Augmentation cystoplasty is a successful surgical procedure for the management of neurogenic bladder in children in order to improve urodynamic parameters.
The aim of this article is to describe urodynamic changes after augmentation cystoplasty in children with myelomeningocele.
Materials and methodsA descriptive cross-sectional study including children aged 8–16 years with a myelomeningocele operated on for augmentation cystoplasty surgery with sigmoid colon segments due to a neurogenic bladder from the years 2003–2013. A urodynamic study was conducted before and after the surgical procedure. Non-probabilistic sample of consecutive cases. Descriptive statistics with frequencies and percentages, medians, and ranges. Inferential intra-group comparison with the Wilcoxon test and inter-group with Mann–Whitney U. SPSS 20.0 statistical package.
ResultsThe study included 50 patients, of whom 25 were male and 25 were female, with a median age of 12 years (range, 6–15 years). Bladder capacity improved from 52.8% to 95.9% (p<0.001), uninhibited contractions 1.4–1.8, contraction intensity 47–8.5 (p<0.001), mean pre-surgical and post-surgical filling pressure 40.8cmH2O and 11.0cmH2O, respectively (p<0.001), mean emptying pressure 48.5 vs. 3.6cmH2O (p<0.001), and bladder accommodation 4.6 vs. 41.3cmH2O (p<0.001).
ConclusionsAugmentation cystoplasty with sigmoid colon significantly improved urodynamic parameters, such as bladder accommodation and filling pressure in children with myelomeningocele-associated neurogenic bladder.
La cistoplastia de aumento es una cirugía exitosa para el manejo de vejiga neurogénica en niños, por mejorar los parámetros urodinámicos.
El objetivo del estudio es describir los cambios urodinámicos posteriores a cistoplastia de aumento en niños con mielomeningocele.
Material y métodosEstudio transversal, descriptivo, que incluyó a niños de 8 a 16 años con mielomeningocele, operados de cistoplastia de aumento con colon sigmoides por vejiga neurogénica del 2003 al 2013. Se realizó un estudio urodinámico previo y posterior a la cirugía. Muestreo no probabilístico de casos consecutivos. Estadística descriptiva con: frecuencias, porcentajes, medianas y rangos. Inferencial intragrupos con Wilcoxon e intergrupos con U de Mann–Whitney con paquete estadístico SPSS 20.0.
ResultadosSe analizó a 50 pacientes, del género masculino n=25 (50%), femenino n=25 (50%), edad mediana 12 años (rango 6–15), capacidad vesical con mejoría de 52.8% a 95.9% (p<0.001), contracciones no inhibidas 1.4 a 1.8 (p<0.001), intensidad de contracciones 47 a 8.5 (p<0.001), presión de llenado promedio prequirúrgico 40.8cm H2O y posquirúrgico 11.0cm H2O (p<0.001), promedio de presión de fuga 48.5 vs. 3.6cm H2O (p<0.001) y acomodación vesical 4.6 vs. 41.3cm H2O (p<0.001).
ConclusionesLa cistoplastia de aumento con colon sigmoides mejoró significativamente los parámetros urodinámicos, como capacidad vesical, acomodación vesical y presión de llenado en niños con vejiga neurogénica por mielomeningocele.
