Hypercalcaemia due to primary hyperparathyroidism is a rare cause of acute pancreatitis, with a reported prevalence of 1.5–8%. There is no clear pathophysiological basis, but elevated parathyroid hormone and high serum calcium levels could be responsible for calcium deposit in the pancreatic ducts and activation of pancreatic enzymes, which may be the main risk factor for developing acute pancreatitis. The aim of this report is to describe four cases.
Clinical caseFour cases are reported of severe pancreatitis associated with hypercalcaemia secondary to primary hyperparathyroidism; three of them were with complications (two pseudocysts and one pancreatic necrosis). Cervical ultrasound, computed tomography, and scintigraphy, using 99mTc-Sestambi, studies showed the parathyroid adenoma. Surgical resection was the definitive treatment in all four cases. None of the patients had recurrent acute pancreatitis events during follow-up.
ConclusionsAcute pancreatitis secondary to hypercalcaemia of primary hyperparathyroidism is rare; however, when it occurs it is associated with severe pancreatitis. It is suspected in patients with elevated serum calcium and high parathyroid hormone levels. Imaging techniques, such as cervical ultrasound, computed tomography, and scintigraphy, using 99mTc-Sestambi, should be performed, to confirm clinical suspicion. Surgical resection is the definitive treatment with excellent results.
La hipercalcemia secundaria a hiperparatiroidismo primario es una causa rara de pancreatitis aguda, con una prevalencia documentada de 1.5 a 8%. La pérdida del mecanismo regulador de paratohormona y la hipercalcemia favorecen el depósito de calcio en los conductos pancreáticos y la activación de enzimas pancreáticas son probablemente los factores precipitantes. El objetivo de este informe es describir 4 casos.
Caso clínicoCuatro pacientes con diagnóstico de pancreatitis aguda severa asociada con hipercalcemia secundaria a hiperparatiroidismo primario, tres de ellos con complicaciones asociadas a pancreatitis (dos con pseudoquiste y uno con necrosis pancreática). El ultrasonido de cuello, la tomografía de cuello y la gammagrafía con Tc-99 sestamibi confirmaron la presencia de un adenoma de paratiroides. La resección quirúrgica del adenoma fue el tratamiento definitivo, con excelentes resultados sin nuevos episodios de pancreatitis o hipercalcemia durante su seguimiento.
ConclusionesLa pancreatitis aguda por hipercalcemia secundaria a hiperparatiroidismo primario es infrecuente; sin embargo, cuando ocurre se asocia a pancreatitis severa. Su sospecha es en pacientes con elevación sostenida de calcio y paratohormona cuando se han descartado otras causas frecuentes. La confirmación diagnóstica se realiza con ultrasonido de cuello, tomografía de cuello o gammagrafía con sestamibi. La resección quirúrgica del adenoma es el tratamiento definitivo con resultados excelentes y cese de recurrencias de pancreatitis aguda.
Primary hyperparathyroidism is a disorder of calcium metabolism that results from an abnormally high level of serum calcium, and an increase in parathyroid hormone. Primary hyperparathyroidism is the most common cause of hypercalcaemia. It can appear at any age; however, in most cases, it is reported over the age of 45, with predominance in females in the ratio of 2:1.1
Hypercalcaemia caused by primary hyperparathyroidism is a rare cause of acute pancreatitis, with a documented predominance of 1.5–8%. However, less than 1% of the patients who suffer from acute pancreatitis have primary hyperparathyroidism.1,2 According to Egea,1 the association between primary hyperparathyroidism and acute pancreatitis was described by Erdheim in 1903, while the association with chronic pancreatitis was published by Martin and Canseco in 1947. However, it was not until 1957 when Cope et al. considered it as another sign of primary hyperparathyroidism.1,2
Patients with primary hyperparathyroidism and hypercalcaemia have up to 10 times more risk of suffering from acute pancreatitis episodes (approximately 2%). The association between hypercalcaemia and certain genetic mutations (gene SPINK 1 (Kazal-type serine protease inhibitor type 1), CFTR (cystic fibrosis transmembrane conductance regulator gene) and CASR (calcium receptor gene)) could be responsible for this predisposition in some patients with hyperparathyroidism.1–4
Although the association between these entities is well described and many theories about their pathogenesis have been proposed, there are few references on acute pancreatitis cases associated with hypercalcaemia and hyperparathyroidism in medical literature. The most common scenario is when they appear in an already known hyperparathyroidism context or during a parathyroidectomy postoperative period; it is more infrequent as an initial sign of a patient suffering from hyperparathyroidism.1–4
We report four cases of acute pancreatitis caused by hypercalcaemia due to primary hyperparathyroidism that was not known previously.
