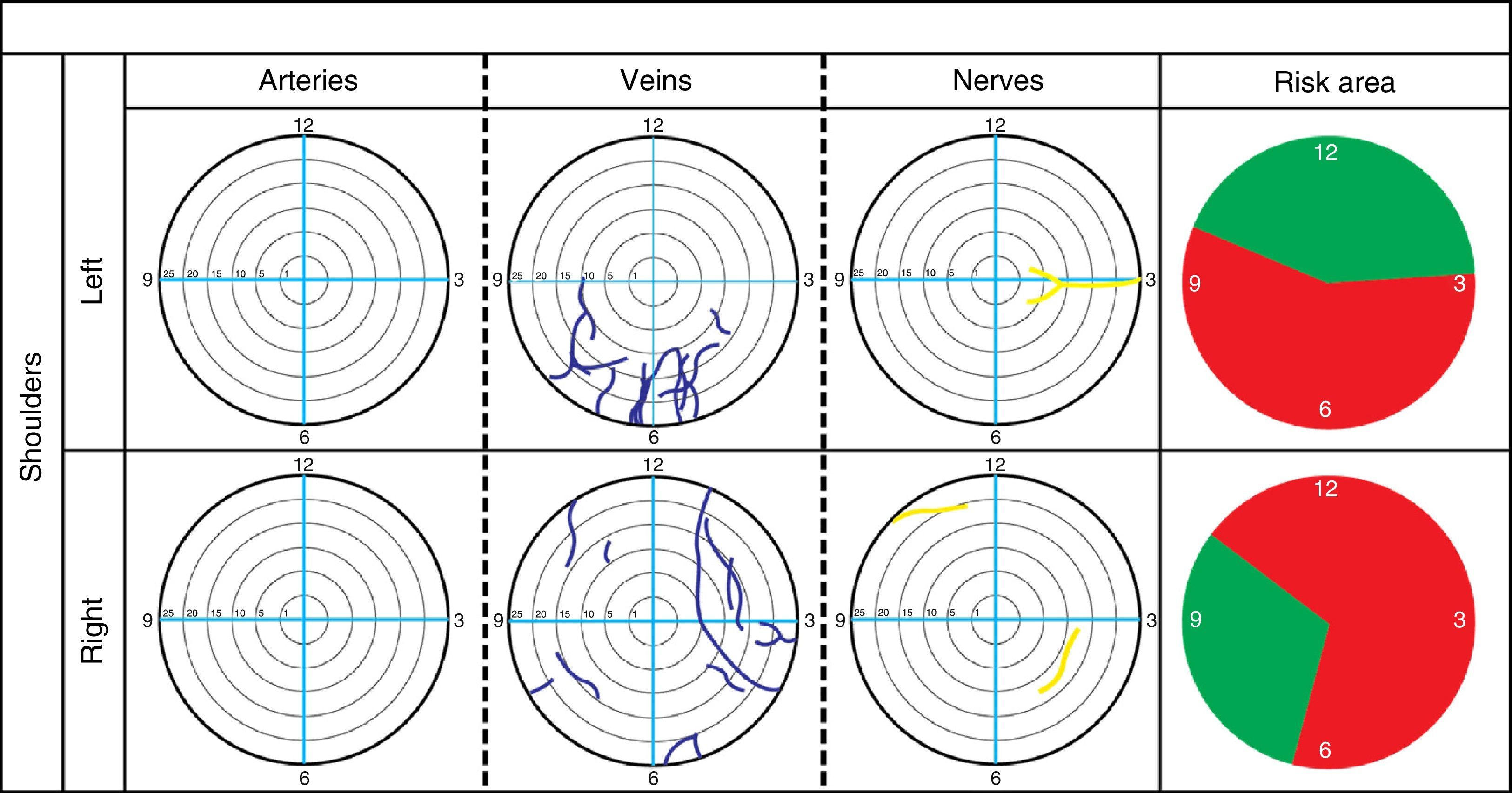
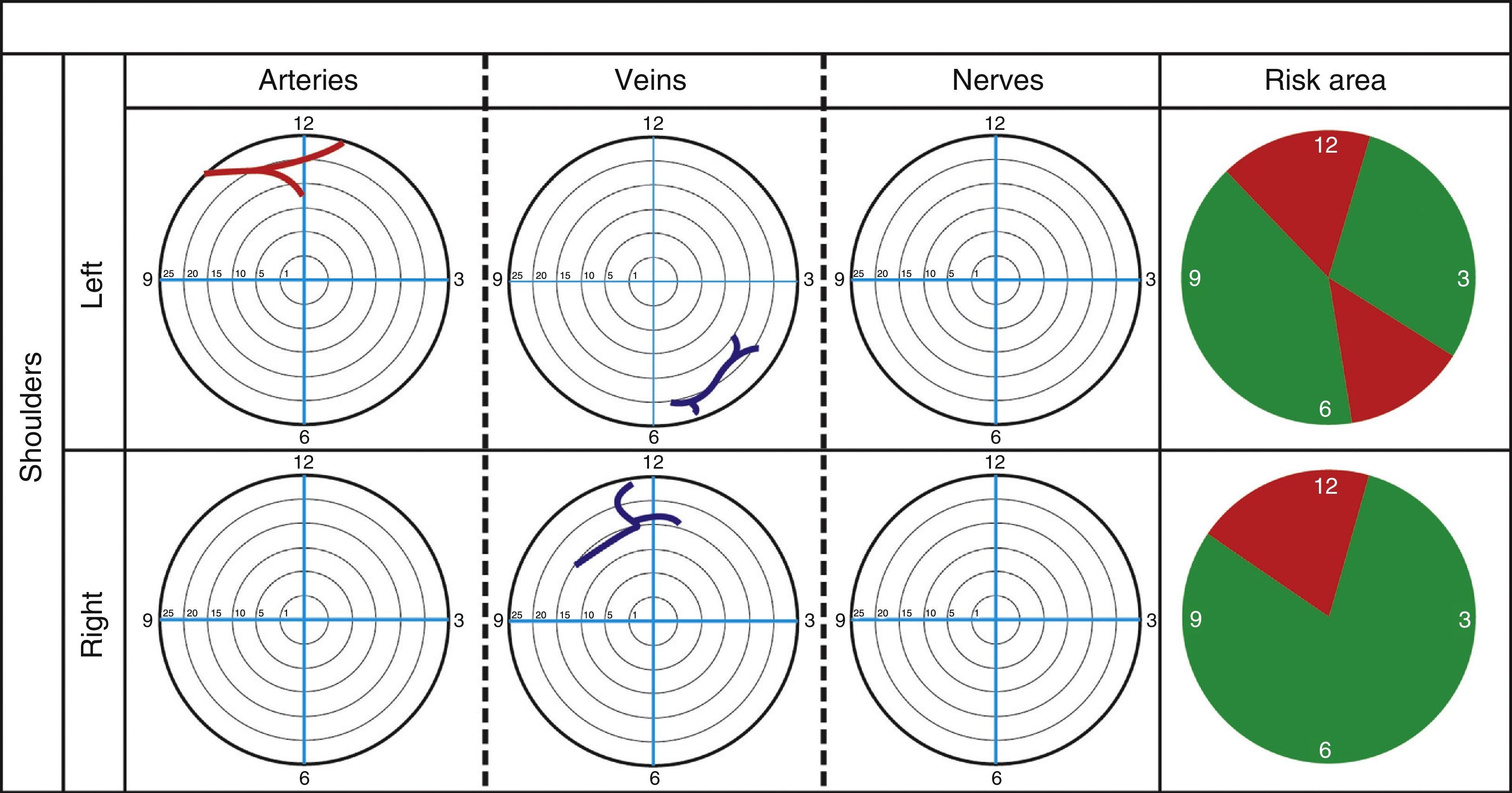
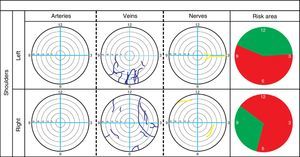
The neurovascular structures found were inside a circumference which represented the punch dissection. A system was used where each neurovascular structure was located inside a clock-hand position, where 12 o’clock represented the upper extreme, 6 o’clock the lower extreme and 3 o’clock and 9 o’clock the anterior and posterior extremes for right shoulders and the posterior and anterior extremes for left shoulders. The arterial, venous and nervous structures were represented, found during the punch dissections; these were also represented using a system of colours, red for the area of risk, and green for the safe area.