Detrusor hyperactivity or hyperactive bladder is a disorder characterised by involuntary contractions during the filling stage, which is associated with a wide variety of neurological conditions. The most common cause of neurogenic bladder in children is abnormal development of the spinal canal, associated with myelomeningocele in 90% of cases.1,2
These disorders have a high social and economic impact, and therefore different techniques have been developed to manage them, including: drug treatment, clean intermittent catheterisation and surgical management.3
The prevalence of myelomeningocele in Mexico is 1.2 per 1000 live newborns, with predominance in Caucasians and women 1.25:1, multiple complications at urological, intestinal, cardiac and orthopaedic levels are known.4
Urodynamics is a dynamic study of the transport, storing and evacuation of urine by the urinary tract, which comprises various tests that used individually or collectively can provide information on the functioning of the lower urinary tract; its components are: uroflow metre, cystomanometer, flow–pressure studies, electromyography, urethral profile, leak point pressure, videourodynamics and ambulatory urodynamics.5
In 2007, López Pereira et al.6 performed a study with 21 paediatric patients with neurogenic bladder with a poor response to clean intermittent catheterisation, who underwent bladder augmentation. Follow-up was 11 years and the subsequent urodynamic tests showed a significant improvement in bladder compliance, ureterohydronephrosis disappeared in all the patients, vesicoureteral reflux in 13 patients, and none of the patients presented new renal scars. At the end of the study renal function was normal in 20 of the patients.6
In 2009, Kajbafzadeh et al.7 performed a study to evaluate the efficacy of transcutaneous interferential electrostimulation, on emptying symptoms and in the urodynamics variables in children with mylomeningocele with neurogenic detrusor hyperactivity. Children aged from 3 to 16 resistant to conventional treatment with moderate to severe symptoms of incontinence and detrusor hyperactivity. The treatment group and the control group were randomised. A urodynamics study was performed before and after electrostimulation and the children were monitored over 6 months. The variables studied in the urodynamic tests were: average maximum detrusor pressure, maximum detrusor capacity, maximum bladder capacity, average detrusor compliance, residual urine and detrusor sphincter dyssynergia. This study demonstrated that therapy with electrostimulation is a minimally invasive technique, effective in terms of improved incontinence symptoms and in the parameters of the urodynamic tests in children with neurogenic detrusor hyperactivity caused by myelomeningocele.7
In 2010 Parshotam Kumar et al.8 performed an experimental bladder auto augmentation study on 18 lambs using the urinary bladder SURGISIS® and INTEGRA (collagen layer) in comparison with seromuscular enterocystoplasty. The auto augmentation was performed with the seromuscular layer of the small intestine, SURGISIS® or the collagen layer of INTEGRA®. Three months after the initial procedure, the lambs were reoperated, the elasticity was measured and the histological test performed. The post-operative period passed without incident in 17 lambs, as one of the enterocystoplasty group presented an intestinal obstruction; a statistically significant differences was observed in the elasticity in SURGISIS® and INTEGRA®. Bladder auto augmentation using the INTEGRA collagen layer showed better histological and functional results in comparison with SURGISIS® and seromuscular enterocystoplasty.8
The use of a segment of the digestive tract or a section of the ureter to enlarge or replace the bladder is an increasingly frequent procedure in paediatric urology; the sigmoid colon and the ascending caecum are the most-used segments due to their anatomical location, they are easy to mobilise and detubulate and there are few complications. Undertaking augmentations with sigmoid colon without mucosa, is an attempt to find a reservoir without intestinal mucus or the undesirable effects of gastrocystoplasty, such as: dysuria, haematuria and metabolic alkalosis. Furthermore, bladder augmentation before puberty preserves renal function and corrects bladder–ureteral reflux and ureterohydronephrosis in most patients, without reimplanting the ureters.6
The objective of the study was to describe the urodynamic changes after augmentation cystoplasty in paediatric carriers of myelomeningocele.
Materials and methodsTransversal, descriptive study; including patients from 1st January 2003 to 31 December 2013 in the Paediatric Urology Clinic of the Unidad Médica de Alta Especialidad, Hospital de Pediatría, Centro Médico Nacional de Occidente en Guadalajara, Mexico.
PatientsPaediatric patients aged from 8 to 16 with a diagnosis of neurogenic bladder due to myelomeningocele, who had undergone bladder augmentation with the sigmoid colon and with a urodynamic study before and after surgery. Patients with augmentation cystoplasty due to infection or trauma or with incomplete patient records were eliminated.
The databases of patients of the Paediatric Urology Clinic who met the inclusion criteria were reviewed. A review of the clinical records of the operated patients was undertaken. A data collection sheet was prepared, which included the 4 most common eurodynamic measurements: bladder capacity, uninhibited contractions, average filling pressure and leakage point. The information was gathered, the electronic base was emptied and the corresponding statistical analysis was made.
Description of technique‘Double calibre 7 or 9 French catheters were used for the urodynamic study. Eight channel Andromeda equipment was used for recording and the software used was Griffon Urodynamics V2.12. The study technique consisted of initial bladder emptying by catheterisation and cystometric study; the infusion speed was 20ml/min and bladder filling was stopped when the patient experienced discomfort when continuous losses of urine were produced or when the volume of perfused liquid exceeded the bladder's capacity which was estimated by the age of the patient. After each filling, the patient was asked to micturate even with Credé or Valsalva's manoeuvres, and the residue was measured.
Ethical aspectsThe guidelines as set out in the General Health Act on health research matters and the World Health Organisation's Helsinki Agreement on ethical principles for medical research in human beings were followed. The protocol was accepted by the local research and ethics committee with folio number R-2012-1302-30.
