The bilateral brachial plexus block is considered a contraindication, due to the possible development of complications, such as toxicity from local anaesthetics or bilateral diaphragmatic paralysis. However, with the real time visualisation provided by the ultrasound scan, these complications have decreased and it is a safer procedure.
Clinical casesFour cases are presented where the bilateral block was performed using guided ultrasound, as the patients were unable to receive general anaesthesia due to a history of adverse effects or the use of opioids in the post-operative or by the prediction of a difficult airway associated with obesity. A systematic review of the literature from January 1993 to June 2013, was also performed by using a search in the MEDLINE, EMBASE, ARTEMISA, LILACS, Google data bases, in Spanish and English language with the following words: bilateral brachial plexus block, bilateral interscalene block, bilateral infraclavicular block, bilateral supraclavicular block, bilateral lateral supraclavicular block, bilateral axillary block, ultrasound-guided bilateral brachial plexus block.
ConclusionBased on the evidence found, ultrasound-guided bilateral brachial plexus block in selected patients and expert hands, is no longer a contraindication.
El bloqueo de plexo braquial bilateral se ha considerado una contraindicación debido al posible desarrollo de complicaciones, como toxicidad por anestésicos locales o paresia diafragmática bilateral; pero con la visualización en tiempo real que proporciona la ecografía, estas se reducen, lo que nos proporciona un procedimiento más seguro.
Casos clínicosPresentamos 4 casos en los que se realizó el bloqueo bilateral guiado por ecografía debido a la negativa de los pacientes a la administración de anestesia general, por antecedente de efectos adversos con su utilización o con los opioides en el postoperatorio, o bien por predicción de una vía aérea difícil asociada a obesidad. También exponemos una revisión sistemática de la literatura de enero de 1993 a junio de 2013, en las bases de datos MEDLINE, EMBASE, ARTEMISA, LILACS y Google, en idioma español e inglés con las siguientes palabras: bilateral brachial plexus block, bilateral interscalene block, bilateral infraclavicular block, bilateral supraclavicular block, bilateral lateral supraclavicular block, bilateral axillary block, ultrasound guided bilateral brachial plexus block.
ConclusiónCon base en la evidencia encontrada, el bloqueo del plexo braquial bilateral guiado por ecografía en pacientes seleccionados y con personal entrenado deja de ser una contraindicación.
Historically, the brachial plexus block in its bilateral application is contraindicated mainly in its supraclavicular and interscalene approach,1,2 since the diffusion of local anaesthetic may block the phrenic nerve, causing diaphragm paresis with changes to the breathing mechanics, which bilaterally may cause respiratory failure.3 This was prompted by the plexus location techniques, since blind methods such as paraesthesia or neurostimulation were used, requiring large volumes of local anaesthetic to result in a successful block.4,5 But with the advent of ultrasound as a guide to conduct these procedures, it is possible to perform them safely, since the technique offers the following advantages: it allows location of the brachial plexus; usually the phrenic nerve may be observed,6 even in the presence of anatomical variations7,8 which negatively affect the patient's breathing mechanics; and it is also possible to directly visualise adjacent structures, particularly muscles, arteries and veins, thereby avoiding accidental injections, using a lower amount of anaesthetics, controlling diffusion to immediate areas, avoiding diffusion to structures that do not require blocking, and it is all conducted in real time.1–3 Thus, the purpose of the case study was to show that with an ultrasound-guided bilateral brachial plexus block the phrenic nerve is not blocked and, therefore, the patient's ventilation is not affected. In addition, we conducted a systematic review of the procedure to support the suggested recommendations.
Clinical casesAll patients were asked for a written informed consent, wherein the nature of the procedure was explained as well as the potential complications, which they accepted. The procedures were conducted by anaesthetists with experience equal to or greater than 5 years conducting this type of procedure. Transoperative analgesia was adequate in all cases. The CO2 curve, respiratory rate, and oxygen saturation were not modified during the entire surgery; also, there was neither dyspnoea nor any evidence of respiratory failure during the transanaesthetic or the mediate postoperative periods.
