Pneumomediastinum is the presence of free air around mediastinal structures, which may be spontaneous or secondary, and can occur in 10% of patients with blunt chest trauma, with the Macklin effect being its main pathophysiology.
Clinical caseA 21 year old male, hit by motor vehicle, with alveolopalatal fracture and blunt chest trauma, who, 72h after admission, shows subcutaneous emphysema in the anterior chest. A simple tomography of the chest and abdomen was performed, finding a pneumomediastinum, bilateral pulmonary contusions and pneumoperitoneum. Oesophageal, tracheobronchial or intra-abdominal viscera injuries were ruled out, establishing the cause of pneumomediastinum and pneumoperitoneum due to the Macklin effect. This required conservative management in intensive care unit, with a favourable clinical course and discharged after a 10 day hospital stay.
DiscussionMacklin effect is caused by dissection of air medially along the bronchoalveolar sheath (interstitial emphysema), secondary to alveolar breakdown and extending into mediastinal and other anatomical structures (pneumoperitoneum). It has been documented in blunt trauma, as well as in acute asthma, positive pressure ventilation, or after Valsalva manoeuvres. The imaging method of choice is computed tomography, and its characteristic findings, interstitial emphysema adhering to a bronchus and pulmonary blood vessel.
ConclusionsIn the presence of pneumomediastinum and pneumoperitoneum is necessary to rule out oesophageal and tracheobronchial injury before establishing the Macklin effect as its cause. The diagnosis is made with computed tomography and managed conservatively.
Neumomediastino es la presencia de aire libre en mediastino que puede ser espontáneo o secundario; se presenta en el 10% de los pacientes con trauma contuso de tórax, y su principal fisiopatología es el efecto Macklin.
Caso clínicoHombre de 21 años de edad, arrollado por vehículo automotor, con fractura alveolopalatina y trauma contuso de tórax. A las 72h después de su ingreso, presentó enfisema subcutáneo en tórax anterior, por lo que se le realizó tomografía simple de tórax y abdomen que presentó datos de neumomediastino, contusiones pulmonares bilaterales y neumoperitoneo. Se descarta lesión esofágica, traqueobronquial y de víscera intraabdominal. Se establece como causa del neumomediastino y neumoperitoneo el efecto Macklin. Es manejado conservadoramente en la unidad de cuidados intensivos, con adecuada evolución clínica y es egresado al décimo día de estancia hospitalaria.
DiscusiónEl efecto Macklin es causado por la disección de aire medialmente a lo largo de la vaina broncoalveolar (enfisema intersticial), y es secundario a la rotura alveolar, que se extiende al mediastino y a otras regiones anatómicas (neumoperitoneo). Se ha documentado en trauma contuso, crisis asmática, ventilación con presión positiva o después de maniobras de Valsalva. El estudio diagnóstico de elección es la tomografía computada y sus hallazgos característicos son la presencia de enfisema intersticial adherente a bronquio y a los vasos sanguíneos pulmonares.
ConclusionesAnte la presencia de neumomediastino y neumoperitoneo, es necesario descartar lesión esofágica y traqueobronquial, antes de establecer el efecto Macklin como su causa. El procedimiento de elección para su diagnóstico es la tomografía computada y se maneja conservadoramente.
Pneumomediastinum is defined as the presence of free air around the mediastinal structures, also known as mediastinal emphysema. It can be divided into 2 groups: spontaneous, with no obvious primary cause; and secondary, with a triggering pathological event, first described by Laennec.1
According to Kelly et al.2 the first series of cases on spontaneous pneumomediastinum was conducted by Louis Hamman in 1939, hence its being termed Hamman's syndrome. The pathophysiological process was demonstrated experimentally by Macklin and Macklin in 1944, known as the Macklin effect. Its fundamental mechanism is alveolar breakdown secondary to pressure gradients which cause air to leak into the interstitium and the pulmonary lymph nodes (interstitial emphysema), which dissects through the interlobar septums adjacent to the blood vessels and bronchial system until it reaches the hilum, then the mediastinum and other anatomical regions.3
Pneumomediastinum can present in 10% of patient with blunt chest trauma, and the Macklin effect can be attributed as the cause. Tracheobronchial injury presents in fewer than 10% and oesophageal injury presents in a lower percentage.4
We report the case of a patient with blunt chest trauma who presented with pneumomediastinum and pneumoperitoneum secondary to the Macklin effect, managed medically by the General Surgery Department in the Hospital General de Zona Norte, Ministry of Health, Puebla.
