Mesenteric cysts are very rare abdominal growths, generally asymptomatic, and which are usually detected incidentally while performing a physical examination or an imaging test. Complications such as infections, haemorrhage, torsion, rupture, or bowel obstruction, are seldom found in this pathology, but they can be a cause of acute abdomen. The purpose of this report is to describe the characteristics and the clinical outcome of a male patient with an infected mesenteric pseudocyst of the jejunum.
Clinical caseA 49 year-old male was admitted to the emergency department with 6-day onset of abdominal pain, bowel obstruction signs, palpable tumour located in the upper hemi-abdomen, systemic inflammatory response syndrome, 36,100/mm3 white cells, 4.21ng/ml procalcitonin, abdominal computed tomography scan with evidence of a mesenteric cystic tumour. An exploratory laparotomy was performed, finding the presence of a mesenteric pseudocyst of the jejunum with infection signs, extirpated and sent for histopathological examination. The clinical progress of the patient was satisfactory with the discharge of the patient 7 days after the surgical intervention.
ConclusionThese cysts can debut as an acute abdomen due to haemorrhage, infection, obstruction and/or bowel perforation, complications can be life threatening if not detected and surgically treated at an early stage by performing a resection of the pseudocysts, with or without bowel resection, depending on the location and the size of the cyst.
Los quistes mesentéricos son tumores intra-abdominales raros, generalmente asintomáticos, y se detectan incidentalmente durante el examen físico o radiológico. Las complicaciones como la infección, hemorragia, torsión, ruptura, obstrucción intestinal, son poco frecuentes, pero pueden ser causa de abdomen agudo. El propósito de este reporte es describir las características y evolución clínica, de un paciente masculino con un pseudo-quiste mesentérico infectado de yeyuno.
Caso clínicoMasculino de 49 años que ingresó al servicio de urgencias por dolor abdominal de 6 días de evolución, con datos de obstrucción intestinal, tumor palpable en hemiabdomen superior, síndrome de respuesta inflamatoria sistémica, leucocitosis de 36,100/mm3, procalcitonina de 4.21ng/ml, tomografía computada de abdomen que evidencía una tumoración quística a nivel de mesenterio, por lo que se realizó laparotomía exploradora encontrándose como hallazgo la presencia de un pseudoquiste mesentérico en yeyuno con datos de infección, el cual fue extirpado y enviado para estudio histopatológico. La evolución clínica del paciente fue satisfactoria dándose de alta 7 días después de la intervención quirúrgica.
ConclusiónLos quistes mesentéricos pueden presentarse con abdomen agudo por hemorragia, infección, obstrucción y/o perforación intestinal, las cuales son complicaciones que pueden poner en peligro la vida del paciente si no se detectan y manejan de forma oportuna con resección del pseudoquiste con o sin resección intestinal, dependiendo de la localización, y el tamaño de la afección.
Mesenteric cyst is a term that only refers to cysts originating in the mesentery. It is a very rare intra-abdominal tumour, generally asymptomatic, and is usually detected incidentally while performing a physical examination or an imaging test.1
Lida et al. mention that the first description of a mesenteric cyst was made by Benevieni in 1507, during the autopsy of an 8-year-old boy.2
The cause of a mesenteric cyst is still unclear; however, it has been attributed to the obstruction or injury of the lymph nodes and to the proliferation of ectopic lymphoid tissue. Congenital diseases, diverticula, surgery in the pelvic area, and pelvic inflammatory diseases have been suggested as aetiological agents.3,4
The incidence of mesenteric cysts reported varies from 1 per 27,000 to 250,000 hospital admissions.5 These cysts are asymptomatic in most cases, and are usually detected incidentally while performing imaging tests. Although complications are uncommon, cases of infection, haemorrhage, volvulus, perforation and obstruction have been reported.6,7 The symptoms associated with mesenteric cysts appear mainly in patients presenting cysts with diameters above 5cm.8
The inner wall of the mesenteric cyst is mainly composed of columnar epithelium or cubical endothelial cells, some of which are incomplete.9 The endothelial cells are classified as false cysts, and they may be caused by trauma, infection or degeneration.