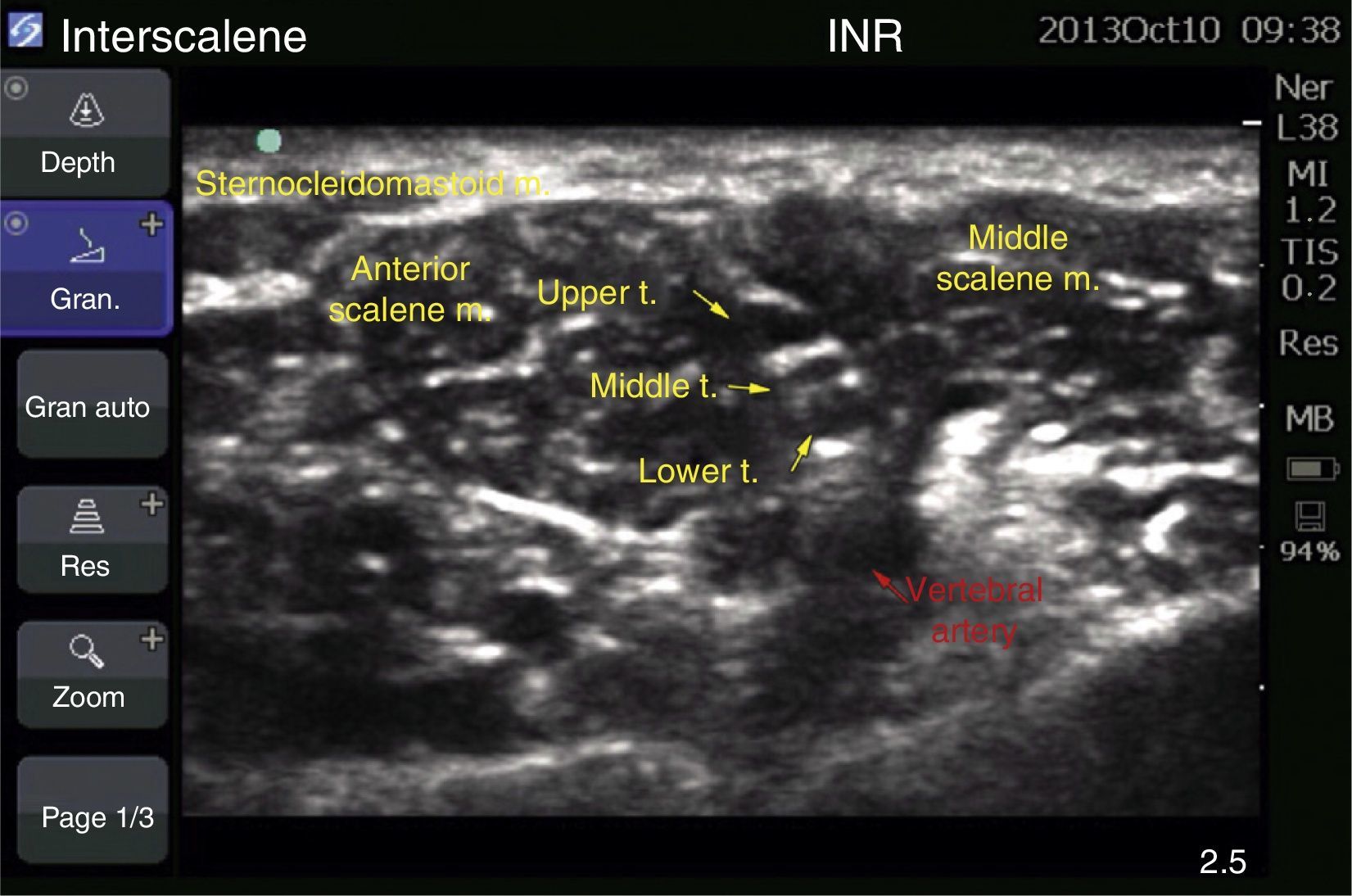
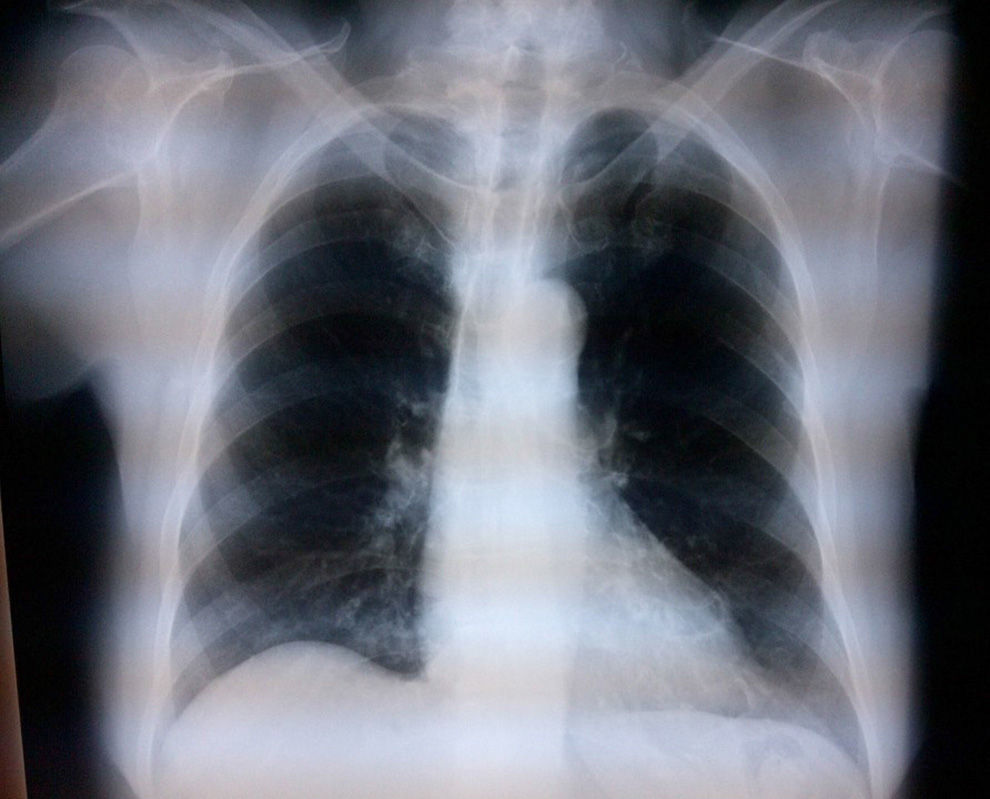
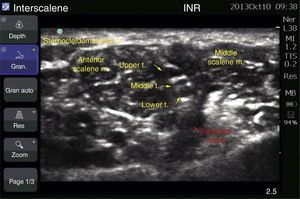
Case 1: bilateral interscalene blockFemale patient of 70 years, ASA II, with a diagnosis of subacromial impingement, scheduled for bilateral shoulder arthroscopy (biceps tenotomy, subacromial decompression, acromioplasty, and distal end resection of bilateral clavicle), history of systemic hypertension, who did not accept general anaesthetics, therefore local anaesthetics were chosen. The block was conducted with an ultrasound (MicroMaxx Ultrasound System, SonoSite Inc., United States) and a linear transducer of 13-6MHz (HFL38, SonoSite Inc., United States) jointly with neurostimulation (B Braun Melsungen AG, Stimuplex Dig RC, Germany). The procedure was conducted first on the left side. The transducer was placed for a cross-section approach, and the procedure was conducted on the long axis with an insulated needle of 50mm (B Braun Melsungen AG, Stimuplex A50, Germany); neurostimulation started once the nerve trunks were visualised and the needle tip was perineural, resulting in a muscular response, the contraction of the deltoid muscle, with