Clinical caseA 21-year-old male, originating from and resident of Tlaxcala, with no history of degenerative chronic disease, previous surgery, allergies or drug abuse.
His condition started after being hit by a motor vehicle; the kinematics of the trauma was not known. On admission to the Emergency Department his vital signs were: blood pressure 130/75mmHg; heart rate 95beats per minute; respiratory rate 26breaths per minute; temperature 37°C, Glasgow 15; reduced mouth opening; no enlarged neck lymph nodes; presence of a rigid collar; no alterations to the surface of the chest; no crepitus or subcutaneous emphysema; pulmonary fields with adequate transmission of vesicular murmur; rhythmic heard sounds with no additional sounds; flat abdomen, palpable, with no pain on superficial or deep palpation, no involuntary muscle resistance, peristalsis present and normal.
Laboratory test reports on admission showed: haemoglobin 15g/dl; haematocrit 43%; leukocytes 11,000; neutrophils 82%; bands 6%; platelets 300,000; prothrombin time 16s; partial thromboplastin time 28s, glucose 110mg/dl; creatinine 1mg/dl; sodium 140mEq/l; potassium 3.5mEq/l; chlorine 115mEq/l. Chest X-ray showed no signs of haemothorax or pneumothorax, no lesions in bony structures or soft tissues; simple abdominal plates normal; eco-FAST with no fluid in the pericardium or intra-abdominal fluid; plain computed tomography (CT) of the skull, showing alveolopalatal fracture.
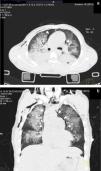
It was decided to refer the patient to the Maxillofacial Department for surgery, 48h after admission, for open reduction internal fixation of the alveolopalatal fracture. During the immediate postoperative period he went into respiratory failure, underwent orotracheal intubation for mechanical ventilation support, and was sent to the intensive care unit. A repeat chest X-ray was performed which revealed the presence of multiple bilateral infiltrates associated with pulmonary contusion and an image suggestive of pneumopericardium (Fig. 1).
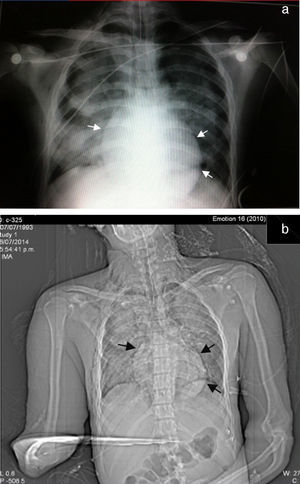
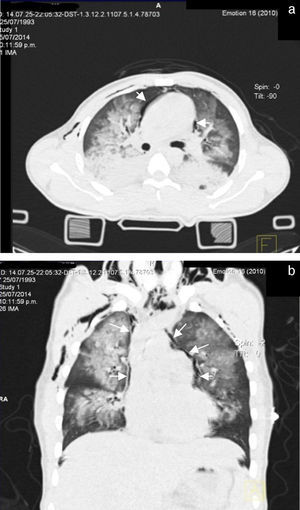
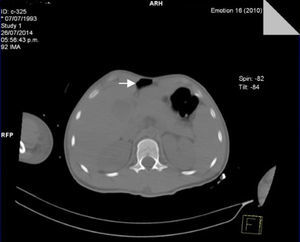
Seventy-two hours after admission, the patient presented subcutaneous emphysema in the anterior chest extending to the neck, a simple CT scan was performed of the chest and abdomen which revealed a pneumomediastinum, bilateral lung contusions and pneumoperitoneum (Figs. 2 and 3). He continued on mechanical ventilation. Oesophageal injury was ruled out by oesophagogram with water-soluble contrast medium, and flexible bronchoscopy ruled out tracheobronchial injury. Furthermore, no signs of peritoneal irritation were found, therefore the Macklin effect was established as the cause of the pneumomediastinum and pneumoperitoneum.
On the sixth day, the patient presented clinical improvement with resolution of the subcutaneous emphysema and X-ray control showed a reduction in the bilateral pulmonary infiltrates.
On the seventh day the patient came off mechanical ventilation, due to his satisfactory clinical progress and was discharged from the intensive care unit. He continued to be cared for in the General Surgery Department and he was discharged in a satisfactory general condition on the tenth day.