Because the standard lateral portal is the most common lateral arthroscopic approach in the lateral region of the shoulder, we decided to use it as the starting point for making the new portal. The new arthroscopic portal was determined according to the safe area established in phase 1, taking into account the anatomy of the deltoid region, the traditional description of the location of the axillary nerve and the anterior and posterior humeral circumflex vessels, along with the anatomical variants reported in them, with regard to their original pattern and description and the approach angle of the intertubercular groove of the humerus, by arthroscopy and correct visualisation of the tendon.
The safety of the new proposed portal was analysed, using the abovementioned methodology for evaluating the standard lateral portal.
Statistical analysisMicrosoft Excel 2010 for Windows XP was used to establish the mean and the standard deviation for each measurement parameter. Parametric correlation tests (Student's t-test) were used to compare the average values obtained from the measurements made by the 2 observers (intraobserver variability) with regard to the distance to the trocar of each structure found and their diameter, a p value of <05 was considered significant.
Ethical considerationsThis research protocol was approved by the Ethics Committee and Research Committee of the Faculty of Medicine of the Universidad Autónoma de Nuevo León, with registration number AH14-002.
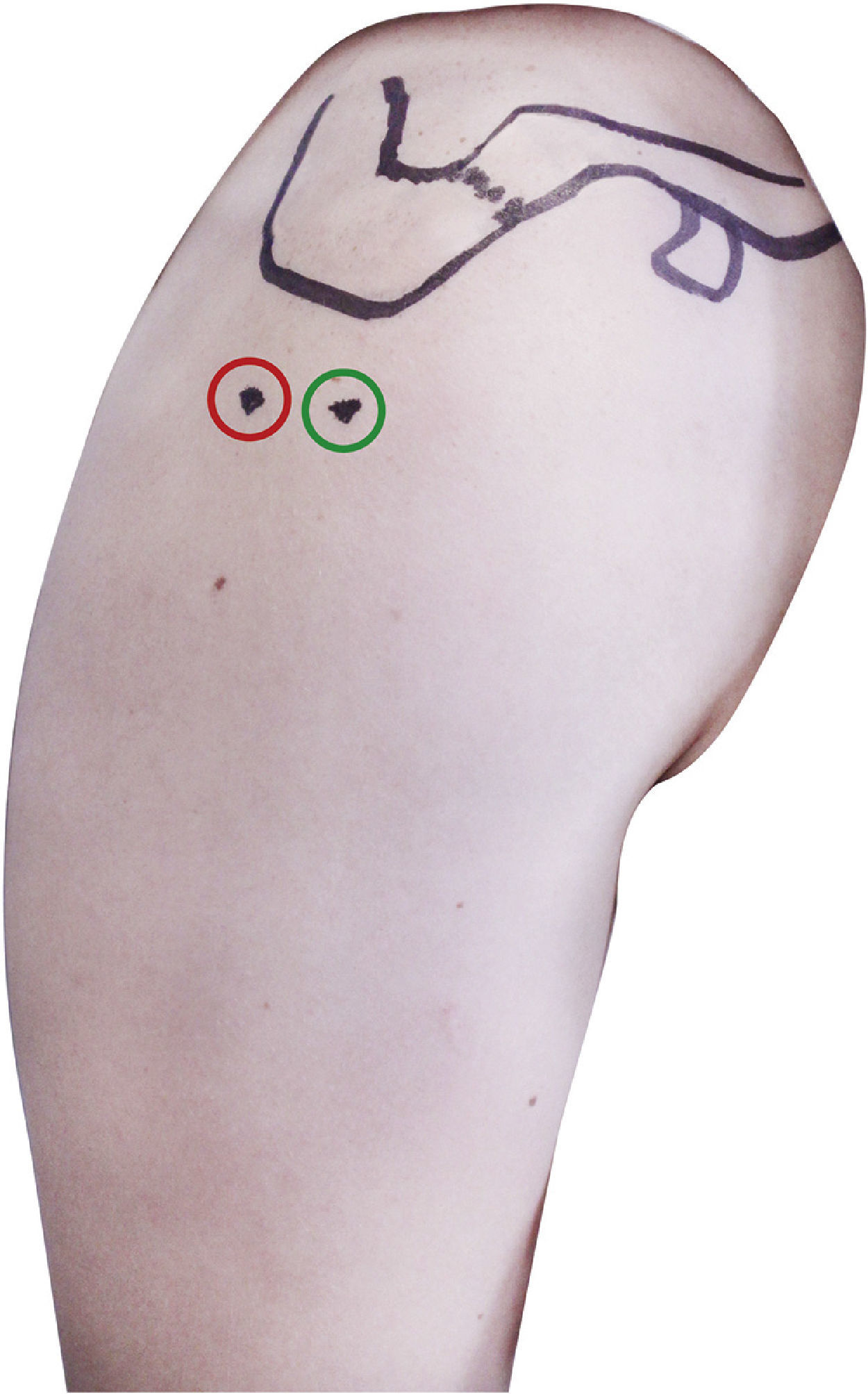