a current intensity of 0.35mA in grade II; the procedure was the same for both blocks. An adequate circumferential diffusion was visualised, with root displacement (Fig. 1). The local anaesthetic used was ropivacaine 7.5% with 15cm3 for each side; a total dose of 225mg was used (equivalent to 3mg/kg). Dexmedetomidine at 1mcg/kg/h was used for sedation. The surgical position used was “beach chair”. A chest X-ray was taken upon completion to assess the hemidiaphragms, which were not compromised (Fig. 2).
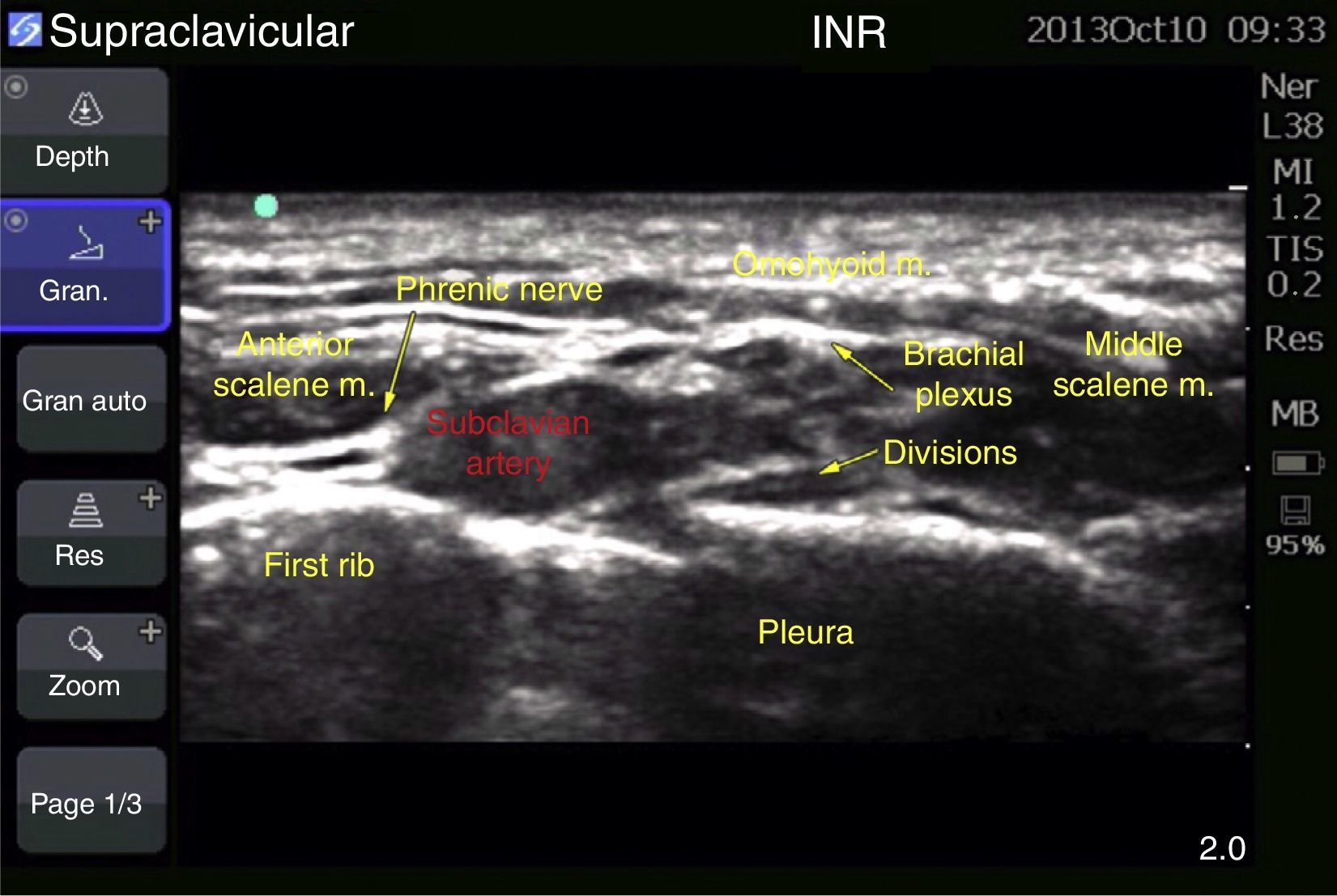
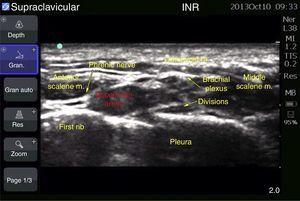
Case 2: bilateral supraclavicular blockFemale patient of 53 years, ASA III, with a diagnosis of bilateral radius fracture, scheduled for osteosynthesis of distal radius. History of obesity (BMI 42.96), hypertension, diabetes mellitus type 2 and sleep obstructive apnoea. Regional anaesthetics were chosen due to her co-morbidities. The block was guided with ultrasound (MicroMaxx Ultrasound System, SonoSite Inc., United States) and a linear transducer of 13-6MHz (HFL38, SonoSite Inc., United States). The left block was conducted first, the transducer being placed in the