DiscussionSeveral studies have shown that spontaneous pneumomediastinum occurs predominantly in young, previously healthy, tall, thin males (14:3, compared to females), in an age range from 12 to 35. In females, it predominates during pregnancy and childbirth in particular. It is associated with an increase in intrathoracic pressure, due to Valsalva manoeuvres,2,5,6 and has an incidence of 1 per 800–32,000 hospital admissions due to accidents.2,7
Pneumomediastinum can also be categorised as atraumatic (20%) or traumatic (80%).8 Traumatic pneumomediastinum can be blunt (86%) or penetrating (14%)8 or due to iatrogenic injury, such as those caused by mechanical ventilation or endoscopic procedures.9
Pneumomediastinum can present in up to 10% of blunt cervical and chest trauma, most commonly as a result of high speed motor vehicle accidents. The main cause is the so-called Macklin effect, although it can also be secondary to tracheobronchial (6%) or oesophageal (0.1–1.6%) injury.10 In our case, the patient presented blunt chest trauma due to impact at high speed, it was possible to rule out tracheobronchial or oesophageal injury by extension studies, and it was associated with the Macklin effect.
The Macklin effect was first described in 1939, and is caused by the dissection of air medially along the bronchoalveolar sheath (interstitial emphysema), secondary to alveolar breakdown and extending into the mediastinal and other anatomical structures (pneumoperitoneum). It has been documented in blunt trauma, as well as in acute asthma, respiratory infections, during childbirth, positive pressure ventilation, or after Valsalva manoeuvres, where the main predisposing factor is an increase in intrathoracic pressure.5,11 It has been associated with physical activity such as diving, basketball, football and volleyball5; other associated factors include: smoking, drug consumption (cocaine), dermatomyositis, idiopathic pulmonary fibrosis, Marfan syndrome and diabetic ketoacidosis. The triggering factor is determined in 38–54% of cases, and remains unknown in up to 51%.12
Interstitial emphysema presents in 3 ways: (a) acute, (b) persistent, and (c) persistent diffuse. The acute form is most common in neonates with pulmonary hypoplasia, due to aspiration of meconium or due to hyaline membranes which require high inspiratory pressure ventilation. In adults it presents with barotrauma secondary to dynamic hyperinflation and in disorders characterised by an increased pressure gradient secondary to linear tears along the alveolar septa and the terminal bronchus. In the diffuse and persistent diffuse forms it is associated with bronchopulmonary dysplasia, the anatomical substrate being the cystic lesions that range from millimetres to 3cm.3
Associated injuries are often found and are associated with the kinematics of the trauma, and do not directly relate to the Macklin effect. These include craneoencephalic trauma (29–49%), cardiovascular injuries (19–30%), unstable thorax or sternal fractures (9.5–20%). A mortality of around 10% is reported.13
The triad that is generally found comprises (1) retrosternal chest pain radiating to the neck, shoulder or back (80–90%), (2) dyspnoea (50%), and (3) subcutaneous emphysema (>90%).2,13
Hamman's sign (described in 1939, by Hamman) presents in 18% of patients and is characterised by a retrosternal “crunching” on auscultation, synchronous with the heartbeat.10,13 Other less common symptoms are: cough (36%), dysphagia (18%); sporadic complaints such as: odynophagia, lightheadedness, weakness, dysphonia, nasal tone in speech (rhinolalia) and epigastralgia.9
Physical examination can be normal in up to 30% of cases10 and it can often manifest with a fever of above 38.5°C and leukocytosis, with polymerase chain reaction (PCR) above 5mg/l (41–68%).12,14 In our case, the only symptom presented was subcutaneous emphysema in the anterior chest radiating to the cervical region, although the patient was put on mechanical ventilation when this occurred. Subcutaneous emphysema can be very extensive and be associated with complications, which are not only of an aesthetic nature, there can also be visual disturbance due to periorbital tumefaction, dysphonia or dyspnoea due to cervical spread associated with compression of the upper airway and even pacemaker dysfunction. The most serious complication is probably massive chest compression with acute respiratory failure and cardiac pseudo-tamponade, associated with pneumomediastinum and pneumopericardium, respectively.15
All trauma patients should be assessed and managed according to the Advanced Trauma Life Support protocols (ATLS), developed by the American College of Surgeons (ACS).
In the event that a pneumomediastinum is suspected, the initial laboratory study is frontal and lateral chest X-ray, including the cervical region; this study will reveal the pneumomediastinum in 90% of cases.9 The radiographic signs suggestive of a pneumomediastinum include a radiolucent line which outlines the mediastinal structures (most evident cranial to heart on the left side), lifts the mediastinal pleura and often extends to the neck or the chest wall. On a lateral projection, this radiolucent line can outline the aortic arch, the retrosternal, precardiac, periaortic and peritracheal areas. Other radiographic signs include “continuous diaphragm sign”, which is mediastinal gas outlining the upper surface of the diaphragm and separating it from the heart; “Naclerio's V sign”, which presents gas outlining the lateral edge of the descending aorta and which extends laterally between the parietal pleura and the medial portion of the left hemidiaphragm, and the “ring around the artery sign” where the gas surrounds the mediastinal extrapericardial portion of the right pulmonary artery.10,13
Indirect radiographic signs include thoracic and cervical subcutaneous emphysema, pneumopericardium, pneumoretroperitoneum and pneumoperitoneum. The presence of a pneumothorax should be deliberately sought; this can be present in 84% of patients. The presence of a penumothorax in patients with pneumomediastinum does not necessarily indicate injury to an organ of the mediastinum; in fact it is a strong negative indicator of oesophageal injury or association with injury to the airway.10 In the clinical case that we present, there was evidence of pneumomediastinum associated with a pneumothorax, with no demonstrated oesophageal or airway injury.
In cases where the chest X-ray is normal (fewer than 10%), the study of choice is CT, which is considered the gold standard, even in patients with suggestive radiological findings.1,10 The Macklin effect appears as a linear collection of air contiguous with the bronchovascular sheath and the characteristic findings of interstitial emphysema due to the Macklin effect present as a triad: (1) interstitial emphysema, (2) to the bronchus, and (3) to the pulmonary blood vessel.3,16 CT has high sensitivity to pneumomediastinum and pneumoperitinoneum (>95%) and specificity (>85%) in order to rule out major injury to the aerodigestive tract. However, the possibility of an oesophageal or tracheal injury should always be ruled out using other diagnostic methods.10
The presence of a pneumoperitoneum is generally associated with perforation of the hollow viscera and therefore requires emergency surgery; in 5–15% of cases it is not the result of visceral perforation and most of the time is associated with medical interventions.17 Mularski et al.17 identified 2 groups as non-surgical causes of pneumoperitoneum: (1) abdominal cause (post-operative air, peritoneal dialysis, endoscopic gastrointestinal procedures), and (2) thoracic cause (mechanical ventilation, cardiopulmonary resuscitation, lung trauma injuries, pneumothorax) which indicate that when abdominal pain and distension are minimal, and when peritoneal signs, fever and leukocytosis are absent, nonsurgical causes should be considered.17,18
Treatment is conservative and symptomatic, with spontaneous resolution in 3–15 days (average days of hospitalisation from 3.5 to 4.5). Management involves rest, appropriate analgesia and avoiding manoeuvres (Valsalva or forced expiratory) that increase lung pressure; the use of antibiotics is not necessary, unless associated with an aerodigestive tract injury.2,10,13 Treatment with pure oxygen increases the diffusion pressure of nitrogen in the interstitium and promotes rapid absorption of the free air.9 Our patient required management by the intensive care unit. He was managed conservatively and made satisfactory clinical progress, with no subsequent complications, and therefore was discharged 10 days after the trauma.
Chassagnon et al.14 proposed 5 parameters to select patients eligible for treatment as outpatients and thus avoid unnecessary hospitalisation: (1) patients with a fever higher than 38°C, (2) oxygen desaturation under 96%, (3) progressive and incapacitating symptoms, (4) vomiting at the onset, and (5) anxiety.
Recurrence of this complication is an exceptional event; very few cases are described in the literature. It is thought that recurrence is caused by persistence of the predisposing factor (asthma, pneumonia, interstitial lung disease), or when the causative situation reoccurs.12,19
ConclusionsSpontaneous pneumomediastinum and pneumoperitoneum is a very rare clinical condition, where oesophageal and trachobronchial injury must be ruled out before the Macklin effect can be suspected as its pathophysiological cause. The gold standard for diagnosis is CT scan and the condition requires conservative management alone, because it is self-limiting.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Carzolio-Trujillo HA, Navarro-Tovar F, Padilla-Gómez CI, Hernández-Martínez IA, Herrera-Enríquez J. Trauma contuso de tórax con neumomediastino y neumoperitoneo secundario a efecto Macklin. Reporte de un caso. Cir Cir. 2016;84:409–414.