Acute pseudo-obstruction of the colon is a disorder characterised by an increase in intra-luminal pressure that leads to ischaemia and necrosis of the intestinal wall. The mechanism that produces the lesion is unknown, although it has been associated with: trauma, anaesthesia, or drugs that alter the autonomic nervous system. The pathophysiology of medication induced colon toxicity can progress to a perforated colon and potentially death.
ObjetivePresent a case of a colonic pseudo-obstruction in a patient with polyfarmacy as the only risk factor and to review the medical literature related to the treatment of this pathology.
Clinical caseThe case is presented of a 67 year old woman with colonic pseudo-obstruction who presented with diffuse abdominal pain and distension. The pain progressed and reached an intensity of 8/10, and was accompanied by fever and tachycardia. There was evidence of free intraperitoneal air in the radiological studies. The only risk factor was the use of multiple drugs. The colonic pseudo-obstruction progressed to intestinal perforation, requiring surgical treatment, which resolved the problem successfully.
ConclusionIt is important to consider drug interaction in patients with multiple diseases, as it may develop complications that can be avoided if detected on time.
La pseudo-obstrucción colónica aguda se caracteriza por la dilatación masiva del colon, con aumento de la presión intraluminal que condiciona isquemia y necrosis de la pared intestinal. No se conoce el mecanismo que produce la lesión, aunque se ha asociado con: traumatismo, anestesia o agentes farmacológicos que alteran el sistema nervioso autónomo. La patofisiología de la toxicidad colónica por fármacos puede progresar hasta la perforación colónica y potencialmente a la muerte.
ObjetivoComunicar el caso de una paciente con polifarmacia como único factor de riesgo para la pseudo-obstrucción colónica, y presentar la revisión de la bibliografía médica relacionada con el tratamiento.
Caso clínicoPresentamos el caso de una mujer de 67 años con distensión y dolor abdominal difuso, progresivo de intensidad 8/10 por pseudo-obstrucción colónica, acompañado de febrícula y, taquicardia. En los estudios de gabinete se observó aire libre en cavidad. El único factor de riesgo que tenía la paciente fue el uso de múltiples fármacos. El cuadro de pseudo-obstrucción evolucionó hasta la perforación intestinal, que requirió tratamiento quirúrgico, con resultado exitoso.
ConclusiónEs importante tener en cuenta las interacciones farmacológicas en los pacientes con múltiples enfermedades, ya que pueden condicionar complicaciones como la perforación colónica, que de ser detectadas a tiempo se podrían evitar.
Acute pseudo-obstruction of the colon is a disorder characterised by massive dilatation of the colon, where there is no evidence of mechanical obstruction, and by definition is associated with a secondary or base disease. Pseudo-obstruction, also known as Ogilvie syndrome, often occurs in elderly, patients who are being treated with a great many drugs, and although rare, drug-induced colonic toxicity is a disorder which should be recognised in time.1,2
Colonic pseudo-obstruction is always secondary to underlying disease such as: infectious, cardiac, neurological or drug-induced processes. Spontaneous perforation presents in 3–15% of cases with 40% mortality.3
The pathophysiology of drug-related colon toxicity starts as a pseudo-obstruction of the colon where the ileus or colonic paresis which results in massive dilatation, is secondary to the use of drugs which act on colonic innervation or motility. The drugs which are most usually associated with this disease include: narcotics, phenothiazines, antidepressants, and calcium channel-blockers. Despite the fact that the association of drugs with this disease is based on case reports, an obvious causal relationship has been established with some drugs such as loperamide, narcotics, phenothiazines and vincristine. Probable association with: atropine, nifedipine, procainamide, tricyclic antidepressants, amphetamines, barbiturates, chlonidine, dicumarol and verapamil.1
The clinical spectrum of drug-related colonic toxicity varies between: constipation, pseudo-obstruction, ischaemia and necrosis. Clinical suspicion of this disorder is important, as timely discontinuation of the drugs can prevent complications which result in a high morbimortality rate.1,2 Initially the treatment guideline is conservative, colonic decompression can be effective although it carries with it a risk of perforation. Surgical treatment is reserved to cases presenting possible complications such as necrosis or perforation.
ObjectiveTo present a review of the subject and the case of a female patient with polypharmacy, who presented with colonic pseudo-obstruction and evolved torpidly, until she presented perforation with peritonitis. She was managed surgically, and after medical management due to sepsis the patient responded favourably with no complications.
Clinical caseA 67-year old female patient who was admitted with distension and progressive diffuse abdominal pain of 8/10 intensity, with no signs of peritoneal irritation, accompanied by a difficulty in passing wind, and her last bowel movement was 2 days prior to admission. It was decided to hospitalise the patient with a diagnosis of colonic pseudo-obstruction. The patient's medical history included, arterial hypertension treated with nifedipine 20mg/tid, dyslipidaemia treated with atorvastatin 10mg/daily. In addition, the patient was taking quetiapine 300mg/daily, levetiracetam 500mg/bid, desvenlafaxine 50mg/day, piracetam and raloxifene 60mg/day for depression. She had no history of abdominal surgery; she only reported resection of a melanoma on her buttock, reduction mammoplasty, rhytidectomy and resection of an unspecified retro-orbital tumour.
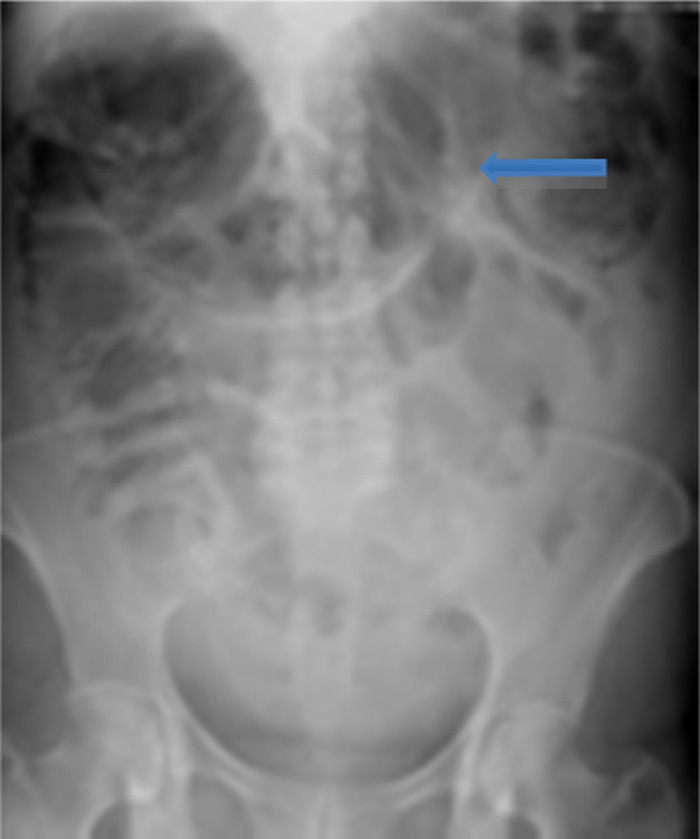
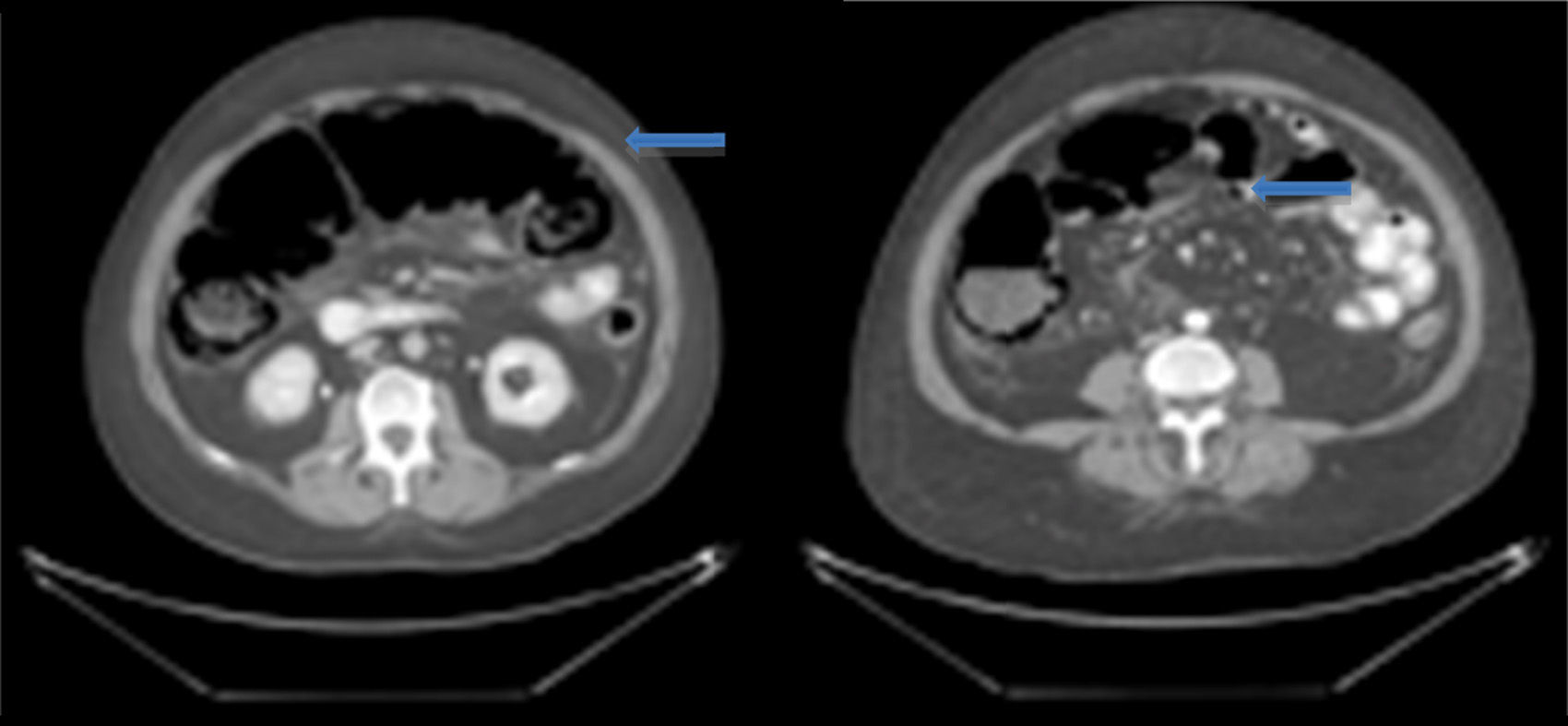
On admission the patient was, dehydrated, tachycardic with a heart rate of 100bpm, low-grade fever, distended, tympanic abdomen, tender on palpation, no peristalsis, no rebound or muscle stiffness. The laboratory tests on admission showed: leucopoenia 4000, creatinine 1.5mg/dl, procalcitonin 60.25ng/ml and C-reactive protein 41mg/l. Abdominal X-rays were requested which showed