Schwannoma is a rare benign tumour derived from nerve sheaths. When derived from the cervical sympathetic chain, it usually presents itself as an asymptomatic mass located in the posterior cervical region, at paravertebral level. Its diagnosis is not easy, usually requiring multiple imaging tests. Its differential diagnosis includes parathyroid adenoma.
Clinical caseA new case of schwannoma of the cervical sympathetic chain in a patient with a synchronous overactive parathyroid adenoma is reported. This case adds to the 60 described in the literature, although to our knowledge no association between schwannoma and parathyroid adenoma has been reported to date.
ConclusionsDespite being a benign tumour, its treatment is a complete surgical resection. The most common complication after the surgery needed for these tumours is ipsilateral Horner syndrome.
El schwannoma es un tumour benigno raro derivado de las vainas nerviosas. Cuando deriva de la cadena simpática cervical se suele presentar como una masa asintomática que se localiza en la región cervical posterior, a nivel paravertebral. Su diagnóstico no es sencillo, por lo que suele precisar de varias pruebas de imagen. Entre sus diagnósticos diferenciales se encuentra el adenoma paratiroideo.
Caso clínicoSe presenta un nuevo caso de schwannoma de la cadena simpática cervical, que se añade a los 60 descritos en la literatura, en una paciente con un adenoma paratiroideo hiperfuncionante sincrónico, asociación que no ha sido descrita en la actualidad.
ConclusionesA pesar de ser un tumour benigno, su tratamiento es la resección quirúrgica completa. La complicación más frecuente tras la cirugía de estos tumores es el síndrome de Horner ipsilateral al tumour.
Schwannoma or neurilemmoma is a rare tumour deriving from peripheral nerve sheaths. They are generally benign, well-delimited, single tumours which rarely become malignant. Cervical sympathetic chain schwannomas are rare.1 They usually present as a slow-growing, cervical mass, and produce no other symptoms. They are diagnosed by means of radiological tests, such as ultrasound of the neck, computed tomography or magnetic resonance. Surgical excision is the treatment of choice for these tumours, in order to be sure of the tumour type. Post-excision Horner's syndrome on the side where the tumour was removed is an expected complication as the sympathetic chain is divided when the tumour is resected.2–4 It is not usually associated with other lesions, and its presentation along with a hyperfunctioning parathyroid adenoma has not been described. We present the case of a cervical chain schwannoma in a woman with an adjacent parathyroid adenoma.
