1. Summary of the clinical history (A-11-08)
This is the case of an 11-year-old male patient with jaundice, drowsiness and vomiting.
1.1. Family history
The mother is 28 years of age and did not complete primary education. She is a housewife, Catholic and healthy. Father is a 31-year-old peasant with incomplete primary schooling.
1.2. Past history
The family is originally from and reside in the state of Hidalgo in a rural environment. They speak Nahuatl language and are from a low socioeconomic status. They cook with firewood, coexist with poultry, and the home is without electricity, drinking water or sewerage system.
Nutrition. The patient was breastfed until 1 year of age and later integrated into the family diet based on corn tortillas and beans. Denied eating wild mushrooms.
Psychomotor development. The patient walked at 18 months, had sphincter control at 24 months, and repeated the second grade in school.
Immunizations. Incomplete, lacked influenza and hepatitis B vaccines.
1.3. Perinatal and medical history
The patient was the product of a GIII. The mother received prenatal care from the fifth month of gestation. There were no complications during pregnancy. She did not consume folic acid or iron. Labor was without complications and the mother was cared for in the rural medical center. The infant cried and breathed at birth; weight, height and Apgar score are unknown. Denied allergies, surgeries, trauma, transfusions or prior hospitalizations.
1.4. Current problem
From January 1 to February 4, 2011 the patient was hospitalized in a second-level hospital due to sudden onset of icterus, which was progressive, cephalocaudal, generalized, accompanied by dark urine and acholia of 1 month duration. During the previous 5 days he also had abdominal pain, vomiting, hematemesis and inversion of the sleep-wake cycle. Papilledema was noted in the fundus of the eye and hepatomegaly of 4-3-3 cm below the costal margin. Ultrasonography of the abdomen showed homogeneous parenchyma, generalized decreased echogenicity, and regular and defined margins. Bile ducts were dilated. Suprahepatic vascular and portal images were normal. He was managed with base solutions at 1,000 ml/m2 sc /day, 4-5 μg/kg/min, dobutamine, dopamine 10 μg/kg/min, cefotaxime 100 mg/kg/day, omeprazole 1 mg/kg/day, vitamin K 10 mg/24 h, lactulose enemas, fresh frozen plasma 10 ml/kg/dose, furosemide 0.5 mg/kg/dose. On physical examination he presented the data described in Table 1. Blood count was done (Table 2).
The male patient was well hydrated with generalized icterus. He was normocephalic and with equal, round and reactive pupils. Nose and ears were without changes. Pharynx showed signs of bleeding and neck was without adenomegaly. Heart and lungs were without compromise. Abdomen was soft and depressible. There was decreased peristalsis. Liver was at 5-3-3 cm of the costal margin. Extremities were without adequate muscle tone and without abnormal movements. Neurological exam revealed somnolence and disorientation. Cranial nerves were without alterations.
February 4, 2011 (intensive care). Endotracheal intubation was carried out due to neurological deterioration. A central venous line and arterial line were placed. Patient was classified as NPO, with saline solution at base 1200 ml/m2 sc/day, glucose 4 g/kg/min, sodium and potassium 30 mEq/m2 sc/day, calcium 100 mg/kg/day, magnesium 50 mg/kg/day, metamizole 10 mg/kg/dose, omeprazole 1 mg/kg/day, vitamin K 0.3 mg/kg/dose, mannitol 0.5 g/kg/c/6 h, norepinephrine 0.1 μg/min, and fresh frozen plasma 10 mL/kg/dose (Table 2).
• CAT of the brain: decrease in the subarachnoid space, irregular differentiation of the gray matter, convexity of cisterns decreased in size, base of cistern without evidence of cystic lesion or hemorrhage.
• Abdominal ultrasound: normal-size and placement of liver, decreased echogenicity without evidence of focal or diffuse lesions. No dilation of the bile duct or intraor extrahepatic vasculature. Scant free fluid in the subhepatic space
• EEG: theta and beta activity, moderate to severe generalized dysfunction
• Chest x-ray: bilateral interstitial infiltrate with homogeneous right apical image.
• Fundus of the eye: demonstrated macular area without cherry red spot, vascular emergence and retina were without alterations.
