Arteriovenous fistulas secondary to gunshot wounds have been increasing due to military activities, with endovascular treatment showing better results in haemodynamically stable patients.
Clinical caseA 16 year-old male with diagnosis of femoral arteriovenous fistula in the left lower extremity was admitted to general surgery for endovascular management. A procedure with stent was performed without complications, and is currently on anticoagulant and antiplatelet treatment.
ConclusionArteriovenous fistulas under the inguinal region can be safely treated with endovascular treatment (embolisation or stent) on stable patients. The objective of this therapy is to close the defect between artery and vein. This is the case of a patient with great results due to endovascular treatment, decreasing complications of the surgical treatment.
Las fístulas arteriovenosas secundarias a arma de fuego han ido en incremento debido a las cuestiones bélicas, mostrando un beneficio en el manejo endovascular para pacientes hemodinámicamente estables.
Caso clínicoSe presenta el caso de un paciente masculino 16años de edad con diagnóstico de fístula arteriovenosa femoral en miembro pélvico izquierdo, que ingresó al Servicio de Cirugía para manejo endovascular. Se realizó procedimiento con stent sin complicaciones, egresando del servicio sin complicaciones. Actualmente en tratamiento anticoagulante y antiagregante.
ConclusiónLas fístulas arteriovenosas por debajo de la región inguinal pueden ser tratadas de manera segura con terapia endovascular (mediante stents o embolización) en pacientes hemodinámicamente estables. El objetivo del tratamiento es cerrar el defecto entre la arteria y la vena, obliterando el flujo que la nutre. Este fue el caso de este paciente, con buenos resultados tras la terapia endovascular, con lo que disminuyeron las complicaciones del tratamiento quirúrgico.
Fistulas are, by definition, communication between the arterial and venous tree, circumventing capillary flow. They are divided into 2 main areas: congenital and traumatic. The latter are sub classified into iatrogenic and accidental. Iatrogenic fistulas are caused by invasive procedures, such as the insertion of catheters, surgical events, and biopsies. Accidental fistulas are produced by penetrating wounds (stab wounds, object fragmentation and gunshot wounds).1,2
The main arteriovenous fistulas secondary to gunshot wounds are, in order of frequency located in: 22% superficial femoral artery; 16% popliteal artery; 1% posterior tibial artery; 8% brachial artery; 43% head and chest and 11% other locations. They are more frequently found in males (3.1:1).3
There are 6 types of arteriovenous fistulas: (1) simple communication between artery and vein; (2) interposition of aneurysmal sac between artery and vein; (3) arteriovenous communication in addition to arterial aneurysm; (4) presence of arterial aneurysm and aneurysmal sac in communication with the fistula; (5) aneurysmal sac which may be above or below the fistula and (6) fistula inside the aneurysmal sac.4,5
The aim of this paper is to present the case of a patient with a type 2 arteriovenous fistula, with endovascular management.
Clinical caseA 16 year old male patient, with no relevant medical history, presented at the emergency department after receiving a gunshot wound in the left thigh, and with unstated blood loss. On examination the patient was found to have no neurological damage, lung fields had not been compromised, heart sounds were of good intensity and frequent, abdomen was not affected. The left thigh had a gunshot opening wound in the side of the thigh, 1cm in diameter in the distal third of the thigh, with a wound exit opening 1cm in diameter in the distal third medial region of the thigh. There was oedema of the limb; posterior popliteal, pedis and tibial pulse rates of good intensity; capillary refill time of 4s; muscular strength of 4/5, with slight pain on movement. The patient denied any paresthesia and there were no signs of change in contralateral limb. Vital signs: breathing rate: 18min−1, heartbeat: 88min−1, blood pressure: 110–60mmHg.
Resuscitation was performed with crystalloid solutions, and good haemodynamic parameters were obtained.