Statistical analysisNon-probabilistic sample of consecutive cases. Descriptive statistics were used with frequencies and percentages for the qualitative variables, medians and ranges; for quantitative variables. The Mann–Whitney U test was used for the inferential analysis to compare intergroup medians and the Wilcoxon test for intragroup medians. A p<0.05 was considered statistically significant. The statistical software package used was SPSS 20.0 for Windows.
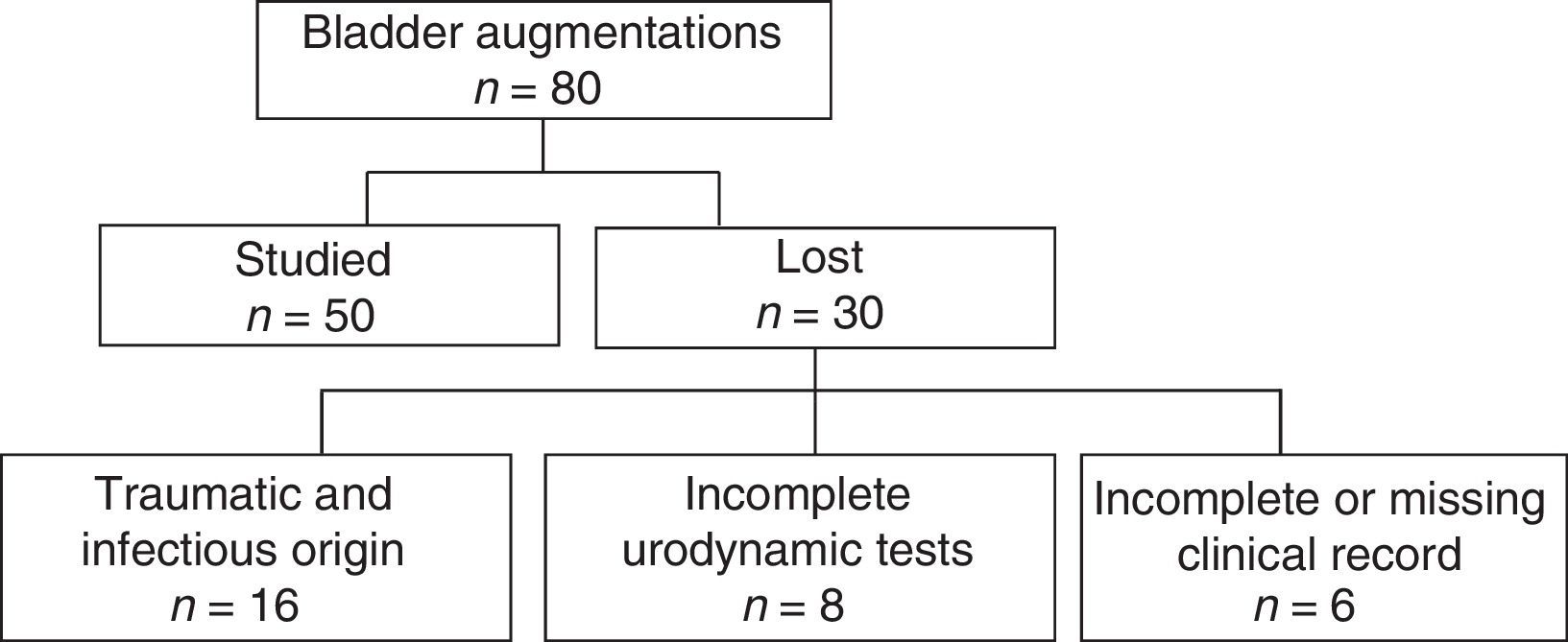
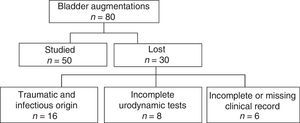
ResultsEighty bladder augmentations were carried out over the study period with sigmoid colon, due to myelomeningocele-associated neurogenic bladder in paediatric patients; of these, only 50 were studied who fulfilled the inclusion criteria. Fig. 1 shows the general study profile of the study and the reasons why the patients were excluded.
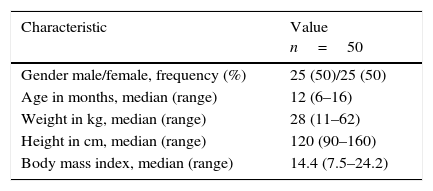
Table 1 shows the most important somatometric features which help us to describe the study population and we observe a symmetrical distribution in: gender, median of 12 years of age, weight of 28kg, height of 120cm and a body mass index of 14.4, with the respective ranges.
