Introducción: La evaluación de la calidad de la atención del recién nacido con complicaciones es un elemento indispensable para las estrategias de mejora orientadas a reducir las tasas de mortalidad neonatal. El objetivo de este trabajo fue evaluar la calidad de atención técnica e interpersonal en el manejo de la taquipnea transitoria del recién nacido (TTRN) de pacientes afiliados al Seguro Médico Siglo XXI.
Método: Se realizó un estudio transversal en 61 hospitales de la Secretaría de Salud, que durante el primer semestre de 2011 reportaron al menos dos casos de TTRN. Se analizaron diferentes variables con respecto a la madre, el embarazo, el nacimiento y las complicaciones neonatales, así como intervenciones realizadas al recién nacido y condiciones de salud al egreso. Para medir la calidad de atención, se definieron y validaron indicadores de calidad en los ámbitos de la prevención, diagnóstico y tratamiento.
Resultados: Se analizaron 256 expedientes de casos con diagnóstico de TTRN. El 8.9% de las madres tenía alguno de los factores de riesgo (asma, diabetes) y el 53.5% presentó complicaciones en el embarazo. El 60% de los casos de TTRN nacieron por cesárea; un tercio tuvieron bajo peso al nacimiento y el 14% fueron trasladados a otro hospital. En cuanto a los indicadores de calidad, en el rubro de prevención se identificó que en más del 90% se registraron los factores de riesgo (tabaquismo, asma, parto por cesárea); los de diagnóstico reflejaron que en el 86-98% se buscaron manifestaciones de insuficiencia respiratoria. Los de tratamiento lograron cifras satisfactorias para las medidas de monitorización y soporte.
Conclusiones: Los resultados permiten considerar que la mayoría de los casos con TTRN recibieron un tratamiento apropiado. Es recomendable desarrollar estrategias efectivas, como reducir la creciente tasa de partos por cesárea, para prevenir la TTRN.
Background: Evaluation of the quality of care of the newborn with complications is an indispensable element for the improvement of strategies directed to reduce newborn mortality rates. The aim of this work was to evaluate the quality of technical and interpersonal care in the management of transient tachypnea of the newborn (TTN) of patients affiliated with the program ‘‘Medical Insurance Siglo XXI’’.
Methods: A cross-sectional study was conducted in 61 hospitals affiliated with the Health Ministry with at least two cases of TTN during the first semester of 2011. Variables such as mother’s health, pregnancy, birth and birth complication characteristics were analyzed. Also, newborn interventions and health conditions upon discharge were included. To measure the quality of care according to prevention, diagnosis and treatment, quality indicators were defined and validated. Results: We analyzed 256 case files with a diagnosis of TTN; 8.9% of the mothers presented risk factors (asthma, diabetes) and 53.5% had complications during pregnancy. There were 60% of cases with TTN born by cesarean delivery; one third of these children had low birth weight and 14% were transferred to another hospital. As for the quality indicators in the area of prevention, more than 90% of risk factors (smoking, asthma, cesarean delivery) were identified. Diagnostic indicators showed that 86-98% of respiratory distress symptoms were sought. Indicators of treatment achieved satisfactory figures for monitoring and support measures.
Conclusions: Prevention, diagnosis and treatment indicators made it possible to consider that most TTN cases received appropriate treatment. It is advisable to develop effective strategies to prevent TTN, such as increasing efforts to reduce the increasing rates of cesarean deliveries.
1. Introduction
Poverty and inequality in access to health services are determinants of mortality in young ages. Newborns are the most vulnerable. In 2006, The System of Social Protection in Health implemented Medical Insurance for a New Generation which, in 2013, was renamed as Medical Insurance Century XXI (SMSXXI). SMSXXI finances complete medical care to children from birth up to 5 years of age without affiliation with social security. Beneficiaries of the SMSXXI have the right to receive preventive medical services and outpatient and hospital medical care without any fee for services.
