Multiple symmetrical lipomatosis (MSL), also known as Madelung’s disease, benign symmetrical lipomatosis, or Launois-Bensaude adenolipomatosis, is a rare benign disease of unknown pathogenesis.1,2
It was mentioned in the literature for the first time by Bordie in 1846 and by Madelung in 1888. Ten years later, 65 more cases were described by Launois-Bensaude, and the disease received his name.1,3
The disease is more commonly observed in white males of Mediterranean origin, aged 30 to 60 years, with a male:female ratio of 15:1 to 30:1.1,2 Chronic alcoholism is associated with over 90% of cases,1 in addition to metabolic abnormalities such as hyperuricemia, hyperlipidemia, glucose intolerance, and others such as macrocytic anemia, renal tubular acidosis, and polyneuropathy.2,3
It is clinically characterized by the deposition of multiple symmetric masses of unencapsulated adipose tissue in the upper chest and neck region, and it is classified into two types.3 Type I presents lipomatous masses in the parotid, cervical, suprascapular, and deltoid regions, and there may be deep involvement. Type II presents diffuse lipomatosis, similar in appearance to common obesity; it is most common morphology in females.4
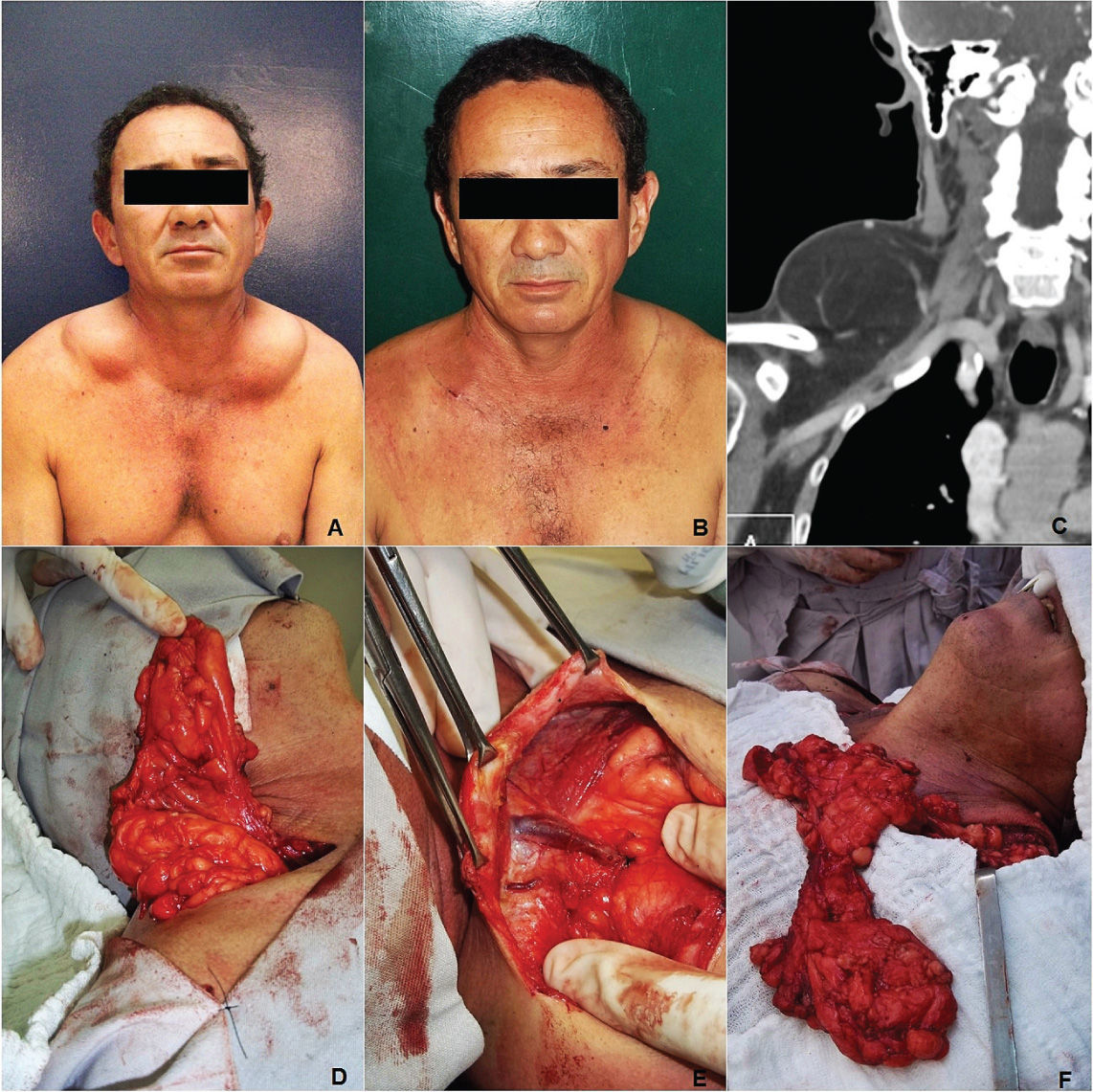
A case of multiple symmetric lipomatosis type I is described, affecting the supraclavicular region, bilaterally.