Laboratory study results were as follows: leukocytes 14mil/mm3, haemoglobin 14.3g/dl, platelets 310,000mm3, glucose 157mg/dl, creatinine 1.4mg/dl, sodium 140mEquiv., potassium 3.5mEquiv. Anterior–posterior and lateral x-ray of the thigh showed no bone lesion. An arterial Doppler ultrasound (USG) showed major oedema of tissues, with correct flow in the external iliac artery, superficial femoral artery, deep femoral artery, popliteal artery, posterior and anterior tibial arteries, with no sign of lesion. A venous Doppler ultrasound showed the external iliac vein, common femoral vein, superficial femoral, deep femoral, popliteal, posterior and anterior tibial veins with good blood vessel diameter and no presences of blood clots or lesions.
The patient was administered treatment with antibiotics, antithrombotic therapy and monitoring of the limb. Forty eight hours later the affected limb presented with paresthesia, pain, weakness on raising the lower limb and when walking. There was also an increase in volume in the distal third of the left thigh. On examination the following were observed: equimosis; delayed capillary refill; femoral, popliteal, posterior tibial and pedis pulses all with good intensity; trill (vibration) during palpation and heart murmur on auscultation.
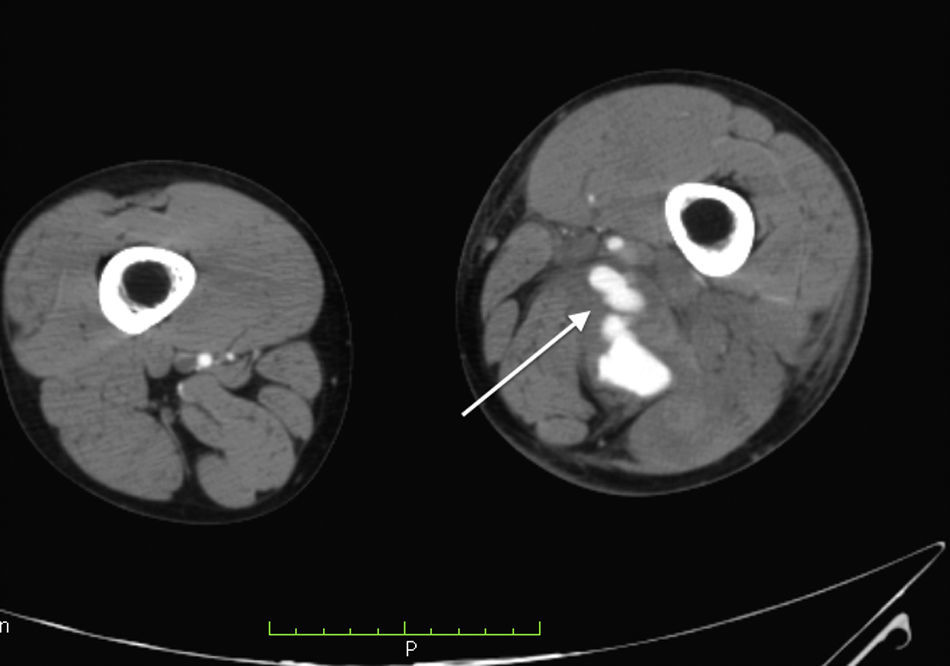
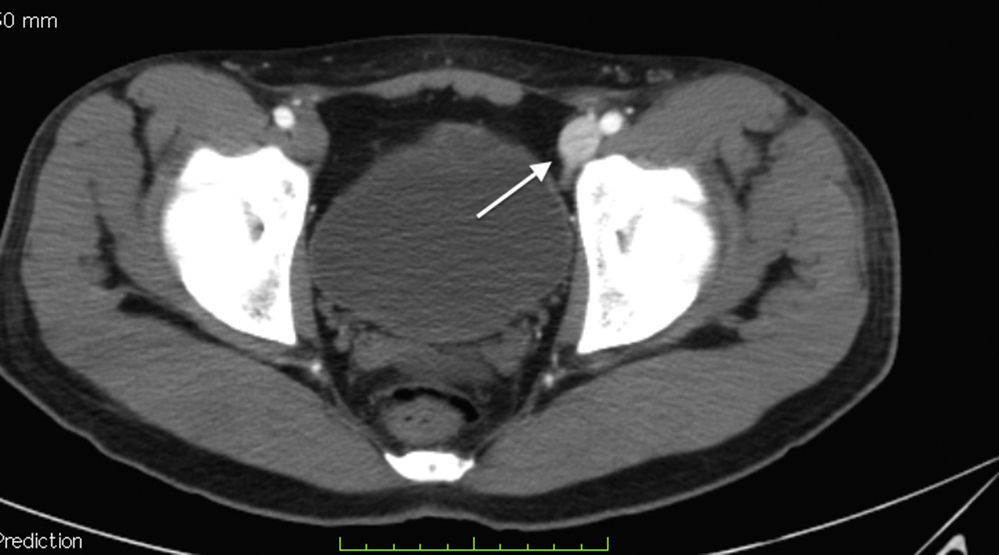
Laboratory control tests were performed and due to a drop in haemoglobin to 8.7g/dl, the patient was given a unit of packed red blood cells. The other tests were unremarkable. Angiotomography was performed and a post-traumatic arteriovenous fistula with aneurismal sac interposition was observed (classified as stage 2) (Figs. 1–3).
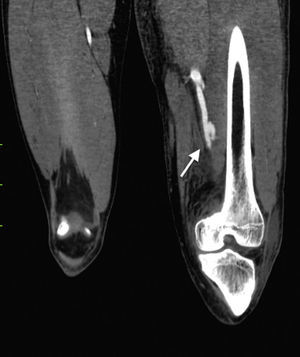
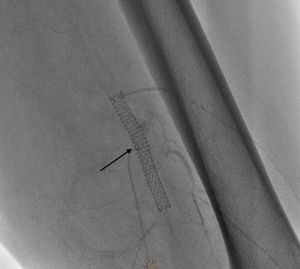