Clinical caseA 58 year old woman under study for primary hyperparathyroidism, with hypercalcaemia and mild hypercalciuria, diagnosed by endocrinology on monitoring hereditary dyslipidaemia, with no clinical manifestations, no osteoporosis or altered renal function. A full hormonal study was performed, no alterations were found in the hormone levels analysed (prolactin, somatostatin, gastrin and thyroid hormones, amongst others, were normal).
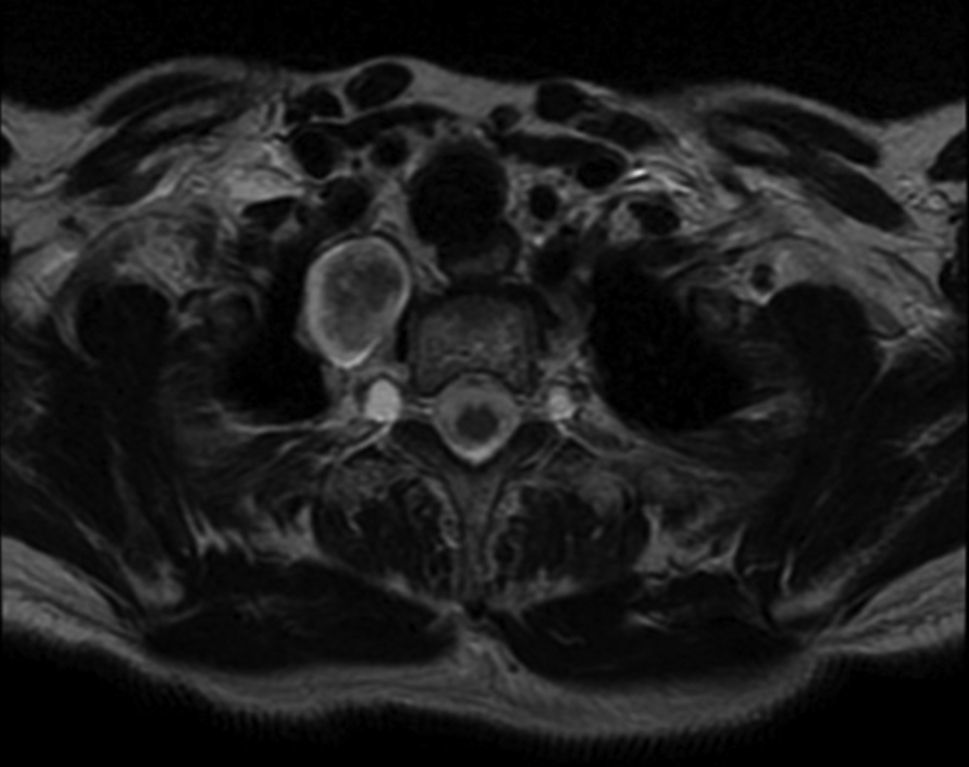
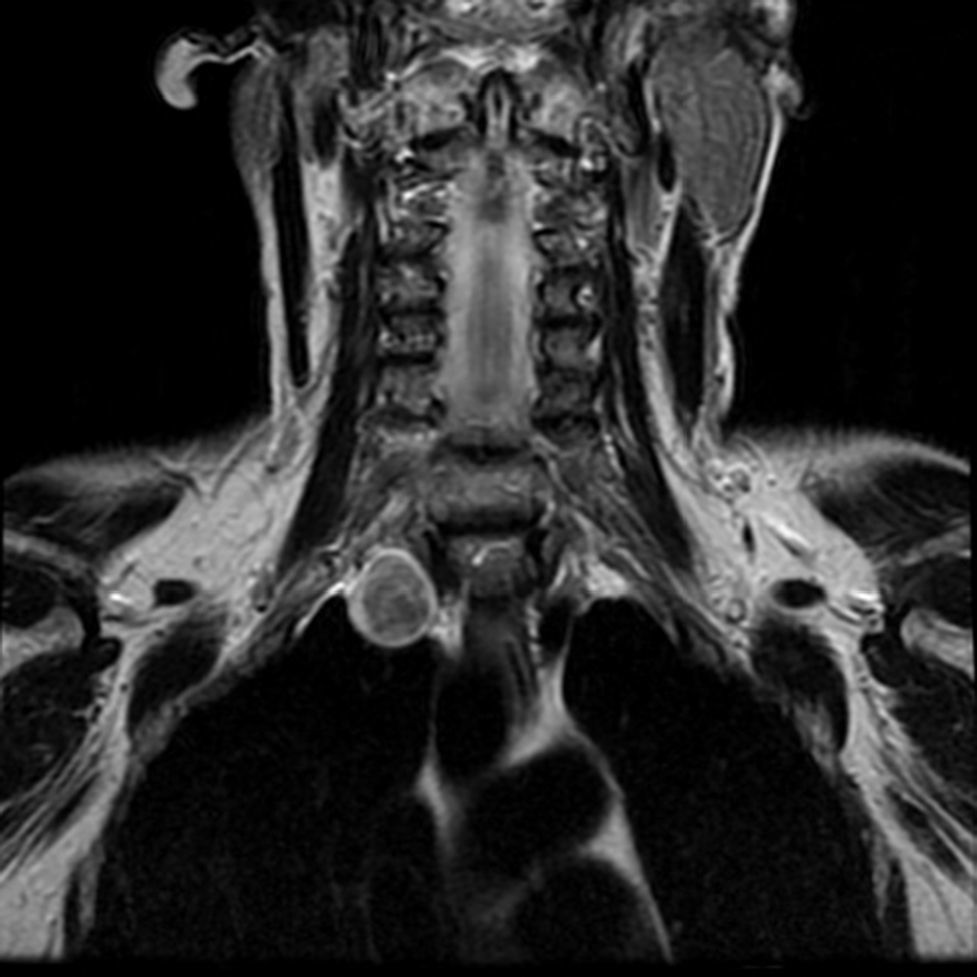
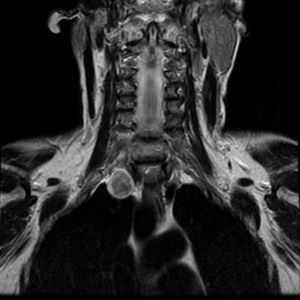
Cervical magnetic resonance with contrast was performed prior to surgery which showed an ovoid lesion of 27mm×19mm×22mm in the right paravertebral location, behind the trachea and lateral to the oesophagus, not touching them, impinging on the parenchyma of the right lung vertex; presenting a slightly hypointense signal on T1 and hyperintense on T2 (Figs. 1 and 2), with intense enhancement which was discreetly heterogeneous with the contrast. Parathyroid gammagraphy was performed after intravenous injection of isonitriles labelled with technetium, without showing uptake in the location shown on magnetic resonance, and cervical computed tomography (Fig. 3) which showed a well-defined tumour, of slightly less than 3cm above the right lung vertex, between the subclavian artery, vertebra C7, and posterior arch of the first rib with fat plane of cleavage with the trachea and the oesophagus. Since there was suspicion of a cervical mass in a patient with primary hyperparathyroidism (suspicion of ectopic adenoma), surgery was performed. A Kocher incision was made; the thyroid gland was explored, which was macroscopically normal: the mass was reached caudally to the lower pole of the right hemithyroid, 2 independent lesions were found, one small in size, and the other a right paravertebral cervical mass of 3m. The preoperative count of calcium was 10.5mg/dl, of phosphate 2.8mg/dl and of parathyroid hormone (HPT) 202pg/ml. After excision of the adenoma, the postoperative levels of calcium were 9.2mg/dl, phosphate 2.8mg/dl and HPT 91pg/ml.