SMSXXI, together with the Protection Fund against Catastrophic Expenses, has placed special emphasis on financing diseases from the first month of life, which is when the greatest number of deaths in those <5 years of age occurs.1,2 In addition to the financing, the Ministry of Health, together with other institutions from the Mexican health sector, has come up with management protocols that include recommendations for diagnostic and treatment procedures so as to reduce the variability in clinical practice and improve the quality of medical care for diseases covered by the SMSXXI, among which is transitory tachypnea of the newborn (TTN).3
TTN is a non-infectious respiratory process caused by a delay in the reabsorption of fetal pulmonary fluid. This condition occurs in 0.3-2.0% of term newborns or late premature newborns and comprises up to 50% of the cases of respiratory distress admitted to the sick nurseries or neonatal intensive care units. Infants born via cesarean section or born rapidly vaginally (labor with duration of 3 h or less) have a greater risk of having excess lung fluid. This is as a result of not having gone through the labor phase and the lack of catecholamines secreted during labor, which stimulate the epithelial Na+ channels. During labor and birth, the pulmonary epithelium of the newborn, which during pregnancy actively secretes chlorine (Cl–) and fluid into the alveoli, undergoes a change characterized by the active absorption of Na+ and fluid so as to remove the latter, which is brought about by the presence of catecholamines. TTN results in the alveoli remaining “moist” when adequate reabsorption does not take place. The result is that the alveoli retain fluid, compromising the gaseous exchange that favors hypoxemia, accumulates in the interstitium until it is removed by the lymph vessels and passes into the circulation. It has also been mentioned that there is genetic predisposition of beta adrenergic hyposensitivity.4
TTN begins in the first hours of birth and is characterized by the presence of tachypnea (respiratory rate >60x’), respiratory failure and increase in oxygen requirement with normal or slightly increased CO2 levels. It is generally a self-limiting process that resolves in ~24-72 h.5-7 Fluid accumulation causes interstitial edema and decrease in pulmonary distention, which causes tachypnea and partial bronchiolar collapse. In the course of hours, the fluid is progressively removed, which improves oxygenation and decreases the tachypnea. Criteria for diagnosis and treatment are clearly established in the literature.8,9
TTN has a benign course. However, its high frequency among neonatal morbidity justifies that the quality of care provided to newborns with this condition be evaluated. A growing incidence of the risk of TTN and other respiratory diseases in the newborn has been noted due to the increase in the rate of cesarean births.10 In Mexico, evaluation of the quality of care in neonatal diseases through indicators is emerging and the studies performed on newborns with respiratory failure11 and with necrotizing enterocolitis12 have identified significant margins for improvement.
Evaluation of the quality of care of the newborn with complications is an essential element for the design and implementation of strategies for improvement aimed at reducing the rates of neonatal mortality in Mexico.
The objective of this study was to design technical quality indicators and to evaluate the quality of care received by the newborns affiliated with the SMSXXI with diagnosis of TTN.
2. Methods
2.1. Construction of quality of care indicators
Construction of quality of care indicators for TTN included review of the literature and of the clinical guidelines repository. Literature review included Medline, Ovid and Cochrane Library databases. Management protocols established by the Department of Health, clinical guidelines (institutional and from other countries) and systematic review of the literature related with the management of TTN were also reviewed. Three pediatricians with experience in neonatology, guided by one of the researchers (LJG), examined the literature for its scientific value and via consensus elaborated the list of indicators. Additionally, the working group took into consideration the feasibility of having the clinical information available to be able to carry out the evaluation using the medical record.
The indicators covered three areas of evaluation: identification of risk factors for TTN, clinical diagnostic procedures and treatment. Risk factor indicators were related to the mother (smoking or asthma), type of birth (cesarean) and birth with rushed labor of <3 h. The indicators for diagnosis were the intentional search for tachypnea, nasal flaring, grunting, costal retractions and request for chest x-ray, arterial blood gases, blood count and pulse oximetry. Treatment indicators were the parenteral administration of solutions, recording and monitoring of temperature and administration of supplemental oxygen.
2.2. Evaluation of the quality of care
Evaluation of the technical quality was done by means of a descriptive cross-sectional study in 61 hospitals affiliated with the Ministry of Health in the federal entities and national institutes that provide care to children affiliated with SMSXXI and who cared for at least two cases of TTN during the first semester of 2011. The information was collected in a sample of 250 medical records of newborns with TTN. The records examined were the most recent at the time of the visit for their examination.