ResultsThe new portal was established at a point located 1.5cm anterolateral to the anterolateral edge of the acromion at an angle of 60° to the horizontal axis of the acromion and in the direction of the intertubercular groove of the humerus (Fig. 3).
This location was decided based on a hypovascular area next to the standard lateral portal.
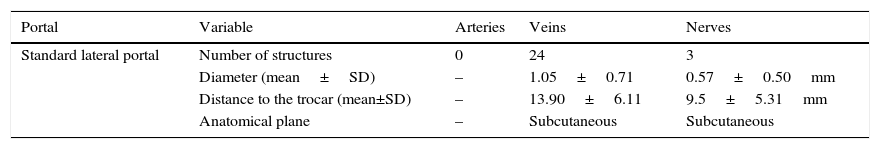
During the evaluation of safety areas close to the standard lateral portal no arterial structures at risk were reported in the dissections of the lateral portals. We documented the presence of 24 venous structures with a diameter in a range between 0.31 and 3.7mm with an average of 1.05±0.71mm (Table 1). The distance to the punch was in range between 3.49 and 23.74mm, with an average of 13.90±6.11mm (Table 1). A tendency was observed for these structures to be located in the lower middle of the dissection field for the left shoulders and a hypovascular area between 7 and 10 o’clock in the dissected circle for the right shoulders (Fig. 4). We found 58.33% of these structures in the subcutaneous plane.
Evaluation of the standard lateral portal. Neurovascular structures at risk in the standard lateral portal.
| Portal | Variable | Arteries | Veins | Nerves |
|---|---|---|---|---|
| Standard lateral portal | Number of structures | 0 | 24 | 3 |
| Diameter (mean±SD) | – | 1.05±0.71 | 0.57±0.50mm | |
| Distance to the trocar (mean±SD) | – | 13.90±6.11 | 9.5±5.31mm | |
| Anatomical plane | – | Subcutaneous | Subcutaneous |
The mean and standard deviation were determined for each variable evaluated. Note the appearance of 24 venous structures and 3 nerve structures.