In view of the above, the patient was referred for a periphery interventionist procedure percutaneously. Approach was contralateral and the right femoral artery was accessed using a modified Seldinger technique. A 7Fr Epsylar introducer 45cm sheath was inserted, passing to the left iliac artery using fluroroscopy. The angiography revealed: (1) external and internal common left iliac artery with no angiographic lesions; (2) common femoral artery and deep left femoral artery with no angiographic lesions; (3) arteriovenous fistula in the distal segment of the left superficial femoral artery before the beginning of the popliteal artery, with 4cm×3cm pseudoaneurysm imaging, leading to minor compromise of distal circulation (Fig. 4).
Surgical intervention commenced with an 0.035cm×260cm hydrophilic filament guide, positioned at the level of the fistula and covering the mouth of the pseudoaneurysm with a 6mm×57mm Be Graft BENTLEY INNOMED stent which was released at nominal pressure and expanded up to 13 atmospheres (6.6mm in diameter), closing the fistula and the pseudoaneurysm completely, with no leakage of contrast. Anticoagulant and antiplatelet drugs were administered (Figs. 5 and 6).
Clinical improvement of the limb occurred three days after treatment with a reduction in oedema, and correct pulses. The patient was discharged from hospital, having improved after a 7 day regimen of antibiotics. Passive mobilisation of the limb was recommended, as was support for walking and physiotherapy. At the medical review one month later the limb was observed to be oedema-free, skin colour was good, muscular strength was good, 5/5, capillary refill was at 3s, pulses were of good intensity and frequency throughout the body. The patient continued treatment with anticoagulants (coumarins) and antiplatelet drugs (aspirin and clopidogrel).
