Eccrine porocarcinoma, first described in 1963, is a rare malignant lesion arising from the eccrine sweat glands. It is usually a primary tumour, or even more common, a malignant degeneration of an eccrine poroma. It usually affects older persons and is located most commonly on the lower extremities. About 20% of eccrine porocarcinoma will recur after treatment. The treatment is wide local excision of the primary lesion. This uncommon skin tumour has a locally aggressive behaviour and a high recurrence rate.
Clinical caseAn 82 year-old man presenting with multiple recurrent eccrine porocarcinoma with inguinal metastasis. The treatment was a radical excision and inguinal lymphadenectomy. There were no postoperative complications, but there was local recurrence after six months.
ConclusionEarly diagnosis and wide excision is the best way to achieve a good prognosis, due to the aggressiveness of this tumour.
Descrito por primera vez en 1963, el porocarcinoma ecrino es un raro tumour maligno que se desarrolla de las glándulas ecrinas, presentándose como tumour primario, o más frecuentemente mediante transformación maligna de un poroma ecrino. Afecta a pacientes de edad avanzada y la localización más frecuente es en extremidades inferiores. Se observa una recurrencia local del 20% después del tratamiento. La escisión quirúrgica es el tratamiento de elección. Esta infrecuente neoplasia cutánea tiene un comportamiento localmente agresivo y un alto índice de recidiva.
Caso clínicoPresentamos el caso de un varón de 82 años con porocarcinoma ecrino multi-recidivado y metástasis ganglionar, tratado con extirpación amplia y linfadenectomía inguinal. Buena evolución postoperatoria. Múltiples recidivas locales a los 6 meses.
ConclusiónDebido a su carácter potencialmente agresivo, el diagnóstico precoz y su rápido tratamiento quirúrgico es la forma adecuada de conseguir un pronóstico favorable frente a este tipo de tumor.
According to Marone et al.,1 eccrine porocarcinoma was described in 1963 by Pinkus and Mehregan as epidermotropic eccrine carcinoma. It is a rare type of skin cancer (0.005–0.01% of all skin tumours), which arises from the sweat glands. It can be a primary or a transformation of an eccrine poroma. It has the same incidence in both genders, and principally affects people of advanced age. Fewer than 300 cases have been reported in worldwide medical literature,1,2 and its incidence in Europe is rare. Twenty percent of these tumours recur, 10% metastasise to solid organs, and 20% metastasise to regional lymph nodes, with a mortality of almost 70% in the latter. It is difficult to establish an accurate prognosis as there is little follow-up of the cases described because the tumour is so rare.
Clinically it manifests as a solitary lesion, which can be ulcerated nodule in type, or a papule or verrucous lesion. Differential diagnosis can be made with basal cell carcinoma, epidermoid carcinoma, seborrheic keratosis, etc.
The most common location is on the lower limbs, head and neck, and it is less frequent on the trunk, vulva, chest, nail bed, and upper limbs.
Histological diagnostic criteria for eccrine porocarcinoma are an accumulation of atypical cells, some with tubular structures, which emigrate from the epidermis, and are glycogen rich and PAS positive.
The treatment for this type of tumour is by broad surgical excision, Mohs surgery or radiotherapy. Mohs surgery is a surgical technique which enables the removal in layers of selected skin tumours and achieves the highest cure rates. Likewise it enables maximum saving of healthy tissue. All of this is possible through microscopic supervision, which enables 100% analysis of the tumour edges of each of the layers, and thus guide the surgeon through the successive lines of tumour until it is completely removed.
Surgical treatment is curative in 80% of cases. The role of prophylactic radical lymphadenectomy is debatable.3
Clinical caseAn 82-year old male patient with a personal history of arterial hypertension, diabetes mellitus and benign prostatic hypertrophy. The patient began with a papulous lesion 4 years previously, which was circular, 1cm in diameter, in the area of the right hip, which was removed with an anatamopathological diagnosis of porocarcinoma, for which he received radiotherapy. He was referred to the plastic surgery unit with local recurrence in the form a of a 1cm papule next to the scar, which was surrounded by an area of major radio dermatitis of 8cm×5cm. The patient underwent computed tomography on which right inguinal adenopathies were identified radiologically suspicious of metastasis. A fine-needle aspiration was undertaken (FNA) of these adenopathies which were palpable on physical examination, and were reported as positive malignancies; the remainder of the extension study reported no evidence of distant metastasis.
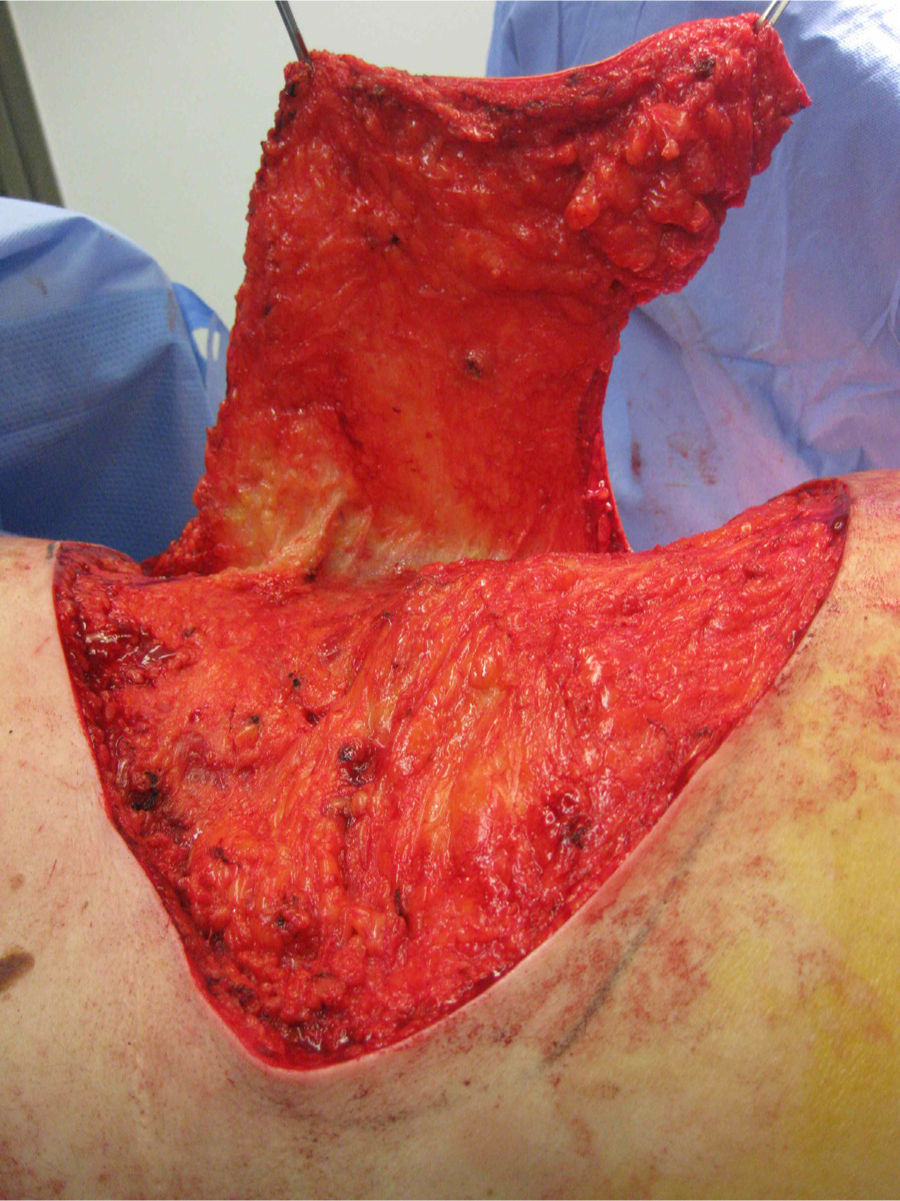
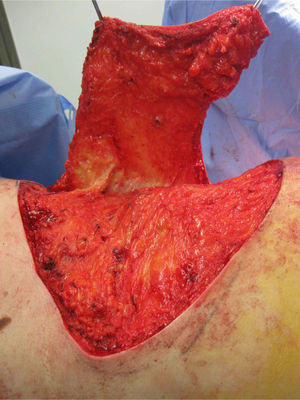
The patient was operated under general anaesthesia, and an en bloc excision of the area of radio dermatitis was performed including recurrence with more than a 2cm margin of healthy tissue (Fig. 1); cover was made using a large rotation flap of the right flank with medial base (Fig. 2); and right inguinal lymphadenectomy (Fig. 3). The anatomopathological report was compatible with recurrence of porocarcinoma, radiodermal changes and broad surgical margins; porocarcinoma metastasis in 2 of the isolated lymph nodes.
There were no incidents in the post-operative period (Fig. 4). Oncology took over follow-up and evaluation of the patient, they did not administer adjuvant treatment, because no signs suggestive of recurrence were seen on control computed tomography.
Six months after surgery the patient presented with skin lesions again in the form of papules on the periphery of the flap suggestive of porocarcinoma, which were removed under local anaesthetic, and the suspected diagnosis was confirmed. Further lesions appeared subsequently which were compatible again with local recurrence which extended towards the abdomen and were treated (in the outpatient department) by excision under local anaesthetic (Fig. 5).
Three years after the last surgery, the patient continues to have good quality of life, because he has been provided multidisciplinary care, due to his age and the high recurrence rate in a patient of 83, for whom it has been demonstrated that there is no effective systemic treatment. It was decided, therefore, that minor surgery (as an outpatient) for the excision of recurring lesions was the best course of action.
At present, 3 years after surgery, the patient continues to have a good quality of life, and recurrences are being treated in the outpatient department.
DiscussionEccine porocarcinoma is a rare skin neoplasm, which derives from the eccrine sweat glands. This tumour can appear de novo or as a progression from a benign poroma, it is very slow growing at onset but after it becomes malignant it behaves aggressively and grows rapidly. It is frequently located on the head and limbs of patients of advanced age (average age 68). Clinically it presents as a nodule, erosive plaque or papule which tends to ulcerate, and can be easily confused with pyogenic granuloma, basal cell carcinoma or amelanotic melanoma.4
From a histopathological perspective5,6 it originates from the intraepidermal portion of the eccrine glands and can be limited to the epidermis or extend to the dermis. The intraepidermal form grows horizontally, and produces pagetoid infiltration in the epidermis: the dermal form shows nodular aggregates with no connection to the epidermis.
Different therapeutic modalities have been applied with eccrine porocarcinoma.7,8 Broad excision is curative in 80% of cases, Mohs surgery is useful and 2–4 years of post-operative follow-up without recurrence have been seen. Chemotherapy is reserved for the treatment of metastatic eccrine porocarcinoma, there are no standard protocols, and varying grades of response. Radiation is of little benefit, and is left for palliative care as response is partial. The role of sentinel node biopsy is unknown, and prophylactic lymphadenectomy is controversial. The high recurrence rate of the case presented should be taken into account; even with broad margins of healthy tissue there was recurrence on several occasions.
ConclusionsEccrine porocarcinoma, although rare is potentially aggressive with a high recurrence rate and distant metastasis. When malignant there can be a delayed diagnosis as it can be confused with a benign lesion. Treatment consists of surgery with broad margins and thorough follow-up to detect possible recurrence. We consider that early diagnosis by a specialist and rapid surgical treatment is the most appropriate way of achieving a benign prognosis for this aggressive tumour.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Acosta-Arencibia A, Abrante-Expósito B, Ramos-Gordillo M. Porocarcinoma ecrino multirrecidivante con metástasis inguinal. Caso clínico. Cir Cir. 2016;84:73–76.