Management consisted of plasmapheresis and enteral feeding was begun with initiation formula. Cefotaxime (150 mg/kg/day) and dicloxacillin (100 mg/kg/day) were administered.
February 5, 2011. Lactate at 3.7 mEq/l. Transplant team did not consider the patient to be a liver transplant candidate due to the high mortality risk. The patient required boluses of crystalloid solutions, norepinephrine (1.3 mg/min), and hydrocortisone (180 mg/kg/h). Dysglycemia was reported.
February 6, 2011. PT 42.8”, PTT without clotting, fibrinogen (108 mg/dl) and ammonia (197 μmol/l). He was transfused with fresh frozen plasma and cryoprecipitates and was maintained NPO.
February 7, 2011. Serum sodium 153 mEq/l, urine sodium 7 mEq/l, ammonia 230 mmol/l, urine osmolality 195 mOsm.
February 8, 2011. Rostrocaudal deterioration at the diencephalic level, anisocoria, pupils areflexic, no response to painful stimuli.
• CAT of the skull: absence of the subarachnoid space and perimensencephalic cisterns, base cisterns very diminished, mild ventricular collapse, alteration in the relationship of the gray and white matter, probable right uncal hernia. Management for cerebral edema continued (mannitol), fresh frozen plasma.
February 9, 2011. Continued with anisocoria without response to stimuli. Na 151 mEq/l, hypotensive. Neurosurgery clinic did not consider decompressive management for the patient’s condition. He progressed without respiratory effort, no corneal reflexes, cough, gag, or osteotendinous response to nociceptive stimuli. Neurology suggested stopping sedative analgesia for brain death studies.
February 10, 2011. Fever, completed 6 days of cefotaxime and dicloxacillin. Antibiotics were changed to cefepime (150 mg/kg/day) and amikacin (15 mg/kg/day).
• EEG: Low voltage delta activity and minimal reactivity.
February 11, 2011. Without automatic respirations, without response to painful, verbal or light stimuli, hypothermia, without fecal output. Mannitol was suspended, conservative management.
February 12, 2011. Brain death determined with apnea test (pH up to 7.19 and CO2 >40 mmHg, negative atropine test, absent reflexes.
February 13, 2011. Hypotension and cardiac arrest.
2. Case presentation
2.1. Coordinator (Dr. Víctor Olivar López)
A case, not uncommon in our hospital, will be reviewed because we are a patient referral hospital for patients with liver conditions. This issue will be reviewed because care of a critically ill patient challenges a system that should be multidisciplinary.
2.2. Imaging (Dra. María Teresa Valadez Reyes)
Ultrasound from February 4 is shown. The images show diffuse diminished echogenicity. There are no focal lesions. The vena cava, hepatic veins and portal veins are seen. Above it is the hepatic artery with turbulence in its interior. The appearance of the hepatic artery has an index of elevated resistance of 0.80; the portal vein has a hepatopetal flow with an inferior portion below the baseline or one line, which translates to a leak flow with a velocity of 13, slow for the age of the patient. Another image presents decrease of the echogenicity of the liver with portal veins with shine with a “starry sky” image. Spleen was not increased in dimensions. There is also scant free fluid in the cavity. The final diagnosis of this study was diffuse liver damage of yet-undetermined etiology, with incipient data of portal hypertension without focal lesions. USG performed at another hospital reports an intrahepatic bile duct dilatation. USG images take in our institution did not corroborate this diagnosis.
On February 8, CT of the skull in simple phase was done. Notable was the discrete collapse of the ventricular system, predominantly in the left anterior horn. The subarachnoid space was found to be diminished in relationship with the cerebral edema. Poor differentiation was seen of the gray and white substances. No hemorrhagic or infarct zones were found. The predominance of the meninges called the attention because of the decrease in the density of the brain in relation to the cerebral edema. Diagnosis is cerebral edema.
