Hemangiolymphangiomas are extremely rare tumours arising from blood and lymphatic vessels. It is a benign disorder, and 95% are of the neck and axilla.
ObjectiveTo present a case of hemangiolymphangioma of the spermatic cord with contralateral recurrence.
Clinical caseA 17-year-old patient with a progressively growing tumour in the right inguinoscrotal region. Examination revealed a painless, movable and soft right inguinoscrotal tumour, mobile and soft. Surgical resection showed a 25cm×25cm tumour from spermatic cord, right testicle, and subcutaneous cellular tissue. Histopathological study reported a hemangiolymphangioma.
ConclusionsThe spermatic cord is an unusual location of hemangiolymphangiomas with contralateral recurrence. Surgical treatment, with histopathological diagnosis, is associated with good prognosis.
Los hemangiolinfangiomas son tumores benignos raros, provenientes tanto de vasos sanguíneos como linfáticos. El 95% se encuentran en cuello y axila.
ObjetivoReportar el caso de un hemangiolinfangioma de cordón espermático con recurrencia contralateral.
Caso clínicoPaciente masculino de 17 años de edad, con tumour en región inguinoescrotal derecha, de crecimiento progresivo. A la exploración física se encontró tumour derecho inguinoescrotal doloroso, de consistencia blanda y móvil. Se resecó un tumour de 25×25cm que tenía involucro de cordón espermático, testículo derecho y tejido celular subcutáneo. El estudio histopatológico confirmó el diagnóstico de hemangiolinfangioma.
ConclusiónEs inusual la localización de hemangiolinfangiomas de cordón espermático, que además tuvo recurrencia contralateral. Debe confirmarse su diagnóstico con estudio histopatológico. El tratamiento es quirúrgico y se obtiene buen pronóstico.
Hemangiolymphangiomas are mixed lesion with a vascular and lymphatic component.1 They are generally benign in nature leading to favourable prognosis. They can be congenital or appear in infancy.2
There is a prevalence in the male of 2.4:1. There is greater risk of the hemangiolymphangiomas presenting in premature babies and in live newborns incidence is 1:12,000. 40–60% of these are discovered at birth (congenital), 80–90% during the first 2 years of life (the age with most frequent presentation) and this frequency decreases with age.3
In 95% of cases, presentation is more frequent in: head, neck and axilla; 5% may be located in: mediastinum, retroperitoneum and mesentery, and is extremely rare in the groin. It may be associated with Klipple–Trenaunay–Weber syndrome, which is a rare congenital disease which was characterised by arteriovenous fistulas and multiple hemangiomas.2–4
They are benign tumours which may infiltrate adjacent organs and cause severe malformations in the cavity and extremities.
The aetiology is unknown. One theory considers that during embryogenesis lymphatic tissue was deposited in the wrong areas with the result that an appropriate connection with central lymphatic pathways was obstructed, and were joined together with blood vessels.4
In general the tumours are asymptomatic, and several reports describe that pain is rare, and that the main concern is over function and aesthetics. Complications will depend on the affected organ, and may include vascular compromise through obstruction, lymphedema, and compartment syndrome (which is extremely rare).
AimOur report is a case of hemangiolymphangioma of the spermatic cord with contralateral recurrence and upon which no known reports exist on this location, according to our review of references.
Clinical caseA 17 year old male patient with a history of left scrotal and testicular hemangiolymphangioma surgical resection at the age of 2, and tonic–clonic seizures treated with valproate and magnesium.