Mesenteric cysts can be classified according to cause and clinical presentation (embryologic, traumatic, neoplasic, and infectious) or according to the histopathological result (mesothelial, endothelial, enteric, urogenital, dermoid).10
The mesenteric pseudocysts (false cysts) are a variant of mesenteric cystic tumours, which are even rarer, since only 14 have been reported in the Japanese literature. Aetiologically, they are of infectious or traumatic origin, with lymphatic or purulent fluid accumulates between the mesentery layers, causing ballooning. Histologically, they are characterised by a lack of epithelial lining in their wall, and they may contain necrotic material, fibrin, macropaghes and lymphocytes.11
The treatment of choice for the mesenteric pseudocyst is the complete surgical resection, with or without bowel resection.
The purpose of this report is to describe the experience in the management of a patient with an infected jejunal mesenteric pseudocyst, and to review the existing information about this topic in the medical literature.
Clinical caseA 49-year-old male was admitted to the emergency department with a 6-day history of mild colicky abdominal pain, not related to food. After 72h, the pain intensified and an asymmetric abdominal distension joined, worse in the upper hemi-abdomen, and constipation resistant to treatment, treated with analgesics (paracetamol). He did not respond to non-specific homoeopathic treatment. In addition, he presented nausea and food-content vomiting on several occasions until he completely stopped tolerating any type of food. Unquantified hyperthermia appeared. In a direct interview, the patient referred to weight loss of 10kg in the course of a