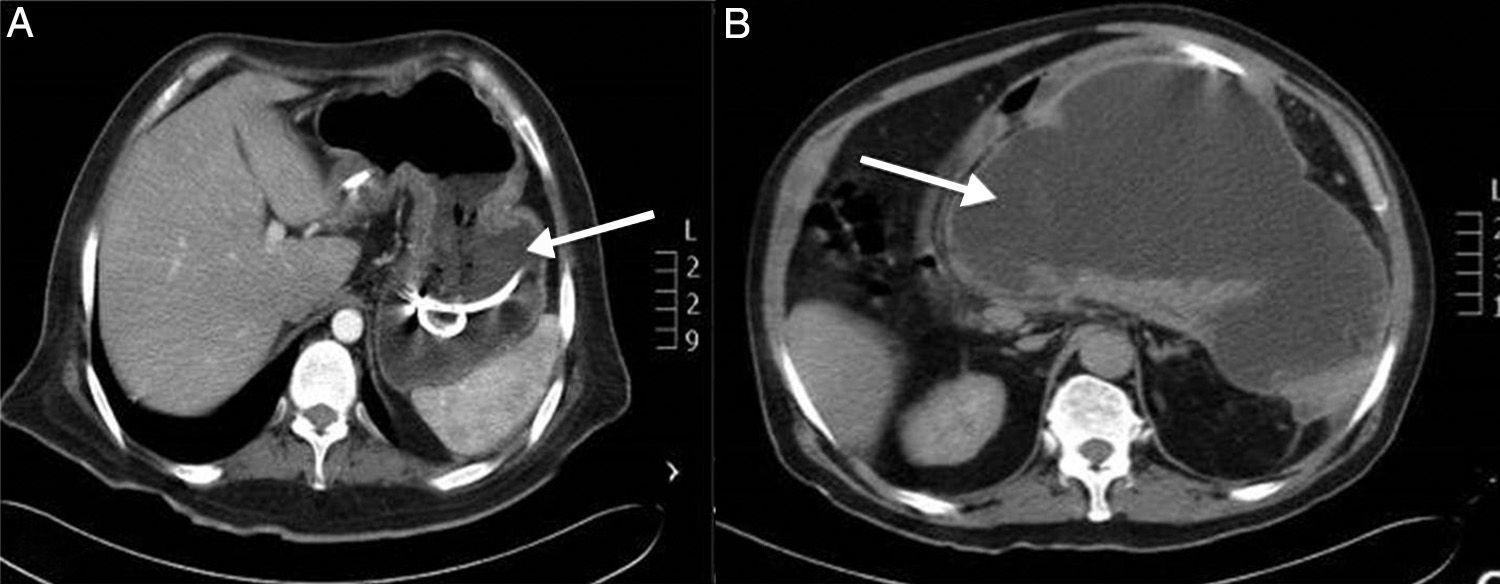
Clinical casesCase 1A 28-year-old male patient with a history of bronchial asthma, diabetes mellitus and amygdalectomy during infancy. He presented with recurrent abdominal pain, which led to three hospital admissions where he was diagnosed with severe acute pancreatitis, with no aetiologic diagnosis. A pancreatic pseudocyst was documented during his last admission; he was sent to our unit for this reason. During physical examination, he was dehydrated and had abdominal pain located at the epigastrium. Laboratory reports at the time of admission showed: haemoglobin 12.1g/d, leukocytes 13,000μl (64.5% neutrophils), plasma amylase 108U/l, lipase 199U/l, glucose 209mg/dl, calcium 14.2mg/dl and phosphorus 2.0mg/dl. The abdominal tomography and the endoscopic ultrasound reported a pseudocyst in the tail and head of the pancreas, which was drained endoscopically through a transgastric method. Patient evolved adequately and was discharged due to improvement (Fig. 1A).