The variables recorded are as follows:
1. Mother’s characteristics: age, marital status, occupation, reproductive history, medical history and family income
2. Characteristics of the pregnancy: treatment of infertility, gestational age at the start of prenatal care, place of prenatal care, institution that provided prenatal care, complications during prenatal care, treatment of the mother with steroids and single or multiple pregnancy
3. Characteristic of the birth: gender, gestational age at birth, type of birth, time of labor, use of antibiotics, use of steroids during labor
4. Presence of neonatal complications: surgical diagnosis, infections, persistence of ductus arteriosus, hematological diagnosis, periventricular leukomalacia, intracranial hemorrhage, retinopathy of the newborn, other diagnoses of the CNS, oxygen dependence at 36 weeks
5. Interventions: ultrasound results, use of surfactant, hyperalimentation, duration of phototherapy, use of central venous catheter, duration of assisted ventilation, duration of oxygen supplementation, transfusion, use of indo-methacin, cardiorespiratory resuscitation, administration of cardiovascular agents, use of anticonvulsants, antimycotic therapy, use of xanthines
6. Conditions at the time of discharge: age of gestation upon discharge, average daily weight gain, reason for discharge
2.3. Collection of information
An ad hoc tool was generated for the collection of the information, which was given by trained personnel in the selected hospital departments. The tool was evaluated in a pilot study to identify the feasibility of obtaining the information and ability to manage the tool. The Ethics and Research Committee of the Hospital Infantil de México Federico Gómez (HIMFG) authorized the study and the National Committee of Social Protection in Health provided support for collection of the information in the selected hospitals.
2.4. Statistical analysis
The information was analyzed using descriptive analysis. The analysis was performed using the statistical package Stata 8.0 (Stata Corp., College Station, TX).
3. Results
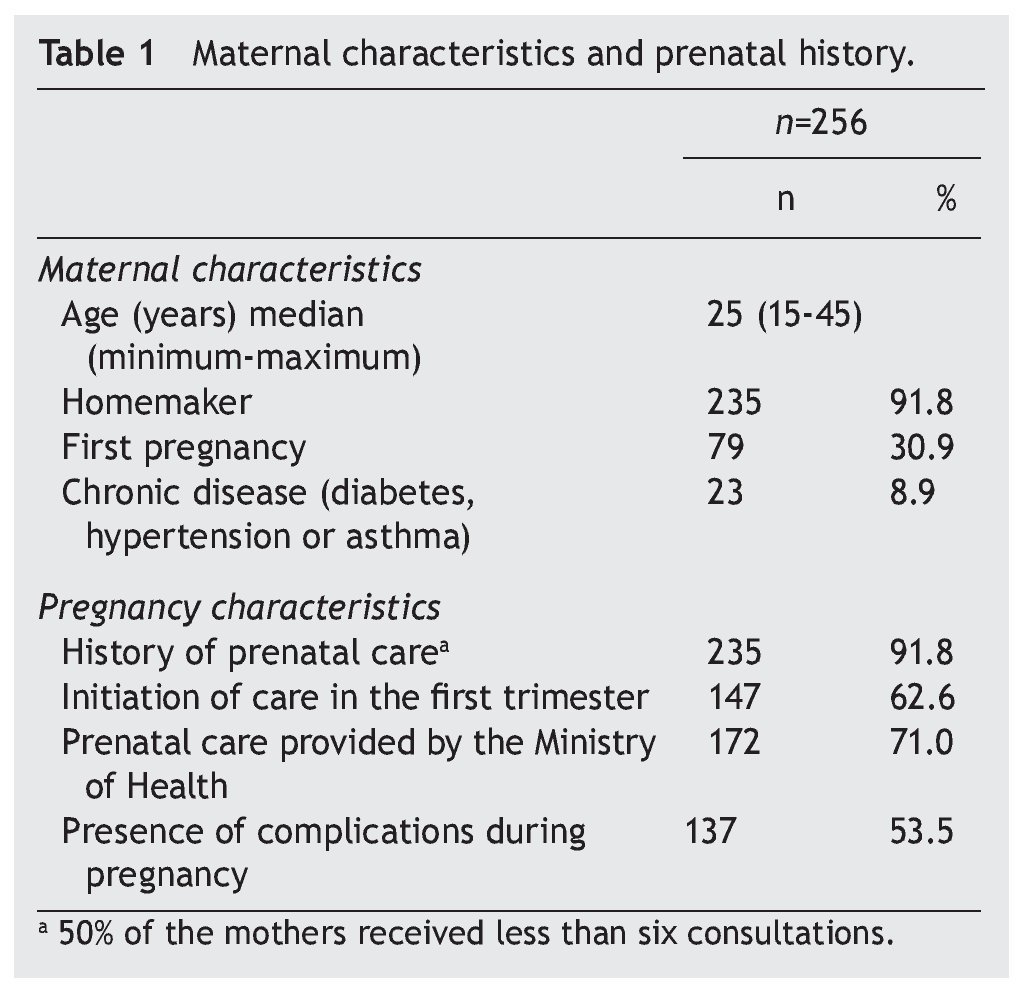
The study included 256 cases with a diagnosis of TTRN and who were cared for in 61 hospitals of the Ministry of Health. Table 1 shows the characteristics of the mother and the prenatal history. It is observed that young mothers who were housewives