year, which he attributed to poor dietary habits, and denied having presented similar symptomatology previously. His vital signs at admission were: blood pressure 120/80mm Hg, heart rate 114bpm, respiratory rate 24rpm, temperature was 38.5°C. On physical examination: painful faeces, thin complexion, dry oral mucosa, pulmonary fields with basal bilateral hypoventilation without added noises; he presented tachycardia, without additional events. The abdomen presented irregular distension, more pronounced in the left superior quadrant; at auscultation, decreased peristaltic noises in frequency and intensity, with generalised pain on deep and light palpation, which increased in the left superior quadrant, negative rebounce. On palpation, a mass at the epigastrium and mesogastruim level of approximately 7cm in diameter, with regular edges, and painful at mobilisation was found. The laboratory studies revealed: haemoglobin 13.2g/dl; haematocrit 38.8%; leukocytes 36,100/mm3; segmented 84%; bands 7%; lymphocytes 3%; monocytes 6%; platelets 575,000/mm3; serum procalcitonin 4.21ng/ml. Double-contrast computerised axial tomography of the abdomen showed intestinal obstruction data, scarce free fluid in cavity, and the presence of a cyst-like tumour located at the small bowel mesentery level (Fig. 1).
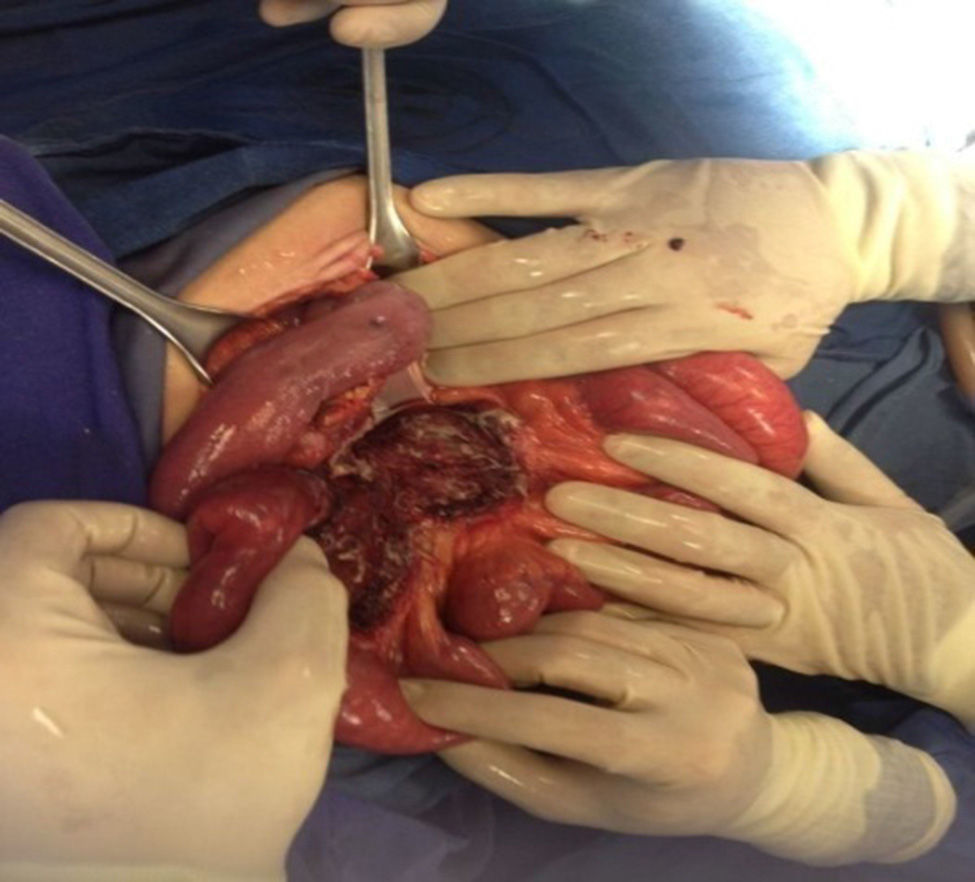
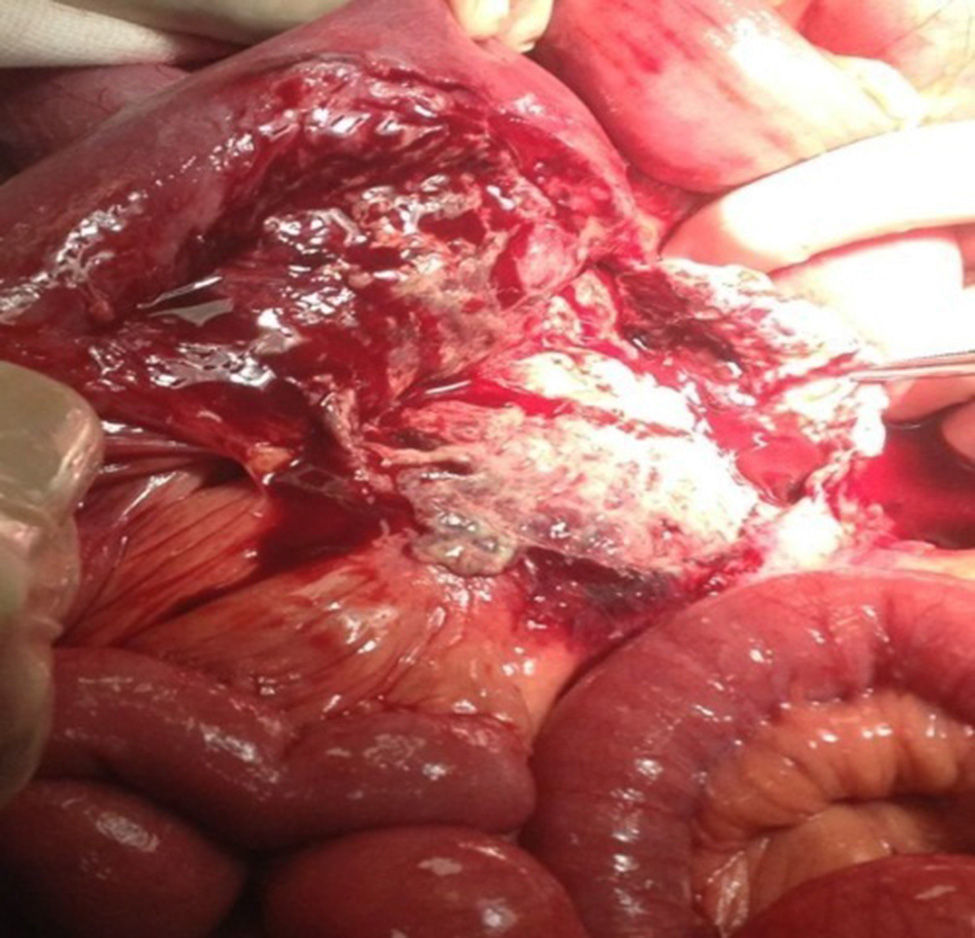
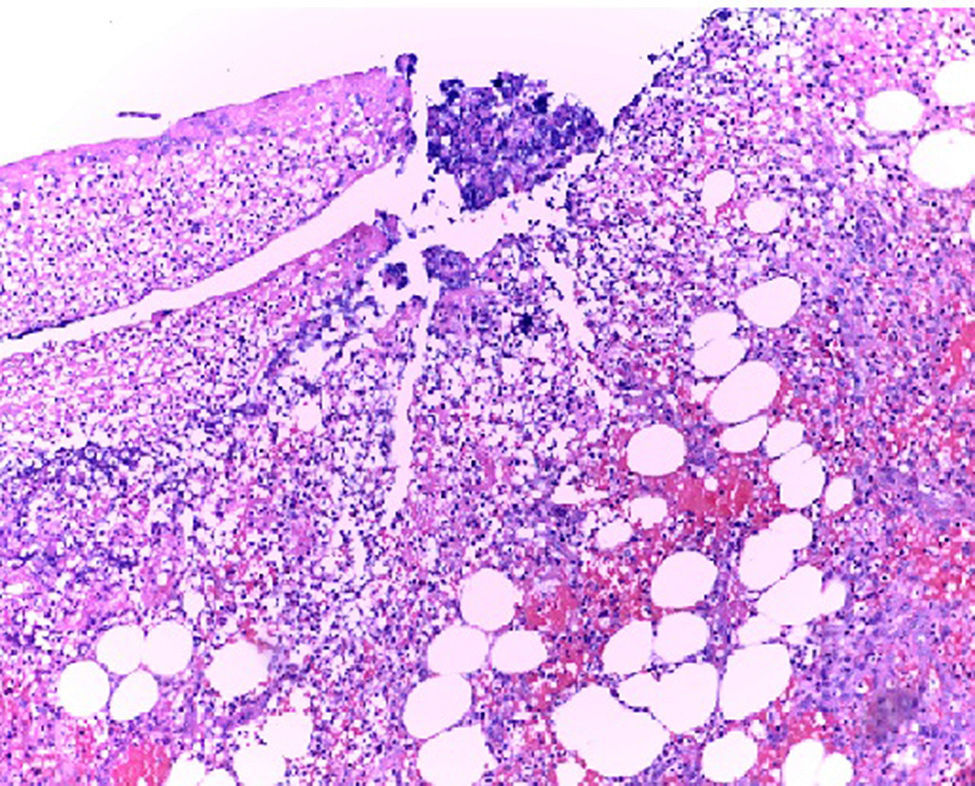
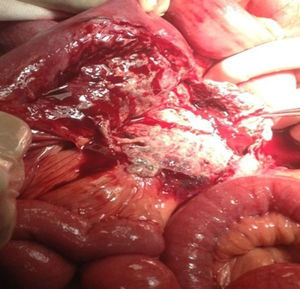
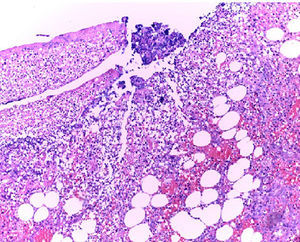