During the treatment and control of a tonic-clonic seizure by the Emergency Service of the Centro Médico Adolfo López Mateos (ISEM), a physical examination revealed the following in the right hypogastrium and inguinal and testicle region: increase in hypogastrium volume and a 25cm×25cm tumour at pubis level spreading to the inguinal channel and right scrotum sac; it was painful to the touch, soft in consistency, moveable, with scrotal skin attached, enlargement of the spermatic cord and the right testicle; the left scrotal sac had no testicle. Adenomegalias were not found (Fig. 1). The patient stated that the increase in volume had been progressive, over 2 years and there was a piercing pain on touch, with discomfort even from contact with underclothes. An assessment was made by the Urology Unit, which requested computed tomography of the abdomen and pelvis. This showed amorphous heterogeneous imaging with densities of 114 to 42 Houndsfield Units in the right scrotal sac. When contrast imaging was used its spread to the inguinal canal and subcutaneous cellular tissues became clear, with an approximate dimension of 26.4cm×25.7cm in antero posterior and transverse edges (Fig. 2). Tumour markers were found to be within normal limits. The laboratory report was as follows: 204UI/l lactate dehygrogenase, 0.77UI/ml alfa-fetoprotein, ≤1.2mIU/ml chorionic gonadotropin fraction β hormone.
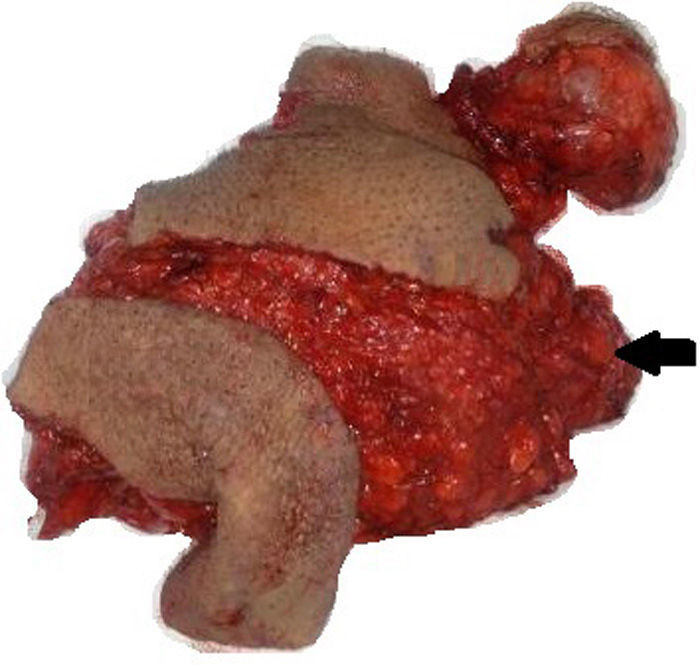
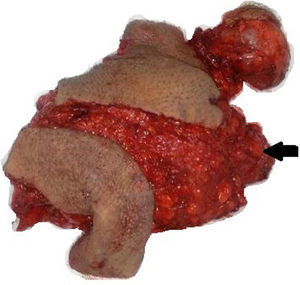
Surgical resection was performed with the following findings: 25cm×25cm soft tumour, with celluloadipose and lymphatic macroscopic characteristics, well defined edges, with subcutaneous cellular tissue, spermatic cord, scrotum and the right testicle; with celluloadipose and lymphatic macroscopic characteristics. After orchiectomy, the surgical specimen was sent for testing to the pathology department (Fig. 3).