On days 11 and 12, two plain x-rays were taken: one thoracoabdominal that showed small lungs due to abdominal distention and ground glass image in relation with the free fluid in the abdominal cavity. No other lesion was observed. Decrease in bone density of the humerus was notable, which could be related to osteopenia, although it is the study of choice for diagnosis. On the image of February 12, cardiophrenic and costodiaphragmatic angles were not observed bilaterally. There is also bilateral ground glass image on the chest x-ray. There would appear to be increase of the left cavities, but due to the critical condition of the patient, it may be growth. There is no infiltrate and there is no other lesion. The tracheal cannula is in good position. The inferior vena cava catheter remains in good position. With these images, diagnosis of bilateral pleural effusion was made.
3. Discussion (Dra. Berenice Lira de León)
This is the case of a 9-year-old eutrophic child from a family with low socioeconomic status. The patient speaks the Nahuatl language, which constituted a sociocultural barrier making communication with physicians and family members difficult. He had no hepatitis B vaccine or influenza vaccine. Syndromatic diagnoses are as follows:
• Subacute hepatic insufficiency: based on icterus, increase in bilirubin and transaminases, coagulopathy that was not corrected after administration of vitamin K, with >4 weeks of evolution.
• Hepatic encephalopathy: based on somnolence, hyperammonemia and deterioration on status of alertness.
• Intracranial hypertension: based on vomiting, Glasgow deterioration, severe cerebral edema and papilledema.
• Infectious syndrome: based on fever, tachycardia, hypotension and bandemia.
In accordance with these syndromatic diagnoses and the child’s evolution, the following nosological diagnoses were integrated:
• Subacute hepatitis: based on the syndromes of insufficiency and hepatic encephalopathy.
• Nosocomial pneumonia: based on the infectious syndrome and bilateral interstitial infiltrate with right apical homogeneous image on chest x-ray.
• Septic shock: based on data of systemic inflammatory response, pulmonary infectious process, hemodynamic dysfunction and arterial hypotension.
The diagnostic approach and the principal differential diagnoses, treatment and complications that led to the patient’s death are discussed below. Hepatic insufficiency is a multiple organ disease of different etiologies characterized by sudden and severe liver damage. It is associated with high morbidity and mortality. According to the O’Grady classification the patient had subacute hepatic insufficiency with >4 weeks evolution, which has the worst prognosis.1
With respect to the origin of the hepatic insufficiency, in ∼40-50% of the cases its etiology is not able to be established. The most common known cause is hepatitis A followed by acetaminophen poisoning, hepatitis B and C infection, mushroom poisoning, autoimmune hepatitis and Wilson’s disease.2-5 However, the patient had negative serologies for hepatitis A as well as for hepatitis B and C and for cytomegalovirus and Epstein Barr virus (Table 2).
There is no report of prior ingestion or administration of acetaminophen and serum acetaminophen levels are not compatible with poisoning. There was also no history of mushroom ingestion or of hyperacute hepatic insufficiency, characteristic of this poisoning.
Autoimmune hepatitis is another cause for acute liver insufficiency, although not common. Generally it is accompanied by hypergammaglobulinemia, which was present in this patient, although the determination of positive antibodies was unavailable for this patient (smooth muscle or anti-LKM). In children>3 years, Wilson’s disease may present as subacute hepatitis; however, copper and ceruloplasmin determinations were not done.6 The patient was referred from a second-level care hospital with data for hepatic encephalopathy and probable cerebral edema. It is believed that the referral to a third-level care hospital was delayed, which increased morbidity and mortality.
Hyperammonemia (165 mmol/l) contributed to the development of hepatic encephalopathy for which he received lactulose. However, its usefulness has not been demonstrated in the management of hyperammonemia in patients with subacute hepatic insufficiency. Ammonia levels >124 mmol/l have been correlated with altered state of consciousness, intracranial hypertension and convulsions and even predictors of developing complications such as acute renal insufficiency and need for mechanical ventilation.