In the presence of abdominal pain, fever, leukocytosis with left deviation, elevated procalcitonin, radiological evidence of cystic tumour and intestinal obstruction, performance of exploratory laparotomy was decided. Preoperative management was started with nasogastric intubation, intravenous hydration, antibiotics such as ertapenem, 1g intravenously. During exploratory laparotomy, a mesenteric cyst measuring approximately 13cm×10cm×7cm was found at jejune level, fixed in the ligament of Treitz and the root of the mesentery, 30cm towards the fixed limb. The cyst, of necrotic aspect and with data of thrombosis, contained purulent, foetid material in a volume of approximately 200ml and was associated with lax inter-limb adhesions. No involvement of the jejuno limbs was observed. 20ml of seropurulent material at the pelvic cavity level was withdrawn and sent for microbiological analysis (Figs. 2 and 3). On exploration of the rest of the abdominal internal organs, multiple diverticula were observed at the cecal appendix, caecum, transverse and sigmoid colon level. During the procedure, the cyst broke in several necrotic areas, so aspiration and resection of the mesenteric cyst inner wall was performed. Viability of the jejunum and its mesentery was then checked. Once the cyst resection was finished, a thorough washing of the abdominal cavity was conducted with 5l of 0.9% saline solution. The closing of the abdominal wall was performed by planes. The microbiological study was negative for the development of micro-organisms after 72h of seeding in culture medium. The histopathological study of the cyst capsule, stained with haematoxylin and eosin, observed with a 100x microscope, reported the presence of connective tissue composed of spindle cells with ample, eosinophilic cytoplasm, with round and oval nuclei without atypia, consistent with the diagnosis of infected jejunal mesenteric pseudocyst (Figure 4).
