The most severe complication following an intestinal anastomosis is the dehiscence with the consequent development of sepsis, fistulas, stenosis, and death. For this reason the compression anastomosis (NiTi) system was developed, with the aim of reducing these complications.
Material and methodsA retrospective study was conducted, from 1 June 2012 to 30 August 2014, on total of 14 patients operated on the Humanitas Hospital Medical Group Coyoacán, the ASMED, and Clínica Médica Sur. The subjects were predominantly male 65%, a mean age of 58 years, with range 30–79 years.
ResultsA total of 14 patients were included. The indication for surgery was complicated diverticular disease Hinchey II–III (36%), and the procedures performed were: 6 (43%) left hemicolectomy with primary end to end compression anastomosis, 2 (14%) major complications (dehiscence wall and anastomosis), 1 (7%) minor complication (infection of the soft tissues). There was a mean 98ml (range 20–300ml) of intraoperative bleeding, with start of oral feeding on the second day, a mean hospital stay of 4 days (range 2–10), one patient with ileo-rectal anastomosis dehiscence presented on the 4th post-operative day, and performing anastomosis with stapling device and loop ileostomy. Stenosis developed in 7% during follow-up and was resolved with a new anastomosis stapler.
ConclusionsThe NiTi device is an additional alternative for colorectal anastomosis, mainly in low anastomosis, obtaining good results in this study without major complications.
La complicación más grave posterior a anastomosis colorrectal es la dehiscencia, debido al desarrollo de sepsis, fístulas, estenosis y, en casos severos, la muerte; para reducir dichas complicaciones, se creó el sistema de anastomosis por compresión NiTi.
Material y métodosSe realizó un estudio retrospectivo del 1 de junio de 2012 al 30 de agosto de 2014. Un total de 14 pacientes fueron intervenidos en el Hospital Humanitas Medical Group Coyoacán, así como en la Clínica Asmed y en Médica Sur. Predominó en la muestra estudiada el sexo masculino (65%), con una edad media de 58 años (rango, 30-79 años).
ResultadosSe incluyeron un total de 14 pacientes. La indicación de cirugía fue enfermedad diverticular complicada Hinchey II-III (36%), los procedimientos realizados fueron: hemicolectomía izquierda con anastomosis primaria por compresión termino-terminal (43%), con 2 complicaciones mayores (14%) (dehiscencia de pared y de anastomosis) y una complicación menor (7%) (infección de tejidos blandos). El sangrado transoperatorio promedio fue de 98ml (rango 20-300ml); inicio de vía oral al segundo día; la estancia hospitalaria promedio fue de 4 días (rango, 2-10). Un paciente con anastomosis del íleo-recto presentó dehiscencia al 4.° día del postoperatorio, realizando anastomosis con dispositivo de grapeo e ileostomía en asa. Durante el seguimiento se desarrolló una estenosis del 7%, resolviéndose con una nueva anastomosis con engrapadora.
ConclusionesEl dispositivo NiTi es una alternativa adicional para la realización de anastomosis colorrectales, principalmente en anastomosis bajas. En este estudio se muestran buenos resultados, sin incremento de complicaciones.
At present, the need for sphincter saving procedures for diseases of both inflammatory and malignant aetiology requires ultra-low anastomoses with greater risk of leakage. With a view to improving the success rate of these anastomoses, we analysed the factors which might influence and increase the inflammatory process and with it, the rates of bleeding, leakage, dehiscence and stenosis. It is essential to maintain the universal principals for the creation of an anastomosis: avoid tension, preserve good irrigation, appropriate intestinal calibre, absence of septic processes and presence of foreign bodies, as is the case with mechanical anastomoses.
According to Hardy et al.,1 in 1980 Knight and Griffen created the first rectal anastomosis by double stapling, which had significant impact especially on colorectal surgery. In recent years, there have been many changes in mechanical suturing apparatus; in 1985 Hardy et al.1 developed a biofragmentable anastomosis ring (Valtrac BAR, Covidien, Mansfield, MA, USA), reporting it as a safe and reproducible procedure for both elective and emergency surgery.2–6 More recently, a compression anastomosis ring has been developed, ColonRing (NiTi Surgical Solutions Ltd.), comprising a nickel-titanium alloy (Nitinol). Because this device works through compression and not staples, trauma to the bowel wall is reduced and thus it the risk of bleeding and stenosis is also reduced. Furthermore, the ring is eliminated between the seventh and tenth day postoperatively through defecation.
The aim of this article is to analyse the efficacy and safety of colorectal compression anastomoses using the NiTi device.
