Duodenal carcinoma is very rare. It represents 33–45% of the all tumours of the small bowel. The symptoms are non-specific, and the diagnosis is often accidental.
Clinical caseA 35-year-old man was admitted to our hospital with post-prandial abdominal pain. Upper gastrointestinal examination revealed a tumour of the third duodenal portion, which was diagnosed, using endoscopic biopsy, as a tubular adenoma with high grade dysplasia. The computed axial tomography scan, the magnetic resonance imaging, and the endoscopic ultrasound showed the neoplasia of the third duodenal portion with no lymph node or peritoneal metastases. Partial resection of the duodenum was performed. The definitive histopathological diagnosis was primary adenocarcinoma of the third duodenal portion. pT2 N0M0, originated in a tubular adenoma.
ConclusionsPrimitive neoplasia of the duodenum is very rare. Duodeno-cephalo-pancreatectomy is recommended in proximally located tumours, while segmental resection of the duodenum is appropriate for distal locations, with the same survival.
El adenocarcinoma de duodeno es un tumor poco frecuente; representa el 33-45% de todos los tumores de intestino delgado. Los síntomas no son específicos, y el diagnóstico con frecuencia es accidental.
Caso clínicoVarón de 35 años, que consulta por dolor abdominal posprandial. La endoscopia diagnosticó un tumor de la tercera porción duodenal (adenoma tubular con alto grado de displasia mediante la biopsia endoscópica). La tomografía computada, la resonancia magnética nuclear y la ecoendoscopia, mostraron un tumor de la tercera porción duodenal, sin metástasis linfáticas o peritoneales. Se realizó resección parcial del duodeno y el diagnóstico definitivo fue de adenocarcinoma de la tercera porción duodenal sobre adenoma tubular pT2N0M0.