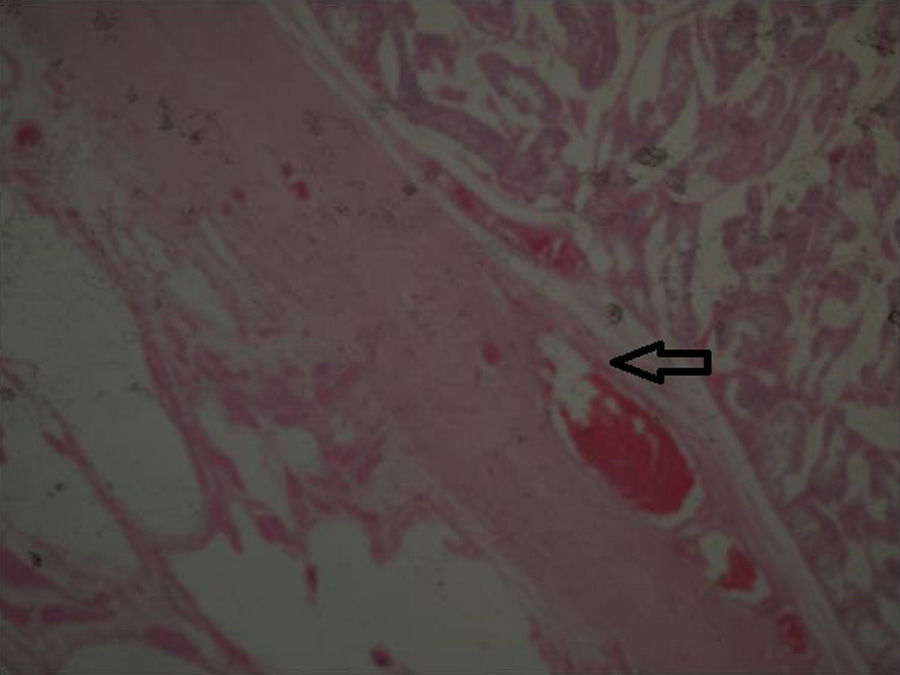
Two testicle specimens were received. The first measured 5cm×4cm, with a scrotal region measuring 4cm×2cm, a dark brown, rugged epidermis, with characteristic congestive hairs; the tunica albuginea was smooth and shiny, as was the paratesticular cystic lesion of 2cm×1cm. The second specimen measured 28cm×10cm×7cm, with 2 flaps of skin, the largest measuring 15cm×10cm and the smallest 11cm×10cm; the epidermal surface was rugged and a brownish greyish colour. The spermatic cord of 6cm×1cm was identified, with an external reddish brownish colour and when dissected, contained dilated vascular structures in its 3 sections. Cavernous hemangiolymphangioma of 15cm of spermatic cord and paratesticular soft tissues (Fig. 4).
A second operation was performed by the Plastic Surgery Service, where an abdominoplasty type abdominal advancement flap was performed (Fig. 5).
DiscussionVascular malformations are localised or diffuse errors of angiogenesis or vasculogenesie (embiogenesis period) and are classified as low-flow which are capillary, venous, or lymphatic malformations, or high-flow which are ateriovenous or ateriovenous fisula malformations.5,6
The classification of lesions from lymphatic vessels are: benign: (a) lymphagiomas with their 3 variants: capillary, cystic and cavernous; (b) linfagioqueratoma; (c) mixed lymphagioma (hemangiolymphangioma) which is our case. Malignant: lymphangiosarcomas.5,6
The diagnosis of this type of lesion occurs through histopathological examination. Their differential diagnoses are hermangiopericytoma, angiosarcoma, pure hemangiomas, pure lymphatic malformations. The lymphatic malformations may mainly be classified in accordance with histopathological characteristics into cavernous, cystic or capillary.7,8
They are clinically characterised by being grouped into blisters, forming raised plaques, being verrucous and pink or reddish blue in colour, with a content based on lymph or erythrocyte cells due to prominent and dilated lymphatic and vascular channels.9
Medical check-ups are recommended for patients with spontaneous regression. If tumours are superficial they may be treated with corticosteroids may be administered or photocoagulation with laser and good aesthetic and functional outcomes are obtained. For deep tumours, as in the case mentioned, the treatment of choice is block surgical resection.10,11
Recurrence is variable and may occur in 10–100% of cases. It depends on the extension of the excision. Locations with main recurrence are mouth, larynx, hypopharynx and tongue. Mortality is reported to occur in 6–10% of cases.11,12
ConclusionsHemangiolymphangiomas are rare lesions with a favourable prognosis. This was the case of our patient who despite this aesthetic deformity was treated satisfactorily. The patient is currently at the 6 month stage of check-ups and no recurrence has occurred. However, medical surveillance will be continued in order to identify new cases of recurrence at an early stage, identify early stage lesions and offer the right treatment with limited damage.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Rogel-Rodríguez JF, Gil-García JF, Velasco-García P, Romero-Espinoza F, Zaragoza-Salas T, Muñoz-Lumbreras G. Hemangiolinfangioma de cordón espermático en adolescente de 17 años, reporte de caso. Cirugía y Cirujanos. 2016;84:162–166.