supraclavicular cavity, parallel to the clavicle, with the edge touching the internal face of the clavicle and angled towards the chest; it was conducted on the long axis with an insulated needle of 100mm (B Braun Melsungen AG, Stimuplex A100, Germany); once the subclavian artery was visualised (a round, pulsating, hypoechoic image), as well as the first rib (hyperechoic), the brachial plexus was identified, which appeared with 4–6 round, hypoechoic structures inside, with hyperechoic edge, grouped in the appearance of a “bundle of grapes”; the needle was placed along the angle formed by the carotid artery and the first rib, ropivacaine 0.75% and lidocaine 2% plain were administered, with a total dose of 180 and 300mg (equivalent to 3 and 5mg/kg of ideal weight, respectively, for a volume of 20ml on each side) (Fig. 3).
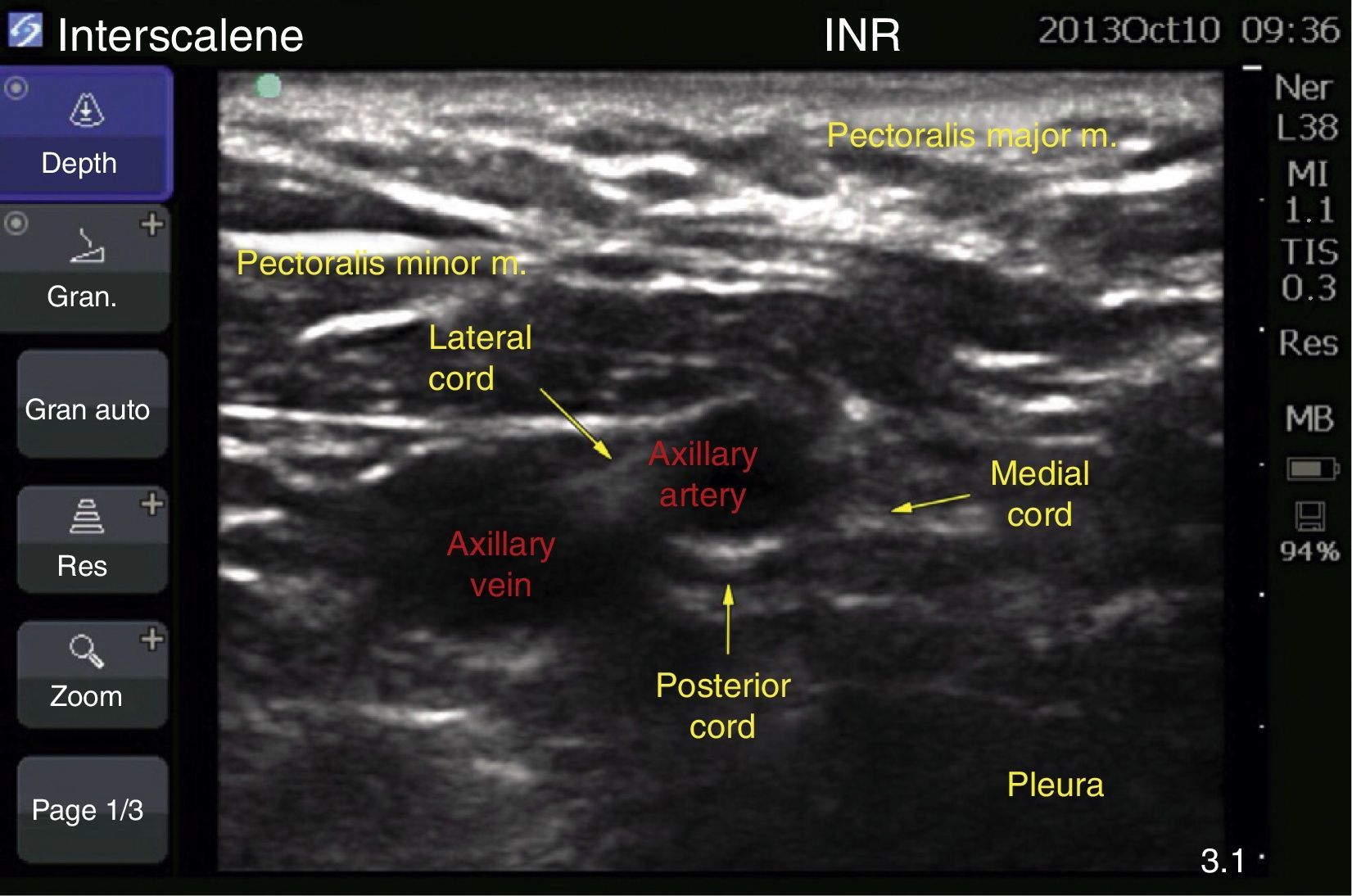
Case 3: bilateral infraclavicular blockFemale patient of 62 years, ASA II, with diagnosis of bilateral carpal tunnel syndrome, scheduled for bilateral endoscopic release. History of systemic hypertension, dyslipidemia and morbid obesity (BMI 44.5); due to these conditions, regional anaesthetics were chosen.
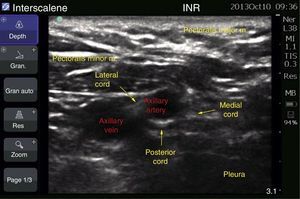
The block was guided with ultrasound (MicroMaxx Ultrasound System, SonoSite Inc., United States) and a linear transducer of 13-6MHz (HFL38, SonoSite Inc., United States). The left block was conducted first, the transducer was placed longitudinally below the coracoid apophysis and inserted on the long axis in perpendicular direction towards the posterior cord, where the local anaesthetic was administered with an insulated needle of 150mm (B Braun Melsungen AG, Stimuplex A150, Germany). A total dose of 150mg of ropivacaine at 7.5% was used, and 200mg of lidocaine 2% (equivalent to 3 and 4mg/kg of ideal weight, respectively, for a volume of 20ml on each side) (Fig. 4).
Case 4: supraclavicular block plus infraclavicular blockFemale patient of 60 years, ASA I, with diagnosis of left Quervain tenosynovitis, as well as right trigger fingers, who was scheduled for open release and for correction. With no history of relevance, she did not accept general anaesthetics due to major adverse effects in prior surgeries, therefore regional anaesthetics were chosen. The block was guided with ultrasound (MicroMaxx Ultrasound System, SonoSite Inc., United States) and a linear transducer of 13–6MHz (HFL38, SonoSite Inc., United States). The right block (supraclavicular) was conducted first with the technique described in case 2, using an insulated needle of 100mm (B Braun Melsungen AG, Stimuplex A150, Germany), ropivacaine 112.5mg+lidocaine with epinephrine 2% were administered, 200mg for a volume of 20ml, at a depth of 25mm Twenty minutes afterwards, the left block (infraclavicular) was conducted, with an insulated needle of 150mm (B Braun Melsungen AG, Stimuplex A150, Germany), with the technique described above for case 3; the following were administered: ropivacaine 75mg+lidocaine epinephrine 2% 200mg, volume of 25ml, with a depth of 60mm (equivalent to 3.3 and 7mg/kg of ideal weight, respectively, for a volume of 20ml on each side).
Systematic reviewA systematic review was preferred for the review of medical and scientific literature, as we believed that the traditional review was not adequate since the studies published in the latter were limited to the assessment or justification of a position adopted by the authors, and there is no critical assessment of the literature.
Search strategyThe search was conducted from 1 January, 1993, until 30 June, 2013. The following electronic databases were included: MEDLINE, EMBASE, ARTEMISA, LILACS, Google. The following keywords in Spanish and English were used: bilateral brachial plexus block, bilateral interscalene block, bilateral infraclavicular block, bilateral supraclavicular block, bilateral lateral supraclavicular block, bilateral axillary block, ultrasound guided bilateral brachial plexus block.
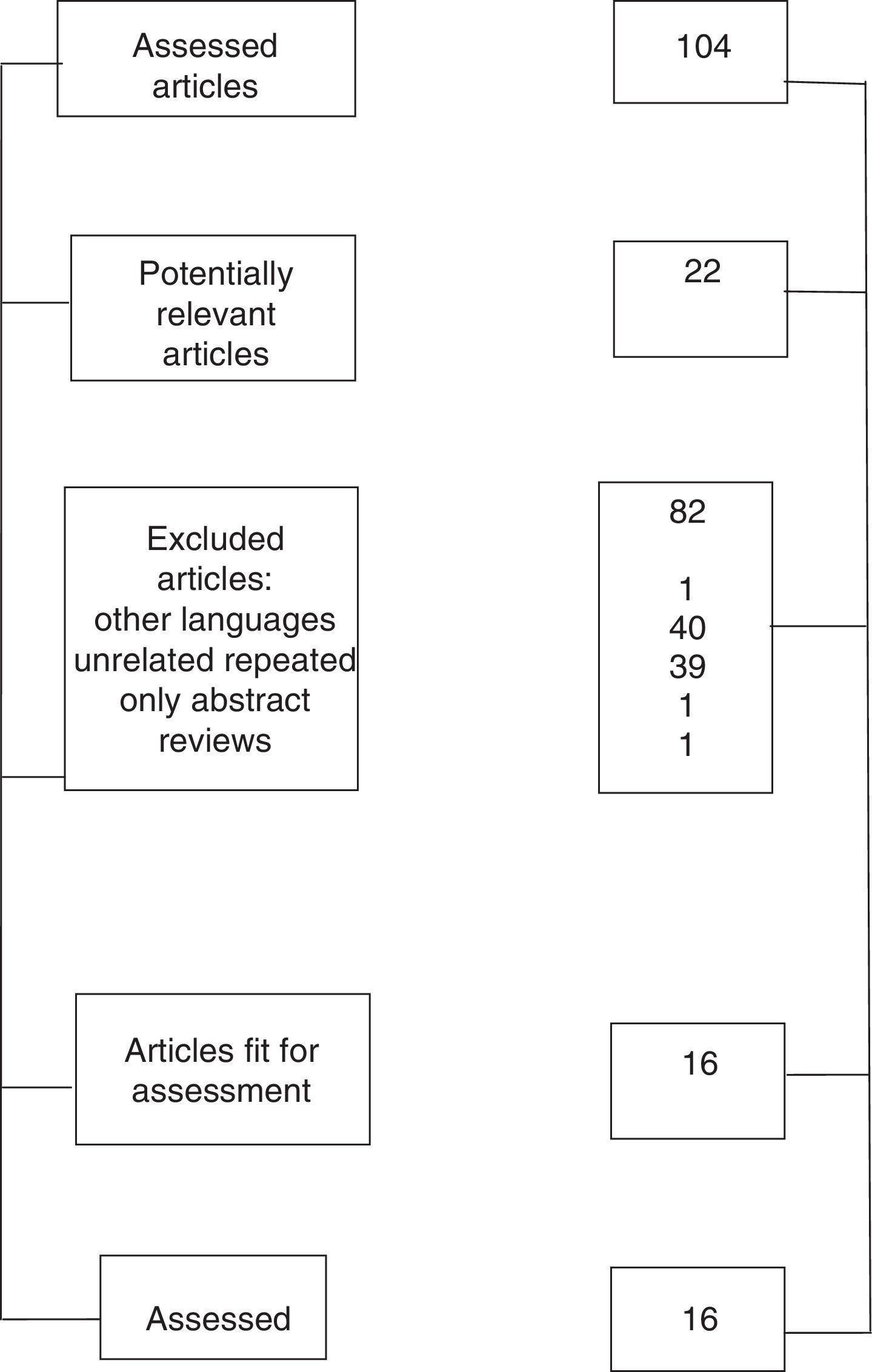
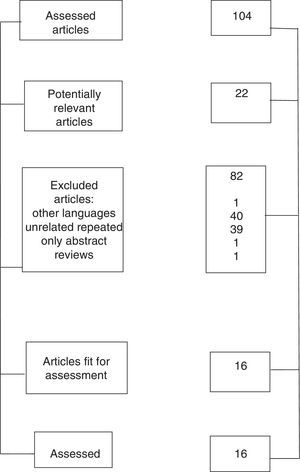
The question that the systemic review attempted to answer was whether the bilateral block of the brachial plexus is a technique that may be routinely conducted, and a total of 104 articles were obtained, 16 of which were selected (Fig. 5).9–24
The studies were selected based on the following grounds: (1) studies reporting the bilateral block technique for the brachial plexus; (2) location will be conducted with any technique (paraesthesia, neurostimulation, ultrasound); (3) any type of upper-limb surgery; (4) in English or Spanish language; (5) studies on humans; (6) patients of both sexes; (7) patients of any age; and (8) with any co-morbidity.
Once selected, they were evaluated to assess their methodological quality. Since all were case reports, the STROBE tool was used in order to issue a degree of recommendation on the application of these techniques.
DiscussionDuring the brachial plexus block, the phrenic nerve is also blocked, causing diaphragmatic hemiparesis in 20% of cases, and it may even occur in 100% of cases, mainly during the interscalene block. It is believed that the triggering mechanisms are generally caused by the rostral and ventral shape of the local anaesthetic diffusion due to the volume of local anaesthetic, which goes from 20 to 40ml, and guided with the neurostimulation technique.3 During the supraclavicular block, the incidence is 50–67%, although without affecting the forced vital capacity.4 Renes et al.5 reported the absence of diaphragmatic hemiparesis in 95% of cases when using ultrasound, since it avoids the direct administration of local anaesthetic on the phrenic nerve or the distribution of the same around the roots of C3–C5. Kessler et al.6 posited that when applying the approach below the cricoid cartilage, the block of the phrenic nerve will depend on the administered volume. The phrenic nerve has its origin in C4, with a variable contribution from the roots of C3 and C5; it descends vertically leaning on the anterior scalene muscle. Additionally, the accessory phrenic nerve, which is present in 61.8% of cases, has its origin in the subclavian nerve, the ansa cervicalis or the sternohyoid nerve, and runs laterally with the phrenic nerve in 90% of cases, and medially in 10%; thus, the phrenic nerve block contributes to the diaphragmatic hemiparesis.7,8
With the use of ultrasound, it is possible to visualise the phrenic nerve directly; it appears as a round hypoechoic structure, medial to the brachial plexus, and superficial to the anterior scalene muscle.6 If it can be visualised, directing the anaesthetic towards it or towards the root of C4 should be avoided, so as to avoid diffusion to the location of the phrenic nerve,3 and the required anaesthetic may be reduced from 20 to 5ml, achieving adequate effectiveness. In cases where the phrenic nerve cannot be visualised, it is sufficient that the local anaesthetic does not go beyond the fascia of the anterior scalene.6 In case 1, we could not visualise the phrenic nerve, therefore the approach was made on the long axis, and the tip of the needle was placed in caudal position to the trunks, to ensure greater distance from the phrenic nerve; also, on starting the injection of local anaesthetic it was controlled with ultrasound visualisation to avoid dispersion of anaesthetic beyond the fascia of the scalenes, mainly the anterior scalene, to avoid blocking it; the fascia works as a wall and prevents contact between the local anaesthetic and the phrenic nerve.2,4
The effect of bilateral diaphragmatic palsy due to anaesthetic block has not been adequately studied in humans.9 It is important because once the procedure is completed, the pulmonary forced vital capacity may be reduced by up to 60%, although it may be tolerated by the patient when the respiratory accessory muscles, such as the intercostal, scalene, and the sternocleidomastoid, are activated. These provide sufficient ventilation and avoid the patient presenting evidence of respiratory failure.
Toxicity by local anaesthetics is not present if the dose of total anaesthetic is calculated according to the body weight, and it is necessary to divide it between both procedures, waiting for some minutes between one procedure and the next to avoid a peak in the plasmatic concentration of anaesthetics and to avoid toxic levels of anaesthetic. Regional anaesthetic was applied in the 4 cases presented in this study, since general anaesthetic was not possible due to patient refusal or because it was deemed difficult for intubation.
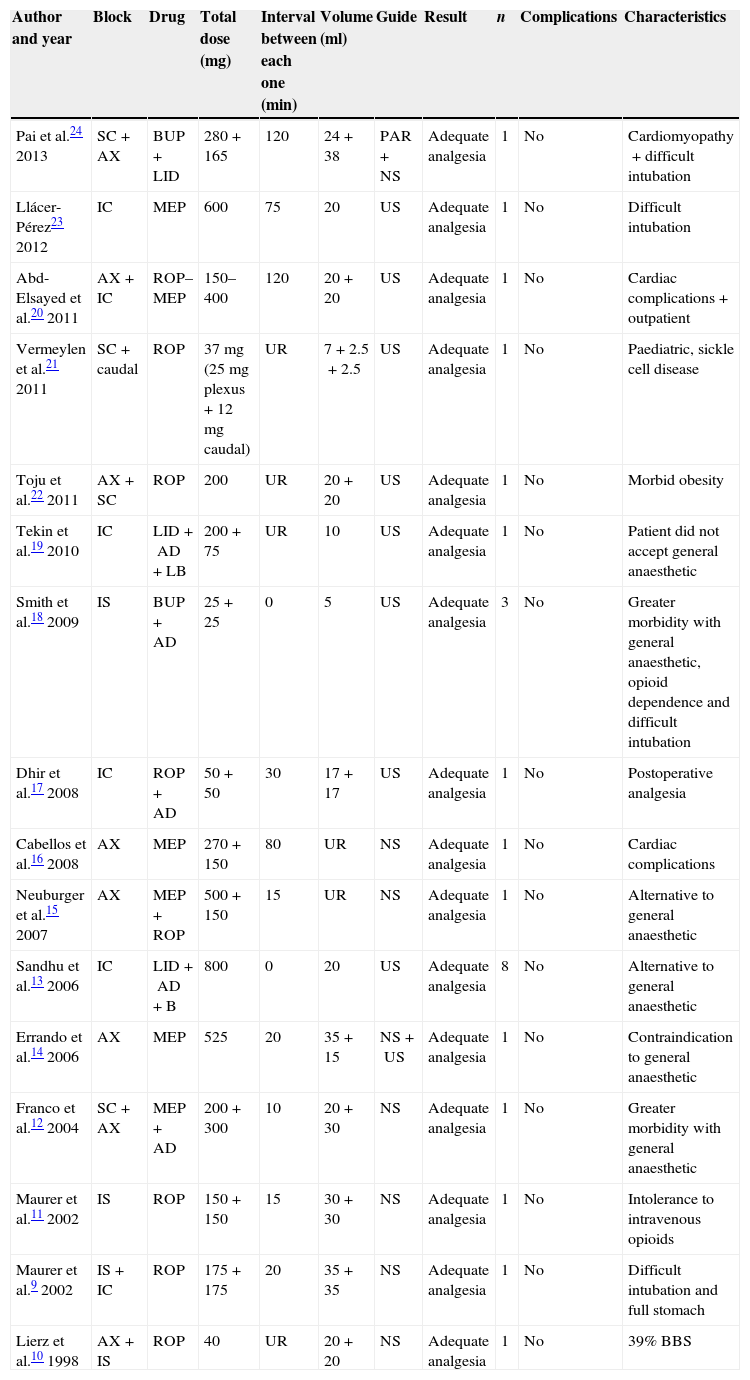
A total of 16 reports was assessed in the systemic review of bilateral brachial plexus block techniques, with a total of 26 studied patients (Table 1).19–24 Sadly, they are all case report articles, since it is difficult to conduct controlled studies through experimentation, or rather, to conduct case control studies which might confirm the sensitivity and specificity of the procedure.
Assessed articles.
| Author and year | Block | Drug | Total dose (mg) | Interval between each one (min) | Volume (ml) | Guide | Result | n | Complications | Characteristics |
|---|---|---|---|---|---|---|---|---|---|---|
| Pai et al.24 2013 | SC+AX | BUP+LID | 280+165 | 120 | 24+38 | PAR+NS | Adequate analgesia | 1 | No | Cardiomyopathy+difficult intubation |
| Llácer-Pérez23 2012 | IC | MEP | 600 | 75 | 20 | US | Adequate analgesia | 1 | No | Difficult intubation |
| Abd-Elsayed et al.20 2011 | AX+IC | ROP–MEP | 150–400 | 120 | 20+20 | US | Adequate analgesia | 1 | No | Cardiac complications+outpatient |
| Vermeylen et al.21 2011 | SC+caudal | ROP | 37mg (25mg plexus+12mg caudal) | UR | 7+2.5+2.5 | US | Adequate analgesia | 1 | No | Paediatric, sickle cell disease |
| Toju et al.22 2011 | AX+SC | ROP | 200 | UR | 20+20 | US | Adequate analgesia | 1 | No | Morbid obesity |
| Tekin et al.19 2010 | IC | LID+AD+LB | 200+75 | UR | 10 | US | Adequate analgesia | 1 | No | Patient did not accept general anaesthetic |
| Smith et al.18 2009 | IS | BUP+AD | 25+25 | 0 | 5 | US | Adequate analgesia | 3 | No | Greater morbidity with general anaesthetic, opioid dependence and difficult intubation |
| Dhir et al.17 2008 | IC | ROP+AD | 50+50 | 30 | 17+17 | US | Adequate analgesia | 1 | No | Postoperative analgesia |
| Cabellos et al.16 2008 | AX | MEP | 270+150 | 80 | UR | NS | Adequate analgesia | 1 | No | Cardiac complications |
| Neuburger et al.15 2007 | AX | MEP+ROP | 500+150 | 15 | UR | NS | Adequate analgesia | 1 | No | Alternative to general anaesthetic |
| Sandhu et al.13 2006 | IC | LID+AD+B | 800 | 0 | 20 | US | Adequate analgesia | 8 | No | Alternative to general anaesthetic |
| Errando et al.14 2006 | AX | MEP | 525 | 20 | 35+15 | NS+US | Adequate analgesia | 1 | No | Contraindication to general anaesthetic |
| Franco et al.12 2004 | SC+AX | MEP+AD | 200+300 | 10 | 20+30 | NS | Adequate analgesia | 1 | No | Greater morbidity with general anaesthetic |
| Maurer et al.11 2002 | IS | ROP | 150+150 | 15 | 30+30 | NS | Adequate analgesia | 1 | No | Intolerance to intravenous opioids |
| Maurer et al.9 2002 | IS+IC | ROP | 175+175 | 20 | 35+35 | NS | Adequate analgesia | 1 | No | Difficult intubation and full stomach |
| Lierz et al.10 1998 | AX+IS | ROP | 40 | UR | 20+20 | NS | Adequate analgesia | 1 | No | 39% BBS |
AD: adrenaline; BGA: balanced general anaesthetic; AX: axillary; B: bicarbonate; BUP: bupivacaine; IC: infraclavicular; IS: interscalene; LBUP: levobupivacaine; LID: lidocaine; MEP: mepivacaine; NS: neurostimulation; UR: unreported; PAR: paraesthesia; ROP: ropivacaine; SC: supraclavicular; BBS: burned body surface; CRPS: complex regional pain syndrome; US: ultrasound.
A qualitative analysis of data was made from the analysed information, which enabled us to answer our research question. The analysis reveals the following premise: there was no complication or major respiratory effect requiring endotracheal intubation in any of the cases. The bilateral use would be indicated in cases where it is important to avoid the morbidity derived from general anaesthetics due to patient co-morbidities, mainly at the cardiorespiratory level, or rather when there are foreseeable technical difficulties with the airways due to difficult intubation, or when the patient does not accept the administration of general anaesthetic.
It would also be indicated so as to achieve adequate postoperative analgesia, particularly in patients with a history of major adverse effects from the use of intravenous opioids or in cases of addiction to them. All the authors reviewed believe that the use of bilateral brachial plexus block increases the benefits, by achieving adequate analgesia in selected patients without increasing procedural risks. This is obvious in our cases, since there were no complications of any kind.
The qualitative analysis of data obtained allows us to issue the following recommendations: (1) under specific circumstances, it may be the anaesthetic technique of choice, i.e., in patients who due to their co-morbidities present a greater risk for the administration of general anaesthetics; (2) in patients with foreseeably difficult intubation; (3) the presence of complications is not greater than when a unilateral technique is applied; (4) the calculation of the total dose of local anaesthetic without reaching the maximum dose does not reach toxic levels and it maintains adequate analgesia (the total dose is calculated per kilogram of weight and divided between each block), since no toxic plasmatic concentrations are reached in this procedure; (5) wait for a reasonable time between each block to avoid the plasmatic peak of the anaesthetic from reaching toxic levels in the case of immediate administration, and (6) the procedure must always be conducted with ultrasound guidance to reduce the volume of local anaesthetic and, therefore, the total dose administered; furthermore, the diffusion of the dose may be visualised and modified to avoid a phrenic nerve block.
ConclusionIn spite of the scant current evidence, this study shows that we can stop considering bilateral brachial plexus block techniques as contraindicated. When they are applied by experienced hands and with ultrasound guidance, they constitute a safe alternative, with an adequate risk-benefit balance.
Conflict of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: Mejia-Terrazas GE, Garduño-Juárez MA, Limón-Muñoz M, Torres-Maldonado AS, Carrillo-Esper R. Bloqueo bilateral del plexo braquial. Reporte de casos y revisión sistemática de la literatura. Cirugía y Cirujanos. 2015;83:312–318.