with an average age of 25 years predominated. There were 33% primigravidas; 8.9% had some chronic disease (diabetes, asthma, or hypertension.) The majority (71%) came for prenatal care at the clinics of the Ministry of Health and half had received at least six prenatal consultations. Also, half of the mothers had some complication during pregnancy.
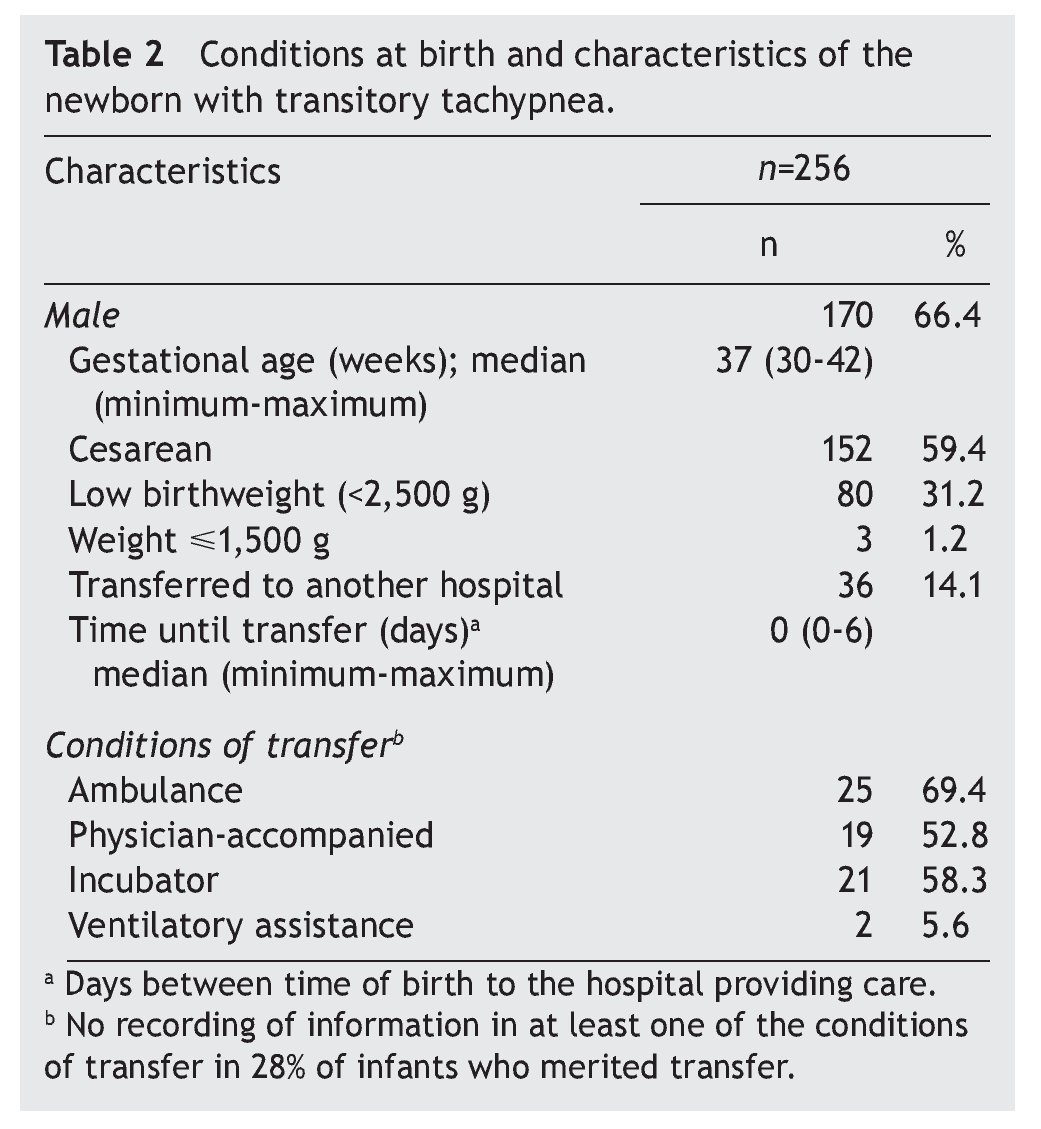
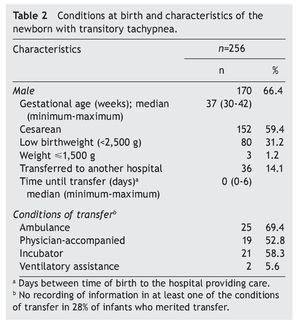
Table 2 describes the characteristics of the newborn. The majority were males. The average gestational age was 37 weeks and a high percentage of newborns (59.4%) were born by cesarean section. A third had low weight at birth and 14% were transferred to another hospital because of complications. In most cases the transfer was done between the day of birth and 6 days later. The majority were transferred via ambulance (69.4%), accompanied by a physician (52.8%) and in an incubator (58.3%).
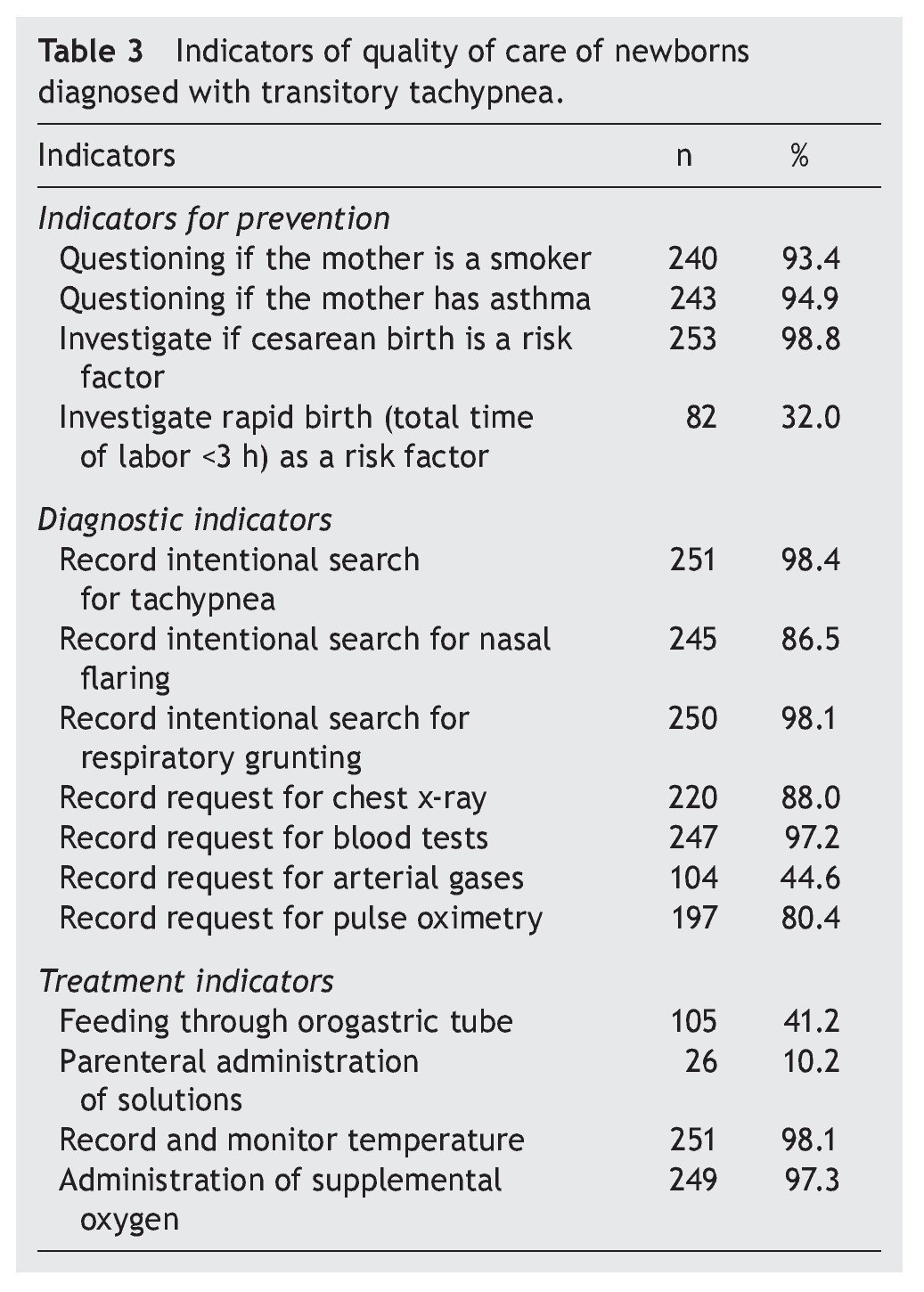
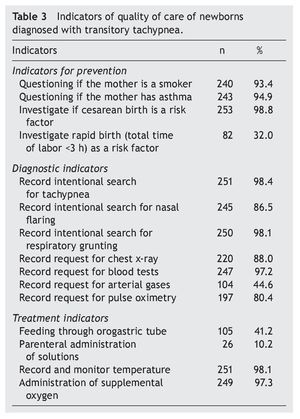
For the TTN quality of care indicators, the following results were obtained. With respect to the component of prevention indicators, it was identified in >90% if the mother smoked, if she had asthma, and if the delivery method was cesarean. With reference to diagnostic indicators, the intentional search for respiratory failure (nasal flaring, tachypnea, grunting) varied from 86-98%. The request for basic diagnostic studies (chest x-ray, blood count and pulse oximetry) was done in a high percentage of the cases with the exception of arterial blood gases (44.6%). The indicators for treatment, basically measures of support and monitoring (temperature and supplemental oxygen), were used in the majority of the cases, whereas the administration of parenteral solutions was done only in 10% and feeding with an orogastric tube in 41% (Table 3).
4. Discussion
The results observed for the indicators for prevention, diagnosis and treatment allow us to consider that a large part of the cases of patients with TTN received appropriate treatment, although some required transfer to another hospital, possibly due to complications.
The mothers presented some of the risk factors mentioned in the literature such as being primigravida, having some chronic disease (asthma13,14 or diabetes15), having had complications during pregnancy and giving birth via cesarean section.