DiscussionVascular lesions associated with automobile accidents and complex surgical procedures have increased compared with the previous century, as have those resulting from military activities. Advances in both diagnosis and treatment have been made, with better survival and limb preservation as a result.5
Arteriovenous fistulas must always be treated as vascular lesions since they may go unnoticed and clinical signs will depend on the blood flow of the arteriovenous fistulas. High-flow arteriovenous fistulas are characterised by heart failure and venous hypertension conditions with their concomitant skin changes. Medium-flow arteriovenous fistulas are characterised by dilatation of the areas next to the artery produced by endothelium shearing which leads to a mass that may develop a compartment syndrome. Low-flow arteriovenous fistulas are generally asymptomatic, and do not lead to haemodynamic changes.6,7
The clinical signs which are highly suggestive of lesion are: trill (vibration) and heart murmur on auscultation. Those suggestive of arterial failure are: claudication, hypothermia and delayed capillary refill.
In those cases where both an arteriovenous fistula and a pseudoaneurysm are present, treatment should be administered immediately on detection, since complications such as rupture, thrombosis and embolisms may present which compromise distal to the limb.8
Diagnosis may be made using non invasive methods, the Doppler ultrasound (USG) being the first choice option due to the fact that blood flow may be assessed and the location of the fistula. As a result, the possible risks from invasive methods are lowered.9,10
Selective angiography plays a major role in assessing the site of vascular compromise, providing better data than the conventional ultrasound with regards to location, type of fistula, affected blood vessels and perivascular complications. This type of test is reserved for haemodynamically stable patients, and mortality has been estimated at 0.025%.11–14
Management of these lesions has evolved from an open surgical approach with ligation of the affected vessel and vascular reconstruction to a closed surgical approach with endovascular therapy. The indications for an open surgical approach are: haemodynamically unstable patients, lesions which compromise a patient's life; high risk of infection due to time in surgery, the lack of a team specialised in endovascular management and damage to neighbouring tissues (muscles and nerves). Endovascular therapy is the gold standard for haemodynamically stable patients. The advantages are: reduction in pain; faster recovery; the use of a remote access site from the lesion location and a lower risk of infection.15–18
Surgical treatment consists of resection of the pseudoaneurysm and primary closure when possible; Should a major defect be found, blood vessel resection must be performed with the inclusion of the pseudoaneurysm and anastomosis performed, be this primary or with the use of an inverted saphenous vein graft.19–21
The goal of arteriovenous fistula treatment is to eliminate the flow which maintains the fistula, converting it into laminar flow. The aim of endovascular treatment is to protect the main artery and vein, closing both the fistula and the pseudoaneurysm. Greater success has been observed with the use of stents or grafts.
The group of stents includes those which are covered (PTFE, dacron, polyurethane) and those which are not (self-expandable or balloon-expandable). The covered stents have been mentioned in this article due to their great use in arteriovenous fistulas and pseudoaneurysms, with no blood passing through the mesh. In people of advanced age the use of stents with peripheral arterial occlusive disease may lead to thrombosis and stenosis. It is known that thrombosis is the body's response to a foreign body located in the blood vessel. Treatment with anticoagulants and antiplatelet drugs reduces the incidence of thrombosis by at least 2%, and it is therefore important to always assess the patient's age and personal habits prior to treatment.21
ConclusionArteriovenous fistulas under the inguinal region may be safely treated with endovascular therapy using stents or embolisation and this is the gold standard for haemodynamically stable patients, offering a better outcome than that offered by open surgery. The main treatment goal for an arteriorvenous fistula is closure of the defect between artery and vein. Failure in complete closure may lead to high recurrence with total change in the blood vessel architecture, and this would require a more complex management and would also involve high morbidity for both the irrigated area and for the patient.
Endovascular treatment for post traumatic fistulas in the lower pelvis is a good alternative in haemodynamically stable patients.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank the Imaging Department, and in particular Dr. García Santillán, for his interpretation of the tomography images, and also the Haemodynamic Department in the Centro Médico Licenciado Adolfo López Mateos, Toluca, State of Mexico.
Please cite this article as: Rogel-Rodríguez JF, Zaragoza-Salas T, Díaz-Castillo L, Noriega-Salas L, Rogel-Rodríguez J, Rodríguez-Martínez JC. Fístula arteriovenosa femoral postraumática, tratamiento endovascular. Cir Cir. 2017;85:158–163.