Clinical and sociodemographic characteristics of children after bladder augmentation with sigmoid colon for myelomeningocele-associated neurogenic bladder.
| Characteristic | Value n=50 |
|---|---|
| Gender male/female, frequency (%) | 25 (50)/25 (50) |
| Age in months, median (range) | 12 (6–16) |
| Weight in kg, median (range) | 28 (11–62) |
| Height in cm, median (range) | 120 (90–160) |
| Body mass index, median (range) | 14.4 (7.5–24.2) |
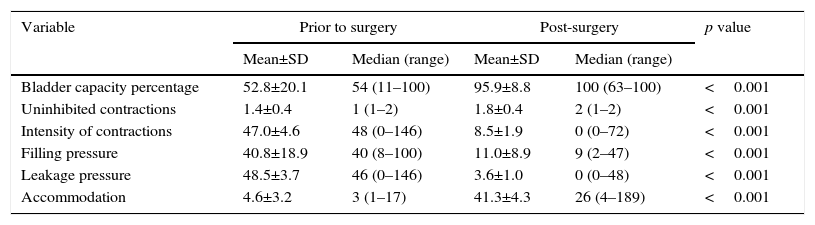
Table 2 presents the results of the urodynamic changes before and after bladder augmentation for neurogenic bladder. Important changes can be seen with a highly significant impact analysed before and after surgery, which were evaluated using Wilcoxon's test.
Description of urodynamic changes in paediatric patients with neurogenic bladder who have undergone bladder augmentation.
| Variable | Prior to surgery | Post-surgery | p value | ||
|---|---|---|---|---|---|
| Mean±SD | Median (range) | Mean±SD | Median (range) | ||
| Bladder capacity percentage | 52.8±20.1 | 54 (11–100) | 95.9±8.8 | 100 (63–100) | <0.001 |
| Uninhibited contractions | 1.4±0.4 | 1 (1–2) | 1.8±0.4 | 2 (1–2) | <0.001 |