A large proportion of newborns (almost 60% of the cases) were born via cesarean section. The increase in the number of cesarean births has multiple consequences, among these TTN because fetal lungs are filled with fluid that needs to be absorbed rapidly to allow gaseous exchange. Cesarean birth, on the other hand, reduces the risk of neonatal asphyxia, trauma and meconium aspiration and, on the other hand, increases the risk of respiratory distress secondary to TTN, surfactant deficiency and pulmonary hypertension.8
Different reports recommend postponing elective cesarean section until after 38-39 weeks of gestation (WG) so as to reduce the risk of neonatal mortality.16
The frequency of TTN is greater in the term newborn. Because of this, it is notable that there were some cases of TTN with gestational age <37 weeks and that in a third of the cases low birth weight was reported. Management of these cases should be geared towards appropriate respiratory support to facilitate respiratory transition and reduce the possibility of complications. It is advisable to delve into focused studies to determine the long-term impact of the shortness of breath that occurs in premature newborns.17
The fact that 14% of the cases required transfer to another hospital, with support of an incubator and accompanied by a physician, indicates deterioration of the newborn, appearance of some complication, or that the diagnosis was not performed appropriately. The case initially believed to be TTN may have progressed towards another respiratory complication because the transfer was carried out between 0 and 6 days and TTN is a self-limiting condition (within a period of 72 h). This indicates the need to perform a differential diagnosis with other respiratory problems of the newborn such as sepsis, pneumonia and respiratory distress syndrome.
The indicators for prevention form part of the routine information recorded in the clinical file, which reflects that there is knowledge of these factors. However, the risk factor of rushed labor was not satisfactorily recorded.
In the large part of cases, the diagnostic indicators such as a search for tachypnea, nasal flaring and respiratory grunting allow for clinically establishing the degree of severity of the respiratory failure and establish the differential diagnosis with other diseases such as respiratory distress syndrome or meconium aspiration syndrome. In the cases with TTN, it is important to observe that it is spontaneously resolved. The indicators of laboratory studies, in this case complete blood count, could provide guidance for ruling out stress or infection (leukocytosis or bands), bacterial infection (neutropenia), anemia (low hemoglobin) and sepsis (thrombocytopenia). The request for a chest x-ray allows for ruling out abnormalities in the lungs and pulse oximetry helps in deciding if oxygen is required. If the newborn’s condition deteriorates, transfer to an intensive care unit is mandatory.
Treatment indicators that were selected for evaluating the quality of care were basically monitoring and support of respiratory function. Treatment of TTN is support because this disease is usually self-limiting. From the clinical point of view, TTN begins early and the patient improves with time as opposed to other respiratory disorders of the newborn such as sepsis or pneumonia, which begin late, whereas respiratory distress syndrome begins early in the premature newborn but its evolution is not towards spontaneous improvement.
It is possible that newborns requiring parenteral solutions and feeding with an orogastric tube had more serious conditions. It was decided to not use the criteria of antibiotic use and/or diuretic use because it has not been demonstrated that the health status significantly improves in cases with TTN.18-20 Some reports have suggested administration of corticosteroids 48 h before elective cesarean section in patients of 37-39 WG to reduce the incidence of TTN; however, there is no convincing evidence in this regard.
The study was based on a sample of medical records which, in a way, limits the validity of the results because the records may lack the necessary information for the purpose of interest (of evaluation or of investigation). In the present study the information available in the clinical record did not allow for a differential diagnosis of TTN with other respiratory diseases of the newborn. The information also was limited with reference to the clinical history and the types of complications that the mother experienced during pregnancy were not appropriately documented. It is recommended to continue with studies focused on developing reliable and valid measures of quality to provide information that help in decision making and the improvement of the performance of neonatology services.
Prevention, diagnosis and treatment indicators allowed identification that most cases with TTN received appropriate treatment. However, it is recommended to develop effective strategies to prevent TTN and to increase efforts to reduce the increasing rate of births by caesarean section. It is also reasonable to develop strategies to improve recording of data in the clinical file and continue efforts to regularly assess the quality of care through indicators.
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of data. The authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consent. The authors declare that no patient data appears in this article.
Conflict of interest
The authors declare no conflict of interest of any nature.
Received 17 December 2014;
accepted 16 January 2015
☆ Please cite this article as: Pérez-Cuevas R, Jasso Gutiérrez L, Doubova S, Flores Hernández S, Mantilla Trollé C, González Guerra E, et al. Evaluación de la calidad de la atención de la taquipnea transitoria en recién nacidos afiliados al Seguro Médico Siglo XXI. Bol Med Hosp Infant Mex. 2014;71:339-345
* Corresponding author.
E-mail: rperez@iadb.org (R. Pérez-Cuevas).