ConclusionesLas neoplasias de duodeno son muy raras. La duodenopancreatectomía cefálica se recomienda para los tumores de localización proximal, mientras que las resecciones segmentarias son apropiadas para localizaciones distales, con la misma supervivencia.
Malign tumours of the small bowel are rare, and in the majority of patients they give rise to signs and symptoms that are not very specific, hindering diagnosis at early stages. They represent from 33% to 45% of small bowel tumours,1 and account for only 0.3–0.5% of all gastrointestinal neoplasias.
Although endoscopic treatments have been published for early stages,2 surgery is the treatment of choice for more advanced phases.
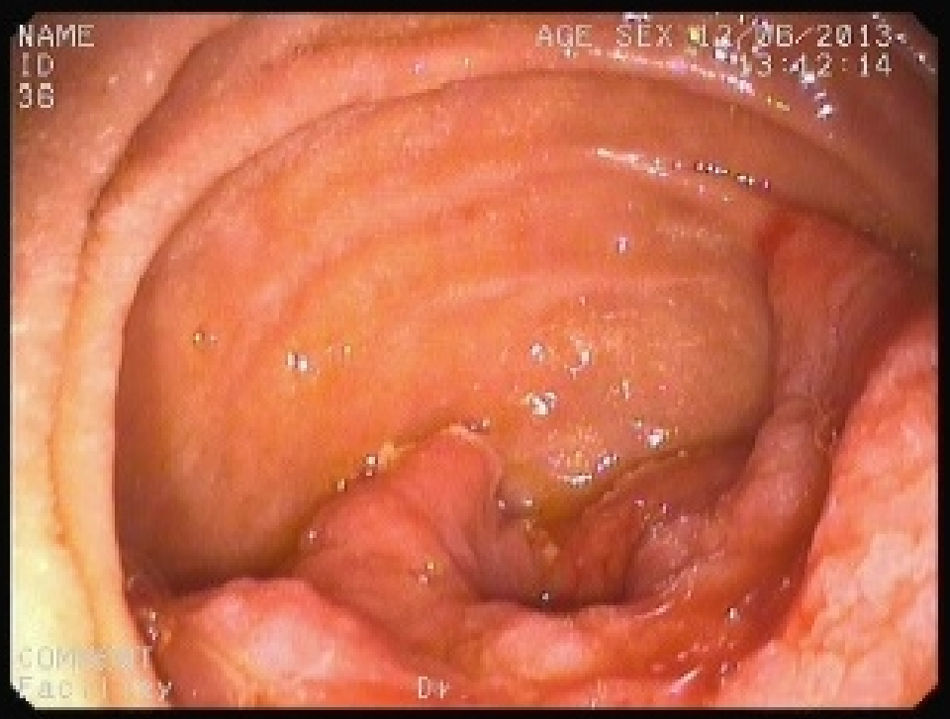
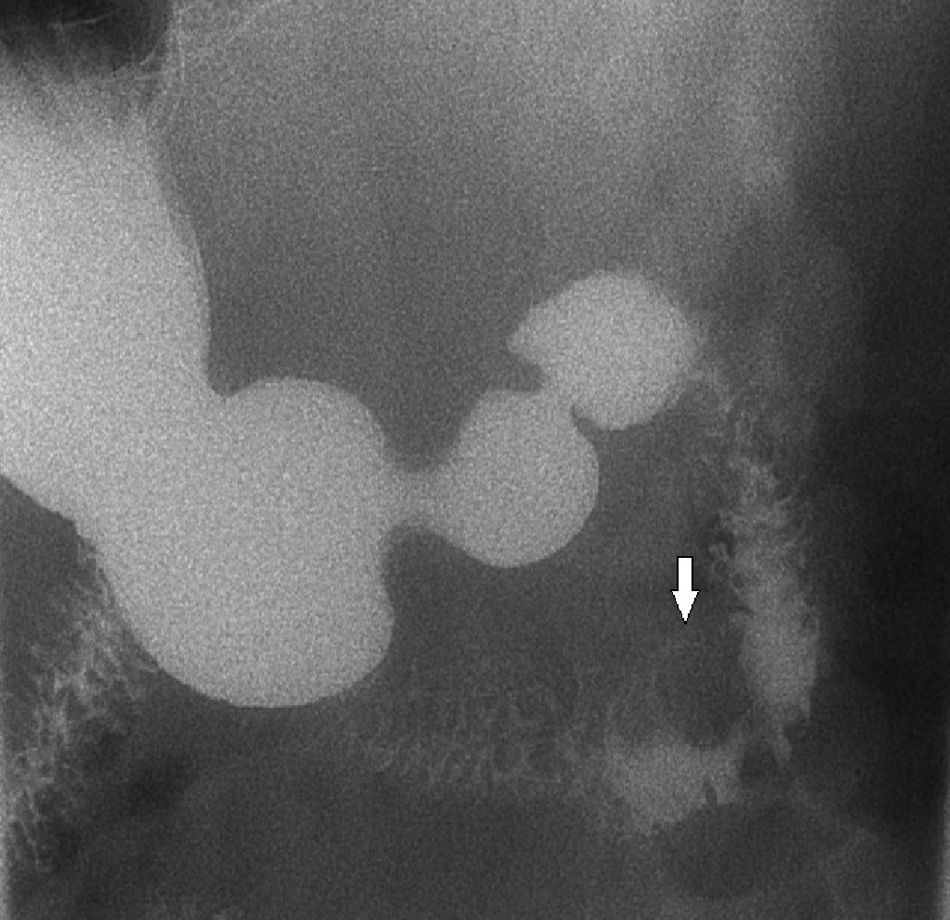
Clinical caseA 35-year-old male who visited due to dyspepsia. Gastroscopy revealed the existence of an exophytic tumour with a friable adenomatose appearance in the second and third duodenal portions (Fig. 1), without involving the duodenal bulb and occupying more than 75% of the duodenal circumference. The results of laboratory tests showed that carbohydrate 19.9 (Ca 19.9) tumour antigen marker and carcinoembryonic antigen (CEA) were within normal limits (5UI/ml and 0.1ng/ml, respectively). Computed tomography (CT), nuclear magnetic resonance imaging (NMR) and endoscopic ultrasound showed that it was a neoplasia of the second and third duodenal portions, without local or remote lymphatic metastasis. Colonoscopy and complete intestinal transit (Fig. 2) ruled out the existence of other polyps in the rest of the intestine. Given these findings, it was decided to operate surgically to achieve exeresis of the lesion.