| Intensity of contractions | 47.0±4.6 | 48 (0–146) | 8.5±1.9 | 0 (0–72) | <0.001 |
| Filling pressure | 40.8±18.9 | 40 (8–100) | 11.0±8.9 | 9 (2–47) | <0.001 |
| Leakage pressure | 48.5±3.7 | 46 (0–146) | 3.6±1.0 | 0 (0–48) | <0.001 |
| Accommodation | 4.6±3.2 | 3 (1–17) | 41.3±4.3 | 26 (4–189) | <0.001 |
Comparison of pre-and post-surgical medians using Wilcoxon's test.
SD: standard deviation.
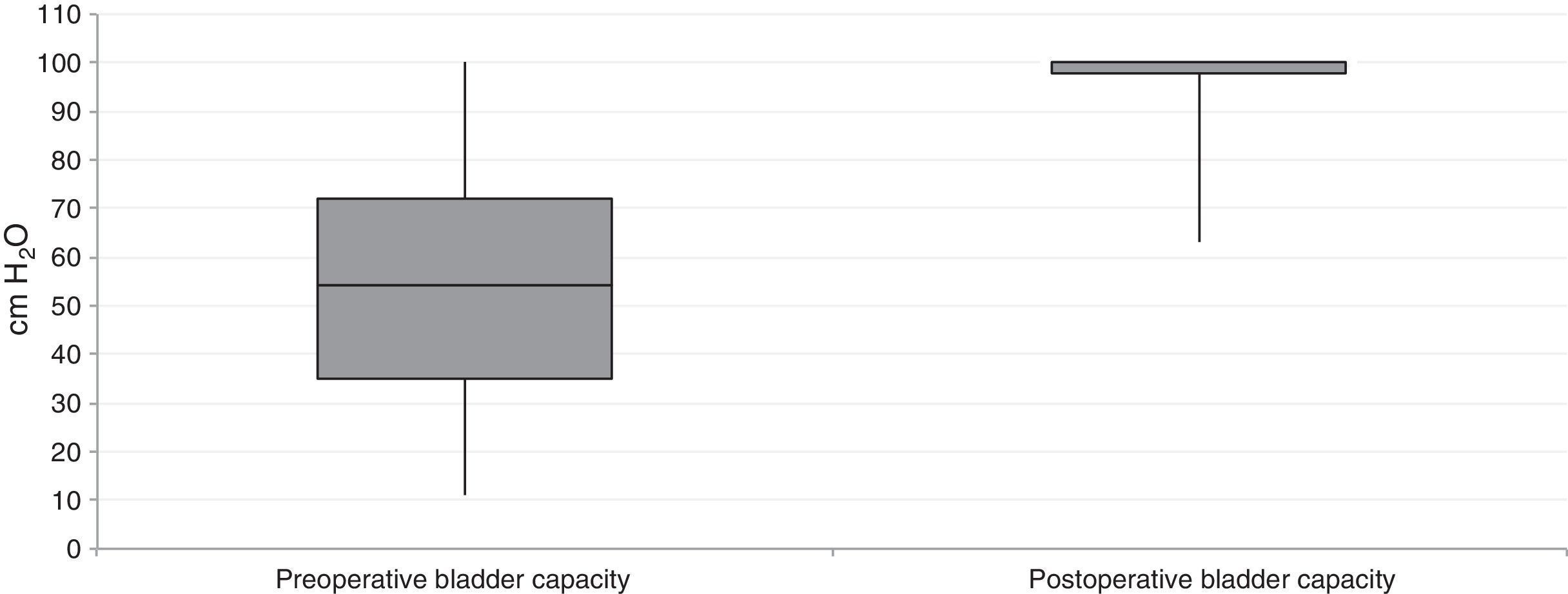
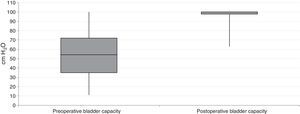
Fig. 2 shows the distribution of the values of bladder capacity before and after augmentation cystoplasty, we observe a considerable increase in the median with a small variability in the data in the post-operative period. The preoperative median of 54cm H2O increased to 100cm H2O after surgery.
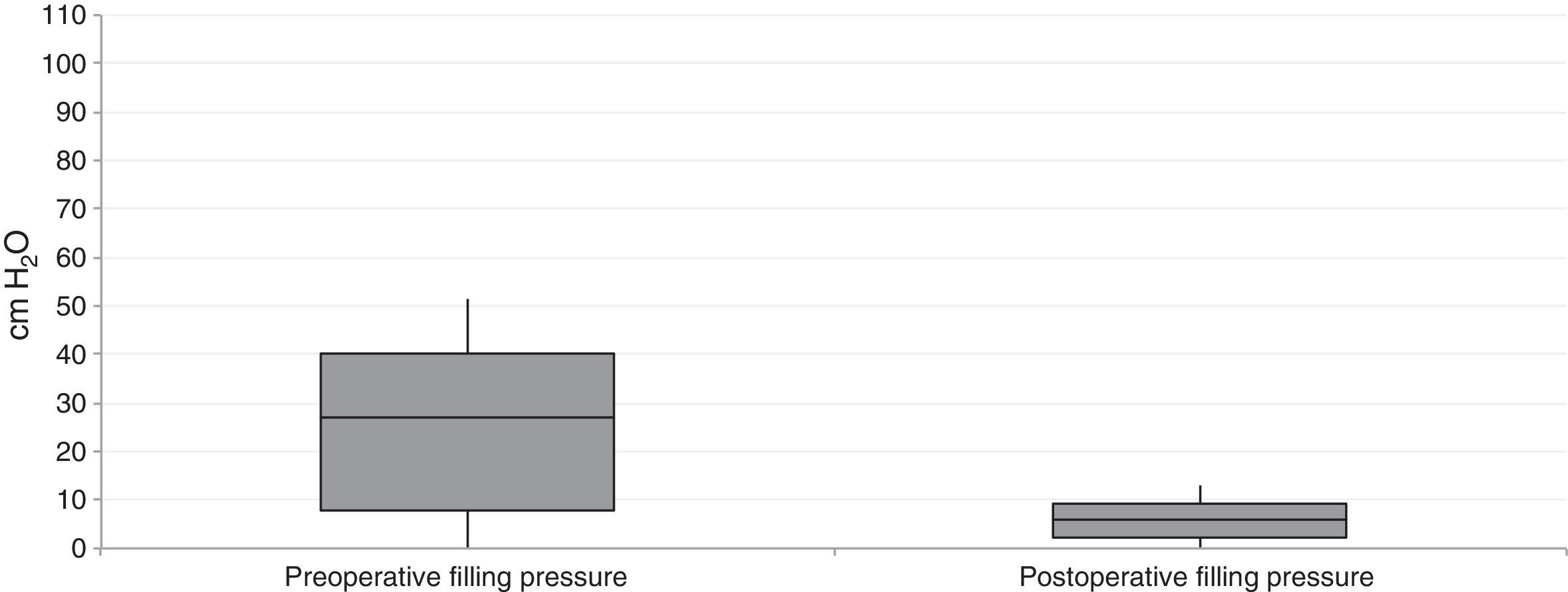
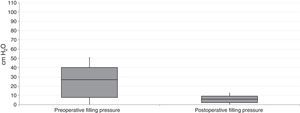
Fig. 3 shows the changes in filling pressure in the urodynamic test of the children who underwent augmentation cystoplasty for neurogenic bladder and we observed important changes with a median of 40cm H2O in the preoperative period, compared with 11cm H2O in the post-operative period, with the respective quartiles and minimum and maximum values in this series of patients.
DiscussionCystoplasty is a surgical procedure which is used to treat urological disorders in children. Its main objective is to reduce bladder pressure during filling and emptying of the bladder to prevent upper urinary tract damage and to reduce the risk of urinary tract infection and incontinence.9
Non-surgical treatment of neurogenic bladder with clean intermittent catheterisation, using pharmacological and antibiotic management, plays an important role in these patients. Failure of this treatment is the most common indication for performing a bladder augmentation for dysfunctional bladders.10
Bladder augmentation with gastro-intestinal tissue is the most frequent treatment for this disorder. The segment to be used is generally determined according to the preference and experience of the surgeon. Serious complications in patients with bladder augmentations performed using intestine, which include metabolic disturbances, which will depend on the segment of intestine used, the anatomical area, the time in contact with urine, kidney function and Ph and serum osmolarity disturbances. Hypokalaemia, hypomagnesaemia, hypocalcaemia and hyperammonaemia and raised urea and creatinine levels have also been reported. For these reasons, this procedure has very limited indications in patients with kidney failure.11
Median term an increase is presented of up to 30% in the incidence of bladder stones and stones of the upper urinary tract, these principally comprise phosphate, which indicates a major participation of bacteriuria and organisms that degrade urea as conditioning factors for this change. Excess mucous is also produced which impedes the management of catheters in the post-operative period and implies a major risk of urinary fistulae.
An increase in the incidence of malignant diseases has also been published in recent years, due to internal and external carcinogenic factors, which might cause changes in DNA structure. The incidence of cancer, principally adenocarcinoma occurs in the anastomosis site at 5% and 13%, at least 10 years after surgery. Patients with a history of bladder extrophy and bladder augmentation have a greater risk of presenting this malignant disease in their forties.12
After bladder augmentation patients often require clean intermittent catheterisation, because cases of spontaneous perforation have been reported which require emergency surgery. In addition, other complications present which are inherent to the use of intestine, such as intestinal obstructions, enteric fistulae, intoxication due to the reabsorption of drugs, malabsorption syndrome, changes in glucose metabolism, delayed development and bone disease. A great many materials have been investigated in an attempt to reduce complications, but to-date with poor results.13
Since the first report on the use of ureteral segments for bladder augmentation with tortuous and redundant refluxing megaureters, non-functioning kidney, these have had good results. Ureteral tissue is an autogenous material, with elastic muscular tissue and transitional cell epithelium.
All of our patients had myelomeningocele-associated neurogenic bladders and the intestinal segment used was the sigmoid colon, which is still the most frequently used world-wide according to the literature.14 It is metabolically less active in the absorption of urine solutes, although it presents greater peristalsis. Due to its surface area, it is excellent in providing adequate augmentation of bladder capacity.
Almodhen et al.15 in a longitudinal in 2007, followed up children with myelomenignocele treated conservatively by performing a urodynamic study and radiography every 6 months and they demonstrated significant changes in the upper urinary tract, and urodynamic changes. The changes observed in their study are similar to those we demonstrate in this series. Therefore we consider that augmentation cystoplasty with the sigmoid colon is a useful technique in the management of paediatric patients with myelomeningocele-associate neurogenic bladder.15
ConclusionsAugmentation cystoplasty with the sigmoid colon significantly improved the urodynamic parameters, such as bladder capacity and filling pressure, in children with myelomeningocele-associated neurogenic bladder.
Conflict of interestsThe authors have no conflict of interests to declare.
We thank the Paediatric Surgery Department and particularly the Paediatric Urodynamics Clinic for providing the facilities to prepare and publish this research study.
Please cite this article as: Zaragoza-Torres RI, Galarza-Flores ME, Gómez-Castellanos JC, Barrera-de León JC. Cambios urodinámicos posteriores a cirugía de ampliación vesical por vejiga neurogénica en pacientes pediátricos con mielomeningocele. Cir Cir. 2016;84:113–118.