We documented the presence of 3 subcutaneous nerves of 0.61, 1.51 and 0.54mm in diameter respectively with an average of 0.57±0.50mm (Table 1). These structures were found at a distance of 13.88, 3.59 and 11.05mm respectively with an average of 9.5±5.31mm (Table 1). Two structures were located at 3 o’clock in the dissection circle while the other was located between 11 o’clock and 12 o’clock (Fig. 4). These structures were situated topographically in the subcutaneous cell tissue and were probably branches of the lateral superior brachial cutaneous nerve coming from the axillary nerve.
No significant differences were found on comparing the average results of the morphometrics performed by the 2 observers in any of the parameters evaluated (the p values varied between 0.14 and 0.96).
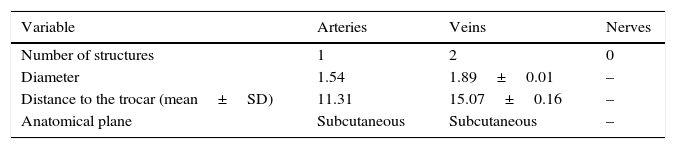
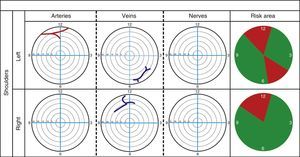
The presence of nerve structures in the proposed portal was not recorded. The presence of an arterial structure was documented in one left shoulder of 1.54mm in diameter at a distance of 11.31 from the centre of the portal, located in the subcutaneous plane (Table 2) and between 11 o’clock and 12 o’clock in the dissection circle (Fig. 5). Similarly, 2 veins were found (one in a left shoulder and one in a right shoulder) with an average diameter of 1.89±0.01mm and an average distance to the trocar of 15.07±0.16mm; located in the subcutaneous plane (Table 2). One of the veins was found between 10 o’clock and 12 o’clock in the dissection circle and the other between 4 o’clock and 6 o’clock. In the 8 shoulders destined for phase 3 of the study it was possible to visualise the intertubercular groove of the humerus, using the proposed approach.
Proposed arthroscopic portal. Neurovascular structures at risk in the proposed portal.
| Variable | Arteries | Veins | Nerves |
|---|---|---|---|
| Number of structures | 1 | 2 | 0 |
| Diameter | 1.54 | 1.89±0.01 | – |
| Distance to the trocar (mean±SD) | 11.31 | 15.07±0.16 | – |
| Anatomical plane | Subcutaneous | Subcutaneous | – |
The mean and standard deviation were determined for each variable evaluated.
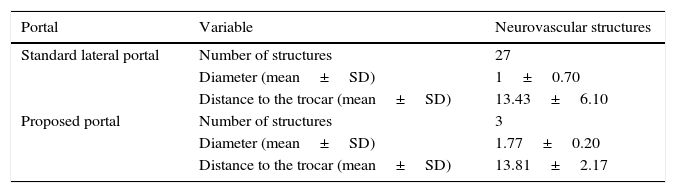
The comparison of structures at risk during the use of both portals is listed in Table 3.
Comparison of neurovascular structures at risk of injury in the standard lateral portal compared to the proposed portal.
| Portal | Variable | Neurovascular structures |
|---|---|---|
| Standard lateral portal | Number of structures | 27 |
| Diameter (mean±SD) | 1±0.70 | |
| Distance to the trocar (mean±SD) | 13.43±6.10 | |
| Proposed portal | Number of structures | 3 |
| Diameter (mean±SD) | 1.77±0.20 | |
| Distance to the trocar (mean±SD) | 13.81±2.17 |
The mean and standard deviation were determined for each variable evaluated. The mean distance to the trocar was greater than that expected of 9mm for the statistical analysis.
The purpose of an arthroscopic portal is to achieve excellent visualisation of the joint cavity and enable the surgeon to use instruments with minimal manipulation of the periarticular tissues.1 The relatively thick musculature of the shoulder girdle and the close proximity to vital neurovascular structures require the creation of safe and reproducible portals, which minimise the risk of injury to these structures.1
The standard lateral portal is used to access the subacromial space and to treat conditions there and as a portal for the visualisation of other arthroscopic portals.1 While this study was being performed, a great number of small calibre veins located near to this portal was recorded, which constitute venous tributaries of the anterior or posterior circumflex humeral vein. These veins are in charge of superficial and deep venous drainage of the deltoid muscle and the articular capsule of the glenohumeral joint.
No quantification of the small calibre structures when making a lateral approach has been reported in the literature. Altogether, these structures might cause intra-articular bleeding which makes visualisation difficult when making a lateral approach and this might have an effect on the clinical outcome. The comparison between the standard lateral portal and the portal proposed is shown in Table 3. If the portal proposed in this study is used the probability will be minimised of injury to venous structures, because they are located in a hypovascular area.
Anatomists have studied the anatomy, distribution and anatomical variants of the axillary nerve by dissection for years.1–14 However, in recent years, orthopaedic surgeons have shown great interest in the anatomy of the axillary nerve and the circumflex humeral vessels because these can become damaged during shoulder arthroscopies.15–18
The axillary nerve is the nerve structure that is most commonly damaged during surgical procedures to the shoulder and represents from 6% to 10% of brachial plexus injuries.19–22 Injuries to the axillary nerve result in atrophy of the deltoid muscle and the teres minor, lateral abduction and rotation deficit of the arm, hypaesthesia of a small area of skin lateral to the shoulder (through the superior lateral cutaneous nerve of the arm, branch of the axillary nerve).23
The axillary nerve also provides some branches to the articular capsule and the middle and lower glenohumeral ligament, which are determinants for the uptake of shoulder proprioception information.17 Open surgery and shoulder arthroscopy require the manipulation of capsular tissue and the glenohumeral ligaments, and these can incur micro injuries during the procedure. These injuries might not entail a clinically remarkable motor or sensory deficit, but they could seriously affect the proprioceptive sensitivity of the shoulder region.24
Murthi et al.25 mentioned that it is not easy to identify injuries of the long head of the biceps brachii tendon by arthroscopic visualisation, because only 50% are visible macroscopically. Even so, diagnostic arthroscopy remains the most sensitive and specific evaluation method, for assessing the great diversity of conditions that can affect this structure.26 Therefore, improving visualisation of this tendon using the new arthroscopic portal proposed in this study might increase the sensitivity and specificity of diagnosis of these injuries and detect subtle macroscopic changes such as hyperaemia of the tendon.
In general, the arthroscopic portal proposed in this study is intended to provide the orthopaedic surgeon with a safer option for approaching the long head of the biceps brachii tendon and its neighbouring structures.
ConclusionsA safety area was identified for the standard lateral portal between 10 o’clock and 2 o’clock for left shoulders, and between 7 o’clock and 10 o’clock for right shoulders. Based on this safety area, the new portal was established at a point located 1.5cm anterolateral to the anterolateral edge of the acromion, at an angle of 60° to the horizontal axis of the acromion and towards the intertubercular groove of the humerus.
The safety of the new proposed portal was validated because the mean distance of vascular structures to the portal was 13.81±2.17mm, which is greater than the expected safety distance >9mm, compared to the standard lateral portal. Nine times fewer neurovascular structures were found in the proposed portal than in the standard lateral portal.
Conflict of interestsThere were no financial or commercial gains from this study; therefore the authors have no conflict of interest of any type to declare.
Please cite this article as: Gutiérrez-de la O J, Espinosa-Uribe AG, Morales-Avalos R, Vílchez-Cavazos F, Elizondo-Omaña RE, Guzmán-López S. Nuevo portal artroscópico para la realización de procedimientos de tenotomía/tenodesis del tendón de la cabeza larga del músculo bíceps braquial. Cirugía y Cirujanos. 2016;84:293–300.