He was readmitted five days later due to fever, anorexia, asthenia, adynamia, nausea, vomiting and abdominal pain at the epigastrium, which irradiated to the right hypochondrium. Laboratory analysis reported normal levels of amylase and lipase. However, serum calcium level was 14.8mg/dl. Thus, a new analysis of serum calcium and parathyroid hormone levels was performed, of which values were 14.3mg/dl and 712pg/ml, respectively (normal value under 9pg/ml). The diagnosis of hypercalcaemia caused by hyperparathyroidism was confirmed. The neck ultrasound and the scintigram with Tc-99 sestamibi showed the presence of an adenoma in the lower right parathyroid gland of approximately 1.4×1.3. A lower right parathyroidectomy was performed; the histopathological result corresponded to a parathyroid adenoma with a nodular pattern of 1.4cm×1cm×0.4cm, after which parathyroid hormone and serum calcium levels decreased to 6pg/ml and 10.2mg/dl, respectively. Patient evolved well and was discharged due to his improvement without having another hypercalcaemia episode. However, after two months of being discharged, he presented with a hydrocholecyst and a pancreatic pseudocyst, which were treated by means of an open cholecystectomy and a cystogastroanastomosis, respectively. Evolution was favourable and the patient was discharged due to his improvement.
Case 2A 50-year-old female patient with a history of systemic high blood pressure, left otitis media with cholesteatoma and radical left mastoidectomy. She had surgery for acute abdomen where a haemorrhagic necrotic pancreatitis was documented, handled by means of drainage of the abdominal cavity, a cholecystectomy and a biliary-duct examination with a T-tube. She had a haemorrhagic vascular episode in the parietooccipital region and cerebral oedema, which is why she was sent to the intensive care unit. Laboratory analysis at the time of admission reported normal levels of amylase and lipase, leukocytes 15,000 (86% neutrophils), 10.1g/dl anaemia, and serum calcium 9.2mg/dl. The case was handled conservatively and the patient was discharged from the intensive care unit after 10 days. An abdominal tomography was performed, which reported severe pancreatitis, Baltazar Grade E. Laboratory results showed normal levels of amylase and lipase. However, a 12.9mg/dl hypercalcaemia and 1.9mg/dl hypophosphataemia were documented. A new analysis of serum calcium and parathyroid hormone levels was performed, showing values of 11.6mg/dl and 684pg/ml, respectively. The diagnosis of hypercalcaemia caused by hyperparathyroidism was confirmed. The neck tomography and ultrasound showed an upper right parathyroid-dependant tumour of approximately 3cm. A lower right parathyroidectomy was performed with right hemithyroidectomy, through which a 3cm×3cm tumour was discovered; the histopathological report was lower right parathyroid adenoma. Parathyroid hormone levels decreased during the immediate postoperative period; the patient's evolution was also favourable. Following this episode, the patient did not have any more hypercalcaemia or pancreatitis symptoms at subsequent check-ups.