According to the American Society for Apheresis, treatment of liver failure also considers the use of plasma exchange, which the patient had done two times. It did not improve the coagulopathy. Use of extracorporeal system of treatment known as MARS (molecular absorbent recycling system) was indicated. This is a method of extracorporeal hemodiafiltration that uses an albumin-rich dialysate as action mechanisms for absorption, dialysis and ultrafiltration to facilitate the elimination of toxins attached to proteins. However, both the plasma exchange as well as the MARS therapy are only indicated as a bridge for a transplant as they do not improve survival, although in a small percentage of cases liver regeneration is described during these support therapies.7,8
Hepatic encephalopathy secondar y to cerebral edema is generally of sudden onset and almost always presents itself after the start of icterus. The degree of encephalopathy correlates with the percent of survival. Patients with grade III-IV encephalopathy have a survival rate <20%, as with this patient who presented neurological deterioration with decrease in Glasgow scale and need for invasive ventilation.
General measures for treating cerebral edema should include decrease in stimuli, semi-Fowler at 30° to improve jugular venous drainage and prevent hypotension, hypoxia and hypercapnia, maintain cerebral perfusion pressure of 60 mmHg, normothermia and normoglycemia.9,10 Hyperosmolar therapy such as the mannitol given to this patient was used for the management of edema.
According to the King’s College criteria to determine the need for transplant in hepatic insufficiency, the patient had a history of icterus for>7 days before the beginning of the encephalopathy as well as having an age<10 years and total bilirubin >17 mg/dl. The concurrence of these three criteria is an indication for liver transplant. However, it was not done because the patient had hemodynamic instability and septic shock, which are contraindications for liver transplant.
The prognosis for liver failure is somber, with a mortality of up to 80% in some series. The factors for poor prognosis in the patient included the unknown etiology, age<10 years, grade III-IV encephalopathy, subacute presentation, maximum bilirubin >13 mg/dl and leukocytosis.11
Infectious complications and cerebral edema are the main causes of death in subacute liver failure; 80% of patients develop bacterial infections and 20-30% develop fungal infections secondary to altered function of neutrophils and Kupffer cells, hypocomplementemia, alterations in opsonization and bacterial translocation. Antibiotic therapy with cefotaxime and dicloxacillin was started on this patient due to pulmonary foci. However, despite presenting hemodynamic deterioration and septic shock refractory to amines, there was a delay in change of antimicrobials for coverage of nosocomial infections, which is considered to have contributed to his poor evolution.12
The patient presented anisocoria. A new tomographic study was done and showed severe cerebral edema and probable herniated right uncus. Placement of a peripherally inserted central catheter (PICC) and decompressive craniectomy were indicated, but the patient was not considered as a surgical candidate because of coagulopathy and amine-refractory septic shock.13-16
Atropine test was done for probable brain death without response, as well as positive apnea test. Within the criteria of the General Health Law, article 344, for the diagnosis of brain death, the patient had absence of automatic respirations, permanent and irreversible loss of consciousness and response to sensory stimuli, and irreversible damage to the brain stem. Only confirmation through an imaging study was missing (angiography without cerebral circulation and EEG without electrical activity).13,14 The patient died 9 days after his admission.
Final diagnoses
• Hepatitis (unspecified etiology)
• Subacute liver failure
• Hepatic encephalopathy
• Cerebral edema
• Intracranial hypertension
• Community-associated pneumonia
• Septic shock
• Multiple organ failure
• Probable brain death
Immediate cause of death
• Uncal hernia
3.1. Training and development professor (Dr. Aarón Pacheco Ríos)
It has been mentioned that the serology for hepatitis was negative; however, serology interpretation is incorrect because IgG was positive for hepatitis. This indicates that the patient had a past infection, which at present was resolved. For hepatitis B, there are surface-specific antigens, antibodies against the positive surface specific antigens and antibodies against the core negatives. Although the clinical history mentions that he did not have hepatitis B vaccine, the serological profile of this patient is that of a child who received the vaccine against hepatitis B. One should be more careful with serological interpretations.