Material and methodsA retrospective study was undertaken during the period between 1 June 2012 and 30 August 2014, on a total of 15 patients operated in the Humanitas Medical Group (HMG) of Coyoacán, Clínica asMED and Hospital Médica Sur, all of which are in Mexico City. One patient was excluded from the final data analysis due to a technical fault in firing the device, a total of 14 patients were studied and signed informed consent forms. Authorisation was requested and granted by the management of HMG Coyoacán since they had the greatest number of patients included in this study. Preoperative evaluation comprised a complete clinical history to rule out other diseases, we found patients with histories of diabetes mellitus, systemic arterial hypertension and heart disease, and we assessed the anaesthetic and surgical risk.
The demographic data such as, age, gender, and surgical variables such as surgery time, transoperative bleeding, days of hospital stay, start date and tolerance of oral diet, and complications.
The inclusion criteria were all patients operated within the study period that had undergone resection of the colon and anastomosis using the NiTi device. Patients with anastomoses made by stapler or failure of the NiTi device were excluded.
Statistical analysis was undertaken by determining means, averages, deviations and percentages.
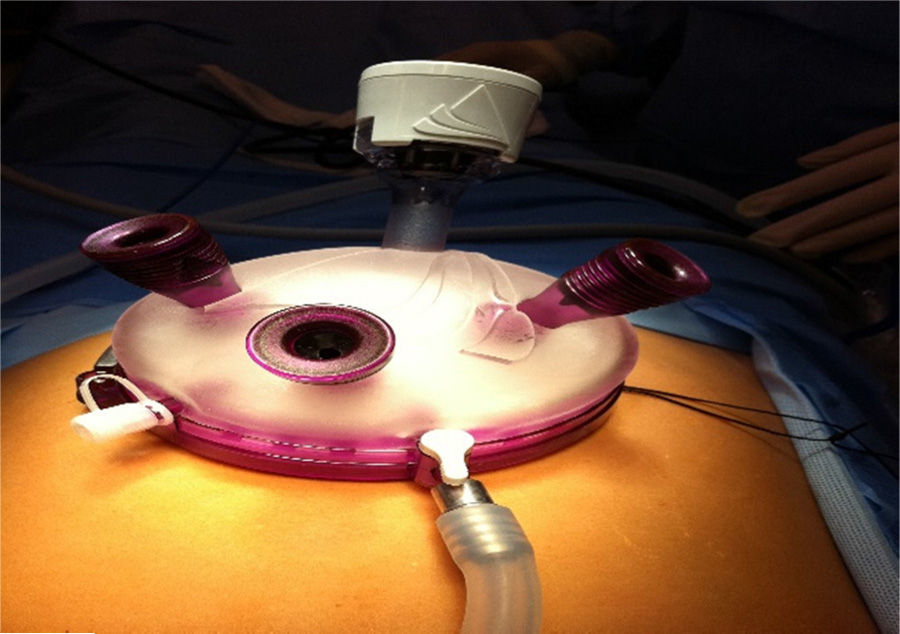
Surgical techniqueSingle-incision laparoscopic surgery (SILS)With the patient in a modified dorsal lithotomy position, under anaesthesia and using asepsis and antisepsis technique, a mid infraumbilical incision of 5cm is made in layers until reaching the cavity and the GelPoint® (Advanced Access Platforms of Applied Medical) is placed (Fig. 1); 3 10mm trocars and a 12mm trocar are placed in the cavity beforehand in rhombus fashion. The left colon is then dissected laparoscopically, starting at the medial portion at the level of the promontory and at the intersection of the superior haemorrhoidal vessels and the promontory; care is taken to identify the left ureter in order to avoid injury to it.