The above findings were confirmed during surgery, so that broad resection was performed including exeresis of the second, third and fourth portions of the duodenum, with local lymphadenectomy and manual duodenal-jejunal latero-lateral anastomosis. There were no incidents during the postoperative period, and on the third day after surgery the patient commenced an oral diet based on what he could tolerate, and he was discharged from hospital on the seventh day.
The definitive histopathological diagnosis was of primary adenocarcinoma of the second and third portions of the duodenum that infiltrated the muscularis propia (pT2), without lymphovascular invasion, moderately differentiated (G2), with local lymphatic involvement (N0) or remote metastasis (M0), over a tubulovillous adenoma. After oncological evaluation no adjuvant chemotherapy treatment was given. The patient remains free of disease after 25 months of follow-up.
DiscussionDuodenal adenocarcinoma represents only 0.3% of gastrointestinal neoplasias, and 15% of them occur in the first portion, 40% in the second and 45% in the third and fourth portions of the duodenum.3
Non-bulb duodenal adenomas are rare lesions and are classified as precancerous lesions which may be associated with diseases such as familial adenomatous polyposis or Peutz-Jeghers syndrome. They may also appear sporadically, and 2 mechanisms for the development of duodenal carcinoma have been suggested: the adenoma-carcinoma sequence and the development of cancer de novo.
It has been reported that the survival rate is higher for small bowel adenocarcinoma when it is not associated with sporadic adenoma. The majority of cases of adenocarcinoma and sporadic adenoma are located at the level of the duodenum, while sporadic adenoma is located at the level of the duodenum and jejunum.1
The symptoms are not specific, and upper digestive tract endoscopy is the gold standard for diagnosis. Nevertheless, false negatives may exist in the third and fourth portions of the duodenum, as these may be inaccessible for this technique.4 Endoscopic ultrasound and CT are suitable means for staging tumours, although sometimes other techniques are needed such as endoscopy of the duodenal bulb or double-balloon enteroscopy to establish the diagnosis.
The optimum surgical treatment is not clearly defined. Initially duodeno-cephalo-pancreatectomy was recommended,5 although recently this tendency has been questioned in favour of segmentary duodenal resection.4,6
Although the morbidity recorded for both types of surgery is similar, some authors have mentioned a slightly higher rate of morbidity following duodenal resection.7 with 9–25% of peripancreatic fistula, 20% intra-abdominal abscesses, 9% peritonitis, 13% intra-abdominal bleeding and 22% delay in gastric emptying.
No differences were found in the literature between these two techniques in terms of mortality,7 although no study compares both surgical procedures for tumours in the same location.
Neoplasias of the first portion of the duodenum have the worst prognosis, due to its topographical relationship with other adjacent organs, which is not the case for the other portions of the duodenum.8 This is why duodeno-cephalo-pancreatectomy would be more appropriate at proximal locations, and this is also so in patients with locally advanced disease (N1), while segmentary duodenal resection is preferable for distal locations, as it seems to give rise to fewer complications, has an easier postoperative process and the same rate of survival. Good results have been recorded for segmentary resections, independently of the state of the local ganglia.9
Although the role of adjuvant chemotherapy is unclear, some authors found that it leads to an improvement in long-term survival.10
Our patient had a T2 duodenal adenocarcinoma without lymphatic or pancreatic invasion, so that a segmentary resection was performed with a good result, without adjuvant chemotherapy.
To conclude, and taking the rarity of duodenal adenocarcinomas into account, it seems that the most important factor, apart from diagnosis itself, is to determine its location, given that this may affect which surgical strategy is applied.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Jiménez-Fuertes M, Ruíz-Tóvar J, Díaz-García G, Durán-Poveda M. Adenocarcinoma de la tercera porción duodenal moderadamente diferenciado. Cir Cir. 2017;85:76–79.