an increase in the calibre of the ascending and transverse colon, and areas of pneumatosis were observed in the ascending colon, and free intraabdominal fluid (Fig. 1), and therefore tomography of the abdomen and pelvis were requested, which corroborated distension of the ascending and transverse colon with images compatible with pneumatosis, associated with free air bubbles in close proximity to the colon (Figs. 2 and 3). Due to these findings it was decided to undertake an exploratory laparotomy, where purulent free fluid was found, dilated colon loops and necrosis of the caecum, ascending and transverse colon with micro perforation of the transverse colon (Figs. 4 and 5). A resection was performed of the terminal ileum, ascending, transverse and descending colon with mechanical ileo-sigmoid anastomosis, with thorough lavage of the cavity. There were no surgical complications in the transoperative period, and the patient went to intensive care due to haemodynamic instability. In the postoperative period the patient had signs of systemic inflammatory response, and was prescribed meropenem and ketoconazol, as well as mechanical ventilation and hydric resuscitation. Mechanical ventilation was withdrawn on the fifth post-operative day, and the patient's haemodynamic status remained stable without the need for vasopressors. The patient remained in intermediate therapy and evolved well. On the eighth post-operative day she had a bowel movement, and started an oral diet, which she tolerated well. The patient was discharged without complications 11 days after surgery, tolerating an oral diet, and presenting adequate gastro-intestinal function.