Case presentationA male patient, 47 years old, white, without comorbidities, alcoholic for 20 years, presented to this unit with a complaint of bulging in the bilateral supraclavicular region, painless, which had been progressively growing for the past five years.
At physical examination, he showed good overall status, with bilateral supraclavicular mass of soft consistency, painless, measuring 10 × 6cm to the left and 12 × 8cm to the right (Fig. 1A). The computed tomography (CT) confirmed the presence of a symmetrical supraclavicular mass, whose density was compatible with fat (Fig. 1C). The mass was surgically removed, and the anatomopathological analysis of the specimen evidenced the presence of lipomatosis (Figs. 1D, 1E, 1F). To date, the patient has progressed well without recurrence, and outpatient follow-up has been maintained (Fig. 1B).
DiscussionIn spite of the uncertain etiology of MSL, its pathogenesis is believed to be related to the dysfunction of cyclic AMP in adipocytes and levels of catecholamines responsible for lipolysis.3 Alcohol also appears to play a role in the adipocyte hyperplasia process2 in genetically susceptible individuals through the pro-lipogenesis, antilipolytic, and decreased lipid oxidation effects. Other studies have also suggested the presence of mitochondrial inheritance through mutation of the maternal gene.3,5
The diagnosis is attained by patient history, physical examination, biopsy, and laboratory and imaging tests. Complementary tests are important to discard differential diagnoses such as multiple familial lipomatosis, sarcomas, angiolipomas, lipoblastomas, neurofibromatosis, Dercum’s syndrome, Hanhart syndrome, polydysplasia syndrome, lymphoproliferative disorders, and muscular dystrophies.2,3
CT is considered the imaging examination of choice for diagnosis, preoperative staging, and postoperative follow-up, due to the overlap of findings with magnetic resonance imaging and its lower cost.3
The palliative treatment is surgical through lipectomy or liposuction, with good results, although recurrences are common due to the difficulty of complete tumor excision, as they are not encapsulated.2,3 Some studies have described a clinical treatment with β2-agonist, in order to increase the adrenergic lipolysis and reduce the accumulation of fat, but with questionable efficacy.2 Although weight loss and alcohol withdrawal appear to have no effect on disease progression, these measures associated with surgery can decrease the recurrence rate,6 as a longitudinal study showed that the amount of alcohol consumed is directly associated with the onset of the disease.3
The prognosis can be good if treated early; morbidity and mortality are more often associated with complications of alcoholism than with the fat deposits directly.3 The lesions hardly ever become malignant; however, they may evolve with compression of the larynx and trachea and development of neuropathies.2
Final commentsThe identification of this rare disease, the appropriate investigation for the exclusion of differential diagnosis, and early surgical approach as observed in the present case, are important to prevent future complications.
Conflicts of interestThe authors declare no conflicts of interest.