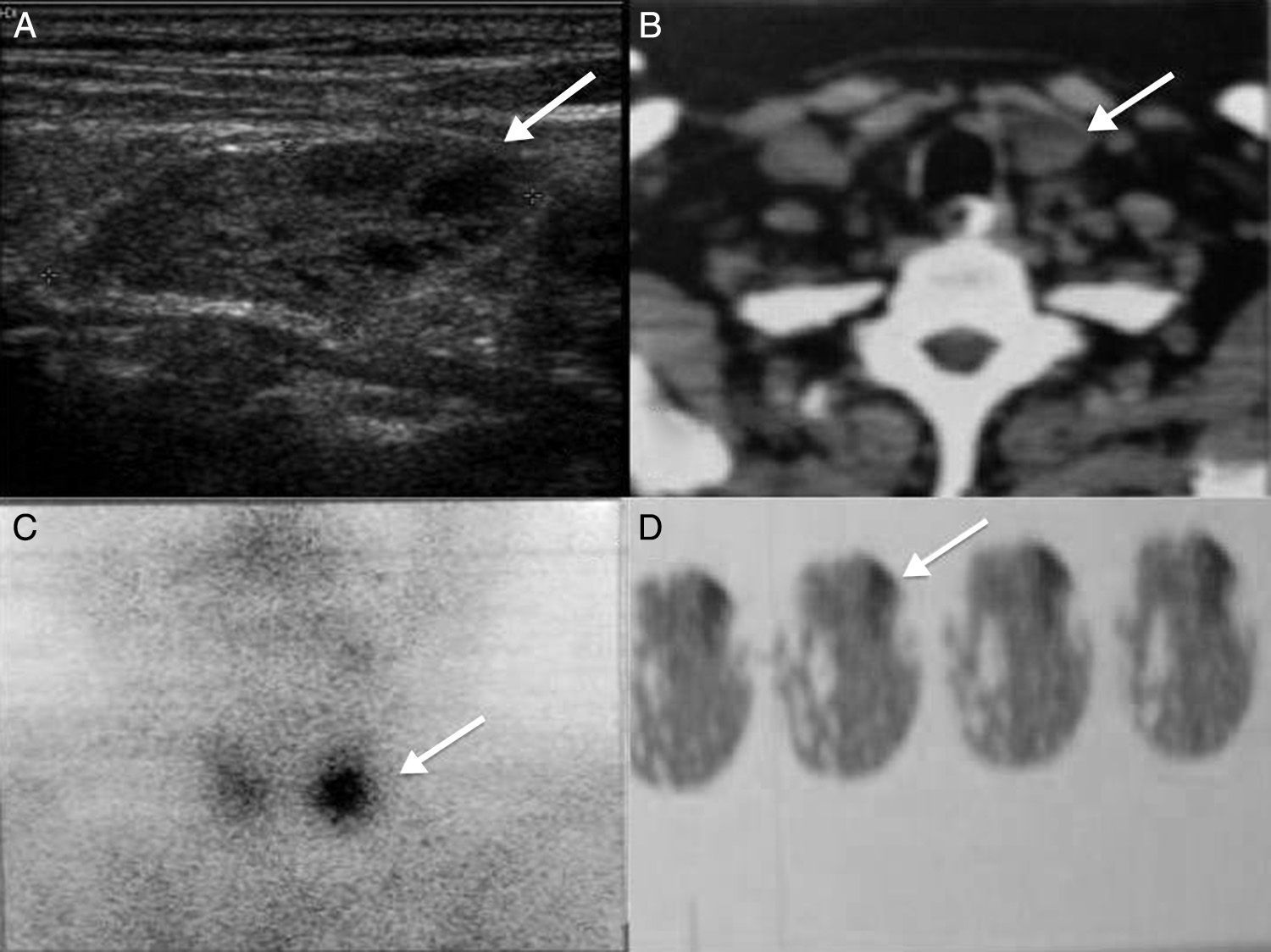
Case 3A 54-year-old male patient with a history of uncontrolled diabetes mellitus, alcoholism and 25 years of intense tobacco use. He presented with recurring abdominal pain located at the epigastrium, which radiated to the right hypochondrium, combined with nausea, vertigo and photophobia. Two hospital admissions found high levels of amylase and a pancreatitis diagnosis. During his last admission, a cystic lesion in the pancreas was reported by means of an abdominal tomography, which prompted him being sent to our unit. The abdominal tomography reported a 10cm×20cm lesion in the tail and head of the pancreas, with an average attenuation of 9 UH, compatible with a pancreas pseudocyst (Fig. 1B). Laboratory results reported increased levels of amylase and lipase of 539U/l and 180U/l respectively, 9.2mg/dl anaemia, serum calcium 12.3mg/dl, and phosphorus 2.84mg/dl. Due to the increase in serum calcium, the levels of calcium and parathyroid hormone were analysed again, finding values of 11.1mg/dl and 235pg/ml, respectively. The neck ultrasound reported a lower left parathyroid gland tumour of 3.4cm×1.6cm×2.4cm, and cystic degeneration areas with hyperechogenic regions (Fig. 2A). The SPECT-CT scan showed an absorption area compatible with lower left parathyroid adenoma (Fig. 2B–D). The patient underwent a Roux-in-Y cystojejunoanastomosis and a pancreatic necrosectomy after his levels of amylase and lipase returned to normal. When the symptoms were completely tackled, the patient underwent lower left parathyroidectomy surgery, through which a lesion of 4cm×2cm was found in his lower parathyroid gland. The decrease in serum calcium levels and the normalisation of parathyroid hormone levels were confirmed during surgery. Pathological anatomy results confirmed the presence of a parathyroid adenoma. The patient evolved adequately and was discharged due to his improvement. During his follow-up consultations, he has not presented new symptoms of pancreatitis or hypercalcaemia.
Case 3. (A) Neck ultrasound where 3.4×1.6×2.4 lower left parathyroid tumour can be seen, heterogeneous, hyperechogenic areas with cystic degeneration (arrow). (B) Neck tomography with lower left parathyroid-dependant tumour (arrow). (C) and (D) SPECT-CT that shows hyperabsorption area in lower left parathyroid gland (arrow).
A 36-year-old male patient with no relevant pathological history. He presented with recurrent abdominal pain, which led to two admissions into the intensive care unit, where he was diagnosed with severe acute pancreatitis, with no aetiologic diagnosis. During his last admission, his levels of plasma calcium and parathyroid hormone were 13.6mg/dl and 612pg/ml, respectively. The neck ultrasound did not show alterations. However, the Tc-99 sestamibi scintigram showed the presence of an ectopic parathyroid adenoma located in the left paratracheal space, at C5 level and posteromedial to the common carotid. A resection was performed; the histopathological result corresponded to an ectopic parathyroid adenoma, after which parathyroid hormone and serum calcium levels decreased to 32pg/ml and 8.2mg/dl, respectively. The patient evolved favourably and was discharged due to his improvement without having other hypercalcaemia episodes.
DiscussionAcute pancreatitis has a great variety of aetiologies. Among these, alcohol and biliary lithiasis cause between 80% and 90% of the cases. Other causes are related to toxics or drugs, neoplastic obstructions of the bile duct or of the sphincter of Oddi, and metabolic alterations such as hypertriglyceridaemia or hypercalcaemia, trauma or mechanic lesions, ischaemic processes, infections and autoimmune diseases, among others. In 10% of the cases the cause cannot be determined and they are regarded as idiopathic.1
Hyperparathyroidism and hypercalcaemia states represent an infrequent cause for the onset of acute pancreatitis. Large series, such as the one from Bess5 and Carnaille et al.6 marked a 1.5% and 3.2% incidence, respectively.
Primary hyperparathyroidism affects between 0.2% and 0.5% of the population. It is sporadic for 90% of the population and familial in only 10%, and it is part of multiple neuroendocrine syndromes (multiple endocrine neoplasia I and II). A single parathyroid adenoma affects 85% of the cases. 10% of the cases involve parathyroid hyperplasia of the four glands, and there are multiple adenomas in only 4% of the cases. Other causes for primary hyperparathyroidism include parathyroid cancer and cysts. However, this only occurs in 3% of the cases.4,7–9
Although a clear physiopathological base could not be established, everything indicates that the association between acute pancreatitis and primary hyperparathyroidism is not coincidental, and the levels of calcaemia would be the main development factor. Reeve and Delbridge10 reported a predominance of acute pancreatitis in 9% in patients who had had parathyroidectomy surgery.2 The proposed physiopathology is the loss of the regulatory mechanism of the parathyroid hormone, which leads to a hypercalcaemia state that mediates the activation of trypsinogen to trypsin, which causes the autodigestion of the gland and favours the forming of calcium deposits in the pancreatic ducts. The direct effect of the parathyroid hormone and the accumulation of calcium would generate an accumulation of autophagocytic vesicles, which would have a decisive role in acute pancreatitis.1–3,11,12 Sustained hypercalcaemia increases the content of calcium in the pancreatic juice, resulting in an accelerated transformation of trypsinogen to trypsin, with a morphologic alteration of the pancreas and acute hyperamylasemia.1,2
The diagnosis for hypercalcaemia-related pancreatitis caused by primary hyperparathyroidism has decreased over time from 12% to 1%, since the diagnosis for primary hyperparathyroidism is now achieved at an earlier stage due to the measurement of calcium by autoanalysers.11
Usually, acute pancreatitis is associated with a decrease in serum calcium and constitutes a prognosis factor during the case's first 48h (Ranson). Therefore, the presence of hypercalcaemia increases the diagnostic suspicion of hyperparathyroidism or of malignancy. The biochemical scenario shows hypercalcaemia, hypophosphatemia, hypercalciuria and an increase in parathyroid hormone levels. The risk of acute pancreatitis with calcium values over 14mg/dl is of 25%.2,3 In our report, we observed an increase in serum calcium above 12mg/dl hypophosphatemia and an increase in parathyroid hormone levels in all cases. In three cases, acute pancreatitis was reported, which required surgical treatment to manage it; this could be through a necrosectomy or by draining the pseudocyst.
As we did with our patients, the preoperative identification of the parathyroid adenoma is performed by means of a neck ultrasound, neck tomography or scintigram with sestamibi. The last has the advantage of documenting ectopic locations.7,8,11,13 Adenoma resection is indicated for patients with symptomatic primary hyperparathyroidism or for those who are asymptomatic and comply with one or more of the international criteria for the treatment of patients with asymptomatic primary hyperparathyroidism: serum calcium levels over 1mg/dl above the upper normal calcium range, creatinine clearance lower than 60ml/min, bone density in hips, spine or distal radius over 2.5 standard deviations below peak bone density (T score below 2.5), a history of or a risk of fractures, and being under the age of 50.7,11
A definite treatment is the surgical removal of the parathyroid adenoma; this cures 100% of the cases according to medical literature reports. Parathyroid hormone values immediately become normal after the removal of the adenoma and this can be confirmed intraoperatively. Related symptoms lessen immediately after removal.7,11,13 Surgical removal of the parathyroid adenoma normalised the levels of serum calcium and parathyroid hormone in the reported cases; none of the patients had a new episode of pancreatitis during the follow-up period. Complications associated with pancreatitis (for example, a pseudocyst) were handled without complications.
ConclusionsAlthough patients with hypercalcaemia caused by hyperparathyroidism are not frequent, we observed that it is associated with severe pancreatitis both in medical literature and in our revision. We found that the diagnostic imaging method could be performed using conventional imaging methods from literature (neck ultrasound, neck tomography or scintigram with sestamibi). Clinical presentation must remain under review when there is a sustained increase in calcium and parathyroid hormone levels and when the most common causes for pancreatitis have been ruled out. Surgical removal represents the definitive management and succeeds in preventing acute pancreatitis recurrences.
Conflict of interestsThe authors declare that there are no conflicts of interest.
Please cite this article as: Tun-Abraham ME, Obregón-Guerrero G, Romero-Espinoza L, Valencia-Jiménez J. Pancreatitis aguda asociada con hipercalcemia. Cir Cir. 2015;83:227–31.