4. Pathology (Dr. Guillermo Ramón García)
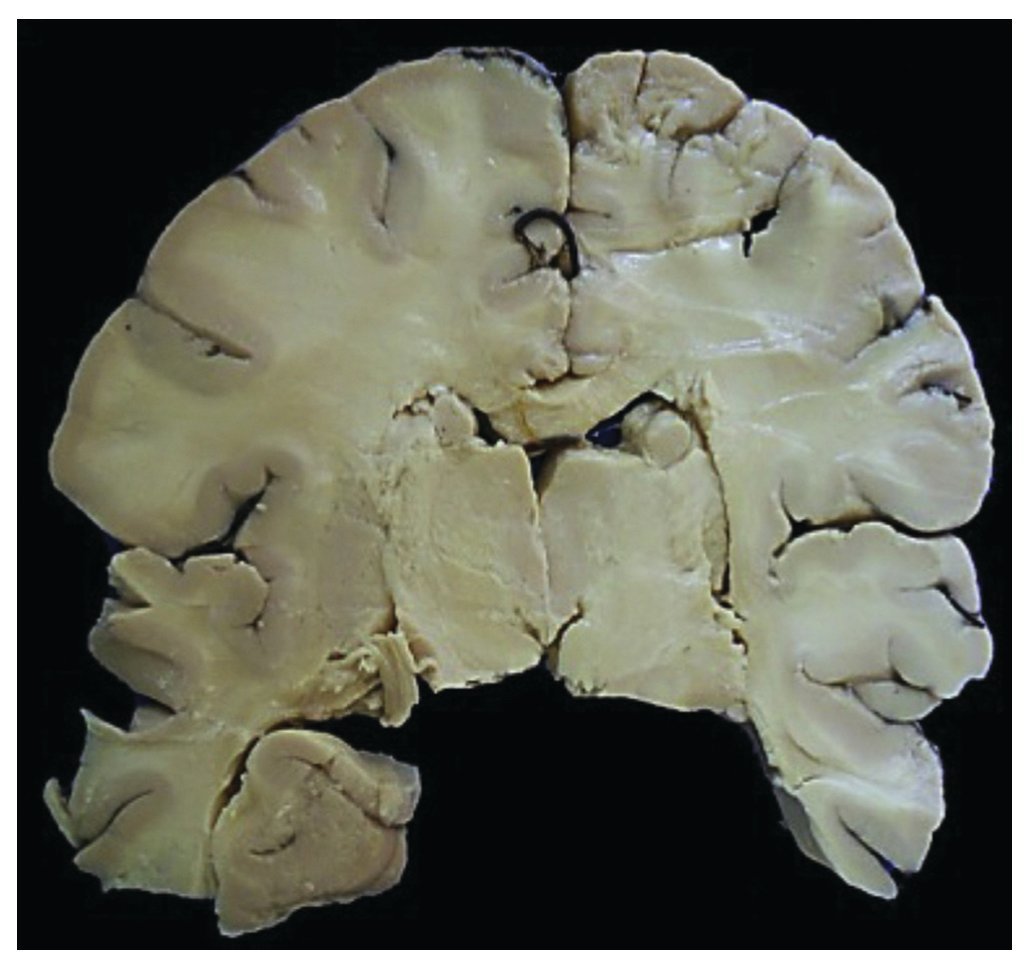
In the outward appearance, jaundice and generalized edema drew attention. The abdomen was distended and, upon opening of cavities, 500 ml of acetic fluid was seen. The liver was slightly retracted, weighed 720 g vs. 760 g and demonstrated congestive splenomegaly (300 g vs. 73 g). The liver showed softening but, on sectioning, large areas of necrosis were observed in 70% of the parenchyma (Fig. 1) that was confirmed microscopically (Fig. 2). The images show the collapse of the parenchyma with the disappearance of hepatocytes in the lobules with only the bile canaliculi and portal spaces visible. Electron microscopy studies were done and determination of copper in the liver tissue, but no evidence of viral inclusions, storage disease or data compatible with Wilson’s disease were found.
Figure 1 Macroscopic aspect of the liver that shows cholestasis and extensive necrotic zones.
Figure 2 A) Panoramic view that shows extensive necrosis of the parenchyma and hemorrhagic zones (HE 10x). B) Approach where extensive necrosis of hepatocytes is observed with collapse of the lobules; only preserved canaliculi and bile ducts are preserved (HE 40x).