Acute colonic pseudo-obstruction is a clinical syndrome which, by definition, implies massive dilatation of the large intestine, with no mechanical obstruction; the disorder is also known as Ogilvie syndrome.1 It is always secondary to underlying diseases such as infectious, cardiac, neurological or drug-related processes,3 as in the case we present in this article, in whom the only identified factor was the use of drugs which reduced colonic motility such as nifedipine, which relaxes smooth muscle by blocking the calcium channels, antidepressants with anticolinergic effect which also inhibit intestinal motility, and which resulted in pseudo-obstruction with massive dilatation of the transverse colon with increased intraluminal pressure, ischaemia and necrosis of the wall and subsequent perforation.1
In cases of colonic pseudo-obstruction with no perforation or haemodynamic instability, treatment is conservative, effective in 53–96% of cases, with a risk of perforation of the colon of less than 2.5%, and mortality from 0% to 14%.4 Conservative treatment includes treating underlying disease, discontinuing the drugs causing colonic hypomotility, and correcting hydro-electrolyte abnormalities.2 Neostigmine is used for decompression of the colon; this is an acetylcholinesterase inhibitor5 with efficacy of 64–91% on the first dose, and in cases of recurrence (30% of cases) a second dose is recommended to increase its effectiveness from 40% to 100%.4 If decompression of the colon is achieved, a transrectal tube or decompressive colonoscopy is used to decrease parietal tension, and thus increase blood flow in the wall and promote peristalsis, which is effective in 61–100% of cases. However, this is not a harmless procedure, as it carries a risk of perforation in 5% and increased mortality.4 Percutaneous or endoscopic caecostomy is used for cases where decompression has not been effective, providing the patient has no signs of perforation or necrosis; this procedure increases the morbidity carried by caecostomy, such as fistula and intestinal leakage.6,7
Surgery is reserved for cases with clinical signs suggestive of peritonitis or perforation and laparotomy is recommended, as in the case of our patient who had signs of free air in the cavity without diagnostic confirmation. The procedure to be carried out will depend on intraoperative findings, as well as the haemodynamic status of the patient, and can go from resection with primary anastomosis to defunctionalisation and bypass of the ileum or colon. Laparoscopy is not recommended, as dilatation of the colon reduces the potential space to create a pneumoperitoneum and manoeuvre inside the abdominal cavity.
Surgery, although it is the definitive treatment in many cases, carries with it a 6% morbidity and mortality of up to 30%; these figures depend on the disease causing the colonic ischaemia.7,8
ConclusionIt is important to take drug interactions into account in patients with multiple diseases, especially in the geriatric population, as they can result in complications with high morbimortality, which can cause intestinal pseudo-obstruction and require surgical treatment which, if detected in time, can be avoided.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Núñez-García E, Valencia-García LC, Sordo-Mejía R, Kajomovitz-Bialostozky D, Chousleb-Kalach A. Perforación colónica secundaria a polifarmacia: reporte de caso. Cirugía y Cirujanos. 2016;84:65–68.