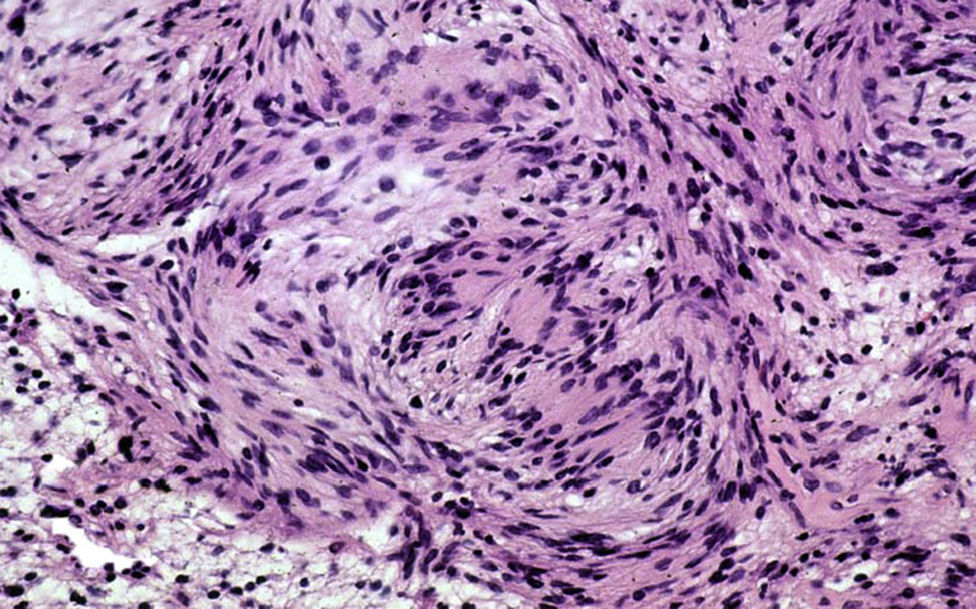
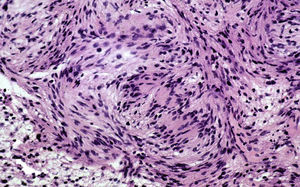
In the postoperative period the patient presented miosis in her right eye, with ptosis and enophthalmos (Fig. 4). The histopathological study showed 2 independent lesions, a parathyroid adenoma weighing 431mg and a schwannoma of 3cm with the remains of a sympathetic ganglion in the periphery (Fig. 5).
The patient evolved well, and was discharged on the third day post-surgery. Twelve months after the intervention, she no longer presented hyperparathyroidism, and had normal calcium levels (around 9.5mg/dl), and normal HPT levels. Magnetic resonance was performed, 1 year after the intervention, which showed no radiological signs of recurrence. The right-sided Horner's syndrome had completely disappeared, and the patient was asymptomatic.