For the remaining organs, the findings were as follows: the spleen with congestion of the red pulp and hyper plasia of the white pulp. Lymph nodes also showed hyperplasia of the germinal centers and of the sinuses with erythrophagocytosis. There was also granulocytic hyperplasia and erythrophagocytosis in the bone marrow. In the kidneys there was necrosis of the tubular epithelium seen with hyaline, epithelial and biliary cylinders. In the gastrointestinal tract there was hemorrhage of the esophageal mucosa, stomach and intestines with superficial ulcers. There was also hyperplasia of the lymphoid tissue associated with the mucosa and contraction bands of the muscular wall. In the lungs, zones of atelectasis and congestion with focal hemorrhage were seen. In the central nervous system there was diffuse edema, necrosis in the white substance in the stem with calcifications on the walls of the vessels and necrosis of the cerebellar cortex (Fig. 3). The pituitary gland also showed extensive necrosis (Fig. 4).
Figure 3 Coronal section of brain where marked edema and generalized pallor are observed.
Figure 4 Microscopic appearance of basal nuclei where individual neuronal necrosis and marked edema of the neuropil are identified (HE 25x).
Final diagnoses were as follows:
Principal diagnosis
• Acute hepatitis with submassive necrosis of undetermined etiology
Concomitant diagnoses
• Submassive necrosis (720 g vs. 760 g)
• Generalized icterus
• Ascitis (500 ml)
• Splenomegaly (PO 300 g vs. 73 g)
• Hydrocele
• Cardiomegaly(325 g vs. 115 g)
• Accentuated cerebral edema with secondary leukomalacia
• Individual neuronal necrosis in cerebral hemispheres and cerebellum
• Necrosis of the pituitary gland
Other conditions secondary to shock
• Acute ulcerated laryngitis
• Acute hemorrhagic esophagitis
• Acute ischemic enteritis
• Ischemic-hypoxic visceral myopathy
• Generalized hyperplasia of the lymphoid tissue with mild hemophagocytosis
Cause of death
• Cerebral edema
The list of toxic substances is enormous. In order to determine any likely toxic substance, the liver tissue where there is no necrosis would have to be analyzed. There was no evidence of any metabolic disease or metal deposits found according to the electron microscopy performed. No substance was able to be determined because the necrosis did not allow for such an analysis to be performed. The lesion process was very advanced and mitochondria were broken. For the determination of any element, a chemical analysis would be of more assistance.
5. Final comments
5.1. Emergencies (Dr. Víctor Olivar López)
There are many aspects with regard to the care of a patient with fulminant hepatitis. The difference is in the details taken in the care of a problem such as the reversibility of the encephalopathy to 100%, i.e., if it recovers, improvement of the neurological problem is evident. Therein lies the importance of caring for this patient for what comes first: improvement, transplantation or death. For this, the details involved in the care are what should be guarded.
5.2. Emergencies (Dr. Carlos Bañuelos Ortiz)
Taking into consideration that the patient had serum sodium levels of 157 mEq/l, it is obvious that sodium management was not adequate. Patients with acute liver failure initially require an adequate amount of fluids and electrolytes as baseline requirements as well as to cover losses with vomiting, diarrhea, loss of appetite, and losses due to fever. There is a systemic inflammatory response with vasodilation, increase in the vascular capillary permeability and loss of fluid to the third space. These losses need to be replaced, especially in the presence of poor perfusion, and rapid volume boluses should be given. As the patient progresses, fluids should be adjusted, possibly reducing them because these patients have activation of the renin-angiotensin-aldosterone system with retention of sodium and water. From the beginning there was evidence that the patient had low urinary sodium levels and elevated urinary potassium. This indicates activation of the rennin-angiotensin-aldosterone system; therefore, the sodium content in the patient should be examined. The excess sodium presented by the patient could only come from two sources: excess contribution by the fluids calculated and by the repetitive blood products or increase in the loss of free water. The problem was that mannitol was used for >8 days. It has been shown that the continuous use of mannitol for >48 h produces leak to the intravascular space of the tissues and “pulls” water from the intravascular to the interstitial spaces as well as renal losses caused by mannitol. By not addressing this situation, hypernatremia was produced. On the other hand, one cannot rule out that the patient may have had diabetes insipidus according to the low urinary sodium and osmