Chromohyphomycosis, also known as chromoblastomycosis, is a disease that affects body areas unprotected by clothing; the lower limbs are the most affected.1 The nasal cavity is rarely affected by chromoblastomycotic lesions, and there have been only three cases described in this region.1-3 This infection is caused by a variety of fungi, which display a dark green color on the surface of culture medium due to the hyphal layer, and are almost black in depth. These fungi are called Dematiaceous and have a brownish color in the histological analysis, when stained with hematoxylin-eosin (HE).4 Septal chromohyphomycosis is rare, and its diagnosis is based on histopathological analysis and culture.5
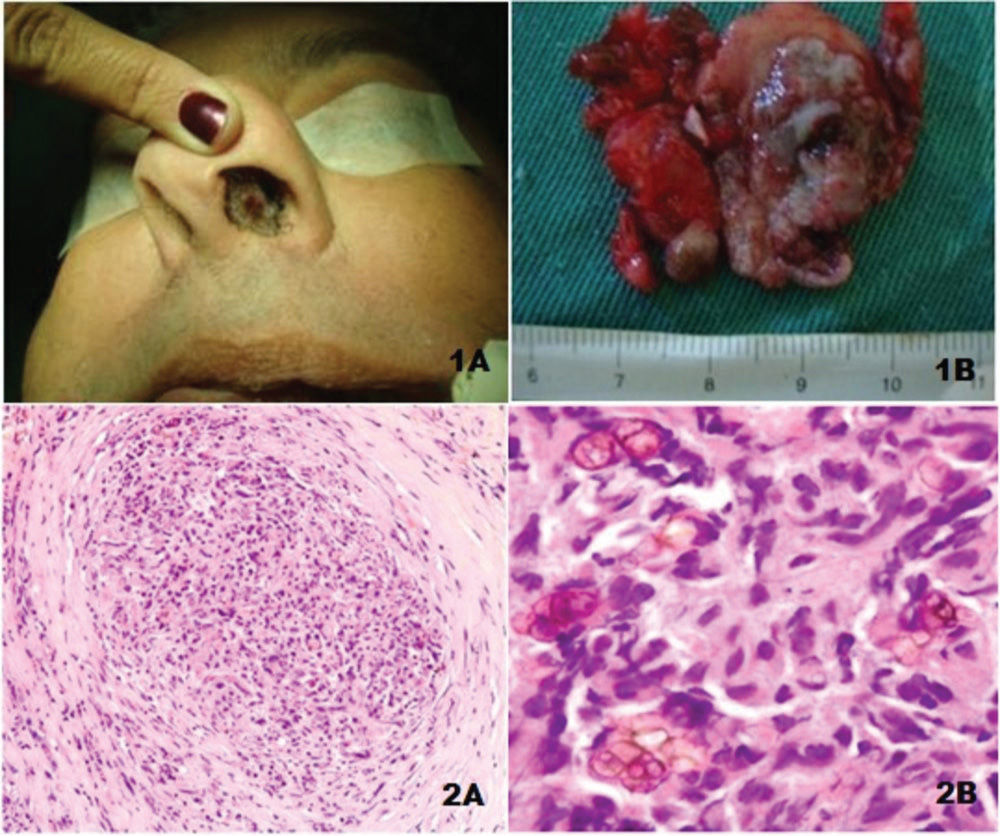
Case reportA 52 years old male merchant , born in São Paulo, denied having been to the countryside, reported the presence of obstruction and rhinorrhea and a lesion in the left nasal cavity for one month. He had developed kidney failure due to polycystic kidney disease, underwent hemodialysis for five years, and underwent a kidney transplant two years before. Due to the transplant, he was immunosuppressed with tacrolimus and corticosteroids. He had a round lesion in the anterior septal region, of granular appearance, 1.5cm in diameter (Fig. 1A). He had similar smaller asymptomatic lesions distributed throughout the nasal cavity and hard palate. The septal lesion was excised with the mucosa through the anterior nasal cavity without complications (Fig. 1B). After removal of the largest nasal lesion, treatment was performed with antifungal agents.
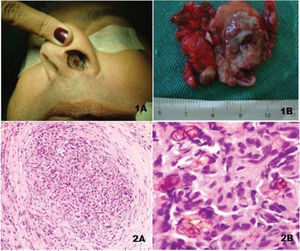
Histopathological analysis with HE showed a granulomatous chronic inflammatory process, with rounded brownish colored fungi (yeasts) some with septae (Figs. 2A and 2B), indicative of chromohyphomycosis. Specific staining for fungi was not necessary. Analysis of fungal growth in the culture medium demonstrated Fonsecaea pedrosoi, which is characterized by having Rhinocladiella-type sporulation, sometimes associated with the Cladosporium type.4
DiscussionChromohyphomycosis is a granulomatous disease, whose infectious agents are several dark-colored fungi, most commonly the Fonsecaea pedrosoi. They are common saprophytic forms found in the soil and decomposing vegetation. Trauma is the gateway for these agents. The disease primarily affects men, usually rural workers, and, according to Carrión,6 it occurred in 96% in their series, with a men to women ratio of 20:1. Lesions start by affecting the feet, then the leg, and reach the upper limbs; they can reach several other organs, such as lungs, conjunctiva, brain, and throat. Although the present patient denied any injury or trauma in the nasal region, t the possibility of trauma due to the habit of scratching could not be dismissed.
Chromohyphomycosis, occurring primarily in regions other than the extremities, is a rare disease. Londero et al.1 in 1968 and Zaror et al.2 in 1987 isolated Fonsecaea pedrosoi from the septal lesion, while Nakamura et al.3 isolated Phialophora verrucosa. Fonsecaea pedrosoi is the most common species in chromohyphomycosis (84%, according to Carrión).6 When examined by the dermatology service, the present patient had lesions,only in the nasal and palate regions, with none on the lower limbs.
The diagnosis of dematiaceous mycosis, a term introduced by Symmers to represent diseases caused by pigmented fungi, can be made by direct examination with lactophenol cotton blue or by histopathology analysis, stained by HE, which demonstrates the presence of the characteristically brownish fungus inside or outside the giant cells.4 Culture in Sabouraud medium allows for the species identification, through the analysis of the sporulation type.4 The differential diagnosis can be made with rhinosporidiosis, leishmaniasis, and paracoccidioidomycosis5 (very rare in the nasal cavity).
The recommended treatment for the patient after the surgical removal of lesions was itraconazole for three months. As there was no response, liposomal amphotericin B was prescribed; after one month of treatment, the patient still had fungi in the direct mycological examination, and there was no decrease in the size of the remaining lesions. Thus, oral voriconazole was prescribed. This antifungal agent is a second-generation triazole, a synthetic derivative of fluconazole, and has advantages over other antifungal agents, especially in cases of amphotericin resistance. It was prescribed for six months at a dose of 6mg/kg every 12 hours, resulting in significant clinical improvement with complete lesion remission.
The prognosis of chromohyphomycosis is usually good, except when it affects viscera. It also depends on the patient’s immune status.
Final considerationsChromohyphomycosis in the nasal septum is a rare disease, and it is difficult to establish its diagnosis in this site. Patient immunosuppression favored lesion development.
Conflicts of interestThe authors declare no conflicts of interest.