DiscussionTumours deriving from the Schwann cells of nerve sheaths or schwannomas are rare tumours, which can derive from any peripheral nerve, cranial nerve or nerve of the autonomous system. Cervical tumours constitute between 25% and 45% of schwannomas1,5; the most common are those deriving from the spinal nerves or last 4 cranial nerves. When they derive from the cervical sympathetic chain, they are extremely rare and are usually located in the posterior cervical planes.3,6
They tend to be difficult to diagnose; they present as asymptomatic cervical masses, which are slow-growing and generally unilateral. When they do manifest symptoms, such as pain or neurological deficit, this indicates a possibility of malignancy.7,8
It is important to make the correct differential diagnosis with other cervical tumours, such as adenopathies, vagal schwannomas, carotid tumours, metastatic lesions or parathyroid.9 The simultaneous presentation, as in the case shown, of a schwannoma along with a parathyroid adenoma has not been mentioned in the medical literature reviewed. Imaging tests, such as ultrasound, computed tomography and magnetic resonance, can be helpful to guide diagnosis, but are not usually definitive. Schwannomas usually appear as well-delimited tumours, which displace adjacent structures without infiltrating them, and they are not vascularised. In the case presented, the imaging tests appeared compatible with these characteristics (Figs. 1–3), but due to the patient's primary hyperthyroidism, it was assumed that it was an ectopic parathyroid adenoma. Puncture and fine needle aspiration cytology yields little, at around 25%.10
Despite their being benign tumours, with little likelihood of becoming malignant, they are treated by complete surgical resection.3,5 During surgery on the case presented, the presence of two independent tumours was observed, and therefore both were excised. Surgery in most cases involves the resection of a major nerve route, although it would be possible to resect the tumour without damaging the nerve route, and therefore, preserve its function. Nevertheless, the possibilities of neurological damage are significant, the most common sequela being ipsilateral Horner's syndrome, which in most cases is usually permanent.3–5,11 After surgical resection, the patient in our case presented right-sided Horner's syndrome in the immediate postoperative period (Fig. 4), with almost complete recovery 9 months after surgery, and her quality of life was not diminished.
When they are studied histopathologically, schwannomas are usually encapsulated lesions, formed by groups of fusiform cells arranged in 2 patterns as defined by Antoni (A or high cellularity or B low cellularity). On occasion biopsy is not conclusive, and therefore immunohistochemistry is reserved for border-line cases. A positive S-100 protein result, antigen present in the tissues deriving from the neural crest.12,13
The treatment of primary hyperparathyroidism with hypercalcaemia and hypercalciuria, as in the case presented, is surgical resection of the parathyroid adenoma which is secreting parathyroid hormone.14,15 To that end, imaging tests need to be carried out to locate it, which include sestamibi gammagraphy, cervical ultrasound, computed tomography, magnetic resonance or even, positron-emission tomography.14–16 Furthermore, it is important to rule out the association of hyperparathyroidism with other endocrine disorders, as it can be included in type 1 or type 2A multiple endocrine neoplasia (MEN-1 or MEN-2A). In fact it is usually the first manifestation of MEN-1.17 Although, usually the presence of an ectopic adenoma practically rules out the likelihood of a MEN. In MEN-1, hyperparathyroidism is associated with pituitary adenomas and pancreatic tumours (insulinoma, gastrinoma), and in MEN-2A it is associated with medullary thyroid cancer.17,18 In our case, the presence of MEN was ruled out, given the normality of the hormone laboratory levels, and the absence of thyroid tumours on the imaging tests and on surgical exploration of the thyroid. After performing the imaging tests, magnetic resonance and computed tomography in our case, with negative gammagraphy, a right-sided paravertebral mass was observed, with non-specific radiological characteristics, which in a clinical context could be a lower, right-sided parathyroid adenoma. Therefore surgery was indicated and the 2 different lesions were found.
ConclusionsSchwannomas are generally benign tumours which can develop in almost any nerve; cervical sympathetic chain schwannoma should be taken into account in the differential diagnosis of any tumour in the posterior cervical region. Therefore, with a patient with hyperparathyroidism and radiological imaging of an ectopic parathyroid adenoma in the posterior cervical region, the possibility of a cervical sympathetic chain schwannoma should be considered. The synchronous presentation of a parathyroid adenoma with a cervical sympathetic chain schwannoma is not described in the literature we consulted. With this diagnostic suspicion, treatment is surgical resection, and Horner's syndrome is the most common complication.
Conflict of interestsThe authors have no conflict of interest to declare.
Please cite this article as: Manzanedo-Romero I, García-Muñoz-Najar A, Acín-Gándara D, Carrión-Álvarez L, Urbasos-Pascual M, Pereira-Pérez F. Schwannoma de la cadena simpática cervical asociado a adenoma paratiroideo. Cir Cir. 2015;83:409–413.