The clinical progress of the patient was satisfactory, presenting fever spikes of up to 38.5°C during the two days following surgery, and paralytic ileus, which resolved spontaneously leading to oral route start at the fourth day. Blood biometry and control serum procalcitonin performed at third day after surgery were within normal limits. The antibiotic regime lasted for seven days (1g of ertapenem administered intravenously). No postoperative complications presented and the patient was discharged seven days after surgical intervention, to continue ambulatory follow-up as an outpatient.
DiscussionAlthough mesenteric cysts may occur at any age, they are more common at ages 40–70; however, they also affect children younger than 10 years. The age of the patient described here, 49 years of age, coincides with ages reported in previous studies.10 Regarding gender, there are reports showing male predominance; however, in the Western world, the frequency reported has been higher in females, which differs from the male gender of the case described in this report.12
Generally, the size varies from few centimetres up to 10cm, and they can be of greater size, as the one described in the present case: 13cm.13 The most frequent location is the mesentery (60%), followed by mesocolon (24%), and the retroperitoneum (14.5%); while undefined location is 1.5% of the cases.14 In this patient, the pseudocyst was located in the jejunal mesentery at the Treitz ligament level, affecting approximately 30cm of the intestinal limb.
Most of the mesenteric cysts are asymptomatic, and are usually detected incidentally while performing imaging tests such as ultrasound scan, computerised axial tomography or nuclear magnetic resonance, or during surgical procedures for other purposes.15
The sensitivity and specificity of the imaging studies have not been established yet; however, it is indicated that the ultrasound scan is more sensitive at diagnosing the internal nature of the mesenteric cysts, the computed tomography offers more accurate data on the dimensions and content of the cyst, and magnetic resonance is even more sensitive in locating the cyst. Some authors suggest that the high-resolution computed tomography, where feasible, should be the imaging study of choice.7,11 In the presented case, the CT was preferred due to the presence of abdominal pain, tumours, any data of intestinal obstruction, and the complication.
The abdominal symptoms caused by mesenteric cyst are: abdominal pain, 55–82%; palpable abdominal tumour, 44–61%, and abdominal distension secondary to intestinal process of occlusion, 17–61% of the cases.3,7,16,17 The cardinal symptom that prompted the patient described here to seek for emergency attention was abdominal pain, abdominal distension secondary to high intestinal obstruction, weight loss, and data from blood biometry showing infection (leukocytosis and young forms of leukocytes). This corresponds with previous reports, indicating that patients who develop infection, haemorrhage, volvulus, intestinal perforation or obstruction seek emergency consultation with data indicating acute abdomen.3,7,18
The treatment of choice is the surgical resection of the cyst, with or without the resection of the affected intestinal segment.14 The management of the mesenteric pseudocyst of the jejunum in the patient presented here was conducted solely by drainage and surgical resection of the pseudocyst without performing intestinal resection; this was due to the length of the intestinal affection and the risk that a short intestine represents, regardless of the higher risk of recurrence and infection that presents this modality of management.7 The intestinal resection is only recommended when there is evidence that the blood supply of the intestinal segment where the cyst was resected is compromised. The postoperative period passed without complications, as described. It is worth mentioning that, with the exception of malignant cystic mesotheliomas, all mesenteric cysts present a favourable clinical outcome; however, they are associated with a high recurrence rate.16
Injuries, found incidentally, associated with pseudocyst: multiple diverticula in the cecal appendix, caecum, transverse and sigmoid colon. In the search of associations of the mesenteric cyst with diverticular disease, only one report describing one case was found,1 located at the level of the ascending colon mesentery. This is consistent with the aetiological agents that have been attributed to mesenteric cyst development, among them the presence of diverticula.3,4
ConclusionMesenteric cysts are generally detected incidentally while performing imaging test for diagnosis or during a surgical procedure; although they can present with acute abdomen due to haemorrhage, infection, obstruction and/or intestinal perforation, complications that can be life threatening if not detected and treated at an early stage by performing a resection of the pseudocyst, with or without bowel resection, depending on the location and the size of the cyst.
Conflict of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: Bolívar-Rodríguez MA, Cazarez-Aguilar MA, Luna-Madrid EE, Morgan-Ortiz F. Pseudoquiste mesentérico infectado en yeyuno: reporte de un caso. Cir Cir. 2015;83:334–338.