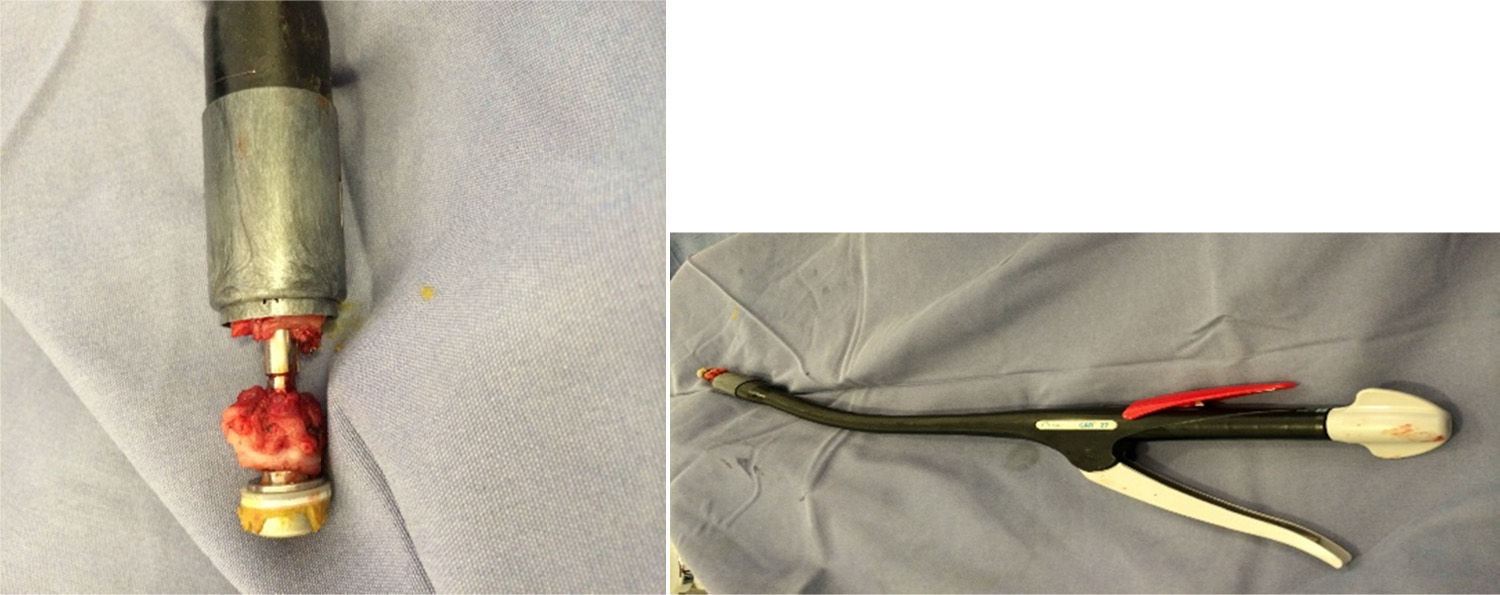
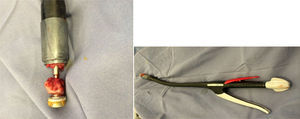
The descending colon is then mobilised to the level of Toldt's line, until reaching the splenic angle. Once the left colon has been mobilised, the posterior fascia are dissected until reaching the union of the upper third with the middle third and the rectum is cut with an Echelon Flex 60mm stapler with gold cartridge; the surgical piece is brought outside once the GelPoint® platform has been removed and the descending colon cut externally, in order to then use the ColonRing (Niti Surgical Solutions Ltd.) in group A. Before loading the CARTM 27 device, the compression anastomosis ring is cooled by submerging it assembled on its loader in a container with a solution of iced saline solution for 5min. Then the CAR™ 27 is loaded and coupled to the distal edge of same. While a purse string suture with Prolene 00 is placed in the proximal end of the colon along with the anvil of the device, the device is introduced transrectally and coupled with the anvil. After checking the segments to be anastomosed, the device is fired. The device is removed and the integrity of the anastomotic doughnut checked (Fig. 2). A hydropneumatic leak test is then performed, haemostasis checked and a drain placed in the gutter and pelvic cavity. The incision is closed by planes and the surgical procedure considered complete.
Traditional laparoscopic surgeryThe same steps as in the single port approach are followed, but the trocars are placed 12mm infraumbilically, 2 right lateral at 2 fingers above the iliac crest and at the height of the umbilical scar on the clavicular midline, and another of 5mm at the height of the umbilical scar on the left side. The infraumbilical incision is widened 4–5cm for the anastomosis and a surgical wound protector placed.
Open or traditional approachWith a midline incision between 15 and 20cm, a lateral to medial approach is taken, with ligation of the vessels with 2-0 suture; the rest of the anastomosis technique is the same as that for laparoscopic surgery. The main difference is that the rectal stump is cut with a contour rather than Echelon stapler.
ResultsThe demographic data show a predominance of the male gender (65%), with a mean age of 58 years (range, 30–79 years). There was 28% comorbidity, with predominance of diabetes mellitus, arterial hypertension and ischaemic heart disease. The preoperative tests showed means of albumin 3.6g/dl and haemoglobin 14.5g.
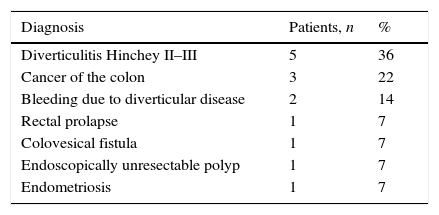
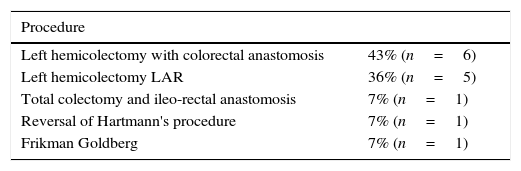
The main indications for surgery are complicated diverticular disease Hinchey II or III (36%; n=5), colon cancer (22%, n=3), bleeding from diverticular disease (14%, n=2), rectal prolapse (7%, n=1), endometriosis (7%, n=1), colovesical fistula (7%, n=1) and endoscopically unresectable polyp (7%, n=1) (Table 1). The surgical procedures were: left hemicolectomy with primary end to end compression anastomosis (43%, n=6), left hemicolectomy with LAR (36%, n=5), total colectomy with ileo-rectal anastomosis (7%, n=1), Frikman Goldberg procedure (7%, n=1), and reversal of Hartmann's procedure (7%, n=1) (Table 2), which were performed by open surgery (43%, n=6), single portal approach (36%, n=5), traditional laparoscopic approach (14%, n=2) and hand assisted surgery (7%, n=1), with no conversions in the laparoscopic approaches. The average surgery time was 100min (90–180). Two major complications presented (14%), consisting of a dehiscence of the wall and a dehiscence of the anastomosis, and one minor complication (7%), a soft tissue infection. Transoperative bleeding was 98ml (20–300); oral diet was commenced on the second postoperative day on average, and the average hospital stay was 4 days (2–10). One patient with ileo-rectal anastomosis presented dehiscence on the fourth post-operative day and required reoperation, a new anastomosis was created with a stapling device protected with loop ileostomy. None of the patients noticed expulsion of the device, and during follow-up there was one stenosis of the anastomosis, which was resolved by reoperation, and a new anastomosis created with a stapling device.
One of the basic principles for a successful colorectal anastomosis is that it should be well-vascularised, and tension free. However, another extremely important aspect is when foreign bodies are left in tissue, which promotes a greater inflammatory response, increasing possible associated adverse effects, such as a reduction in the size of the anastomosis lumen, which might cause postoperative stenosis.7 Anastomotic leaks should not be forgotten either; they increase morbidity and mortality substantially in these types of procedures, and are even more frequent during low anterior resection of the rectum, with a rate described at between 2.9% and 15.3%.8
In order to reduce the complication rate of these anastomoses and therefore reduce morbidity and mortality, new alternatives have been sought for creating anastomoses, including compression anastomosis using a nickel-titanium alloy (Nitinol) device. Nitinol has 2 physical properties: it is temperature dependent, with shape memory and superelasticity. When cool, it has inferior mechanical properties in which it acquires stability, and can become flexible and return to its pre-deformed shape at ambient temperature.9 Superelastic springs of nickel-titanium alloy sheet are used in the CAR NiTi™ 27 in order to maintain continuous pressure in the anastomosis, irrespective of the thickness of the tissue inside the anastomosis.10 And given that the healing process takes place outside the ring (serosa-serosa), an intact anastomosis is formed before the ring becomes detached and is expelled, leaving no foreign material in the body, thus reducing the incidence of anastomosis stenosis.
It is important to stress that although follow-up of this procedure is still short, its safety has been demonstrated in several studies, initially in animals and later in humans,11,12 observing safety results very similar to those obtained with mechanical stapling devices, and some even have lower anastomosis leak rates, as published by D’hoore et al.13 There is already evidence of their use in gastrointestinal oncology patients, as reported by Kim et al.,14 who after assessing 50 patients observed no differences in operation time, transoperative blood loss, time to first flatus, first defecation or complications. Therefore, the CAR™ 27 was approved by the Food and Drug Administration (FDA) for use in intestinal anastomosis in August 2006. In 2013, Masoomi et al.15 performed a study in the United States, In Germany and other countries including a total of 1180 patients, in whom a colorectal anastomosis was created, with a leak rate of 3.22%.
Another factor to be taken into consideration is the cost, which is even lower than that of circular stapling devices (324 vs 360 dollars),16 with no requirements other than the device itself.
ConclusionsThis series is one of the first to be undertaken in our country. Of course, clinical trials with significant samples and medium and long-term follow-up are required in order to be able to establish a true role for the NiTi in colorectal surgery.
The NiTi device is an additional alternative for the creation of colorectal anastomosis, principally in low colorectal anastomosis. Good results were obtained in this study, with complications similar to those described in the literature. Although in the literature the NiTi device is used in ileo-rectal anastomosis, we had to exclude one patient, who presented dehiscence with this device in an ileo-rectal anastomosis. We consider that the thickness of the small bowel increases the possibility of leak or dehiscence, and therefore we do not recommend the device for small bowel anastomosis.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: González-Contreras QH, de Jesús-Mosso M, Bahena-Aponte JA, Aldana-Martínez O, Pineda-Solís K, Mejia-Arcadia SN. Anastomosis colorrectales por compresión utilizando el dispositivo NiTi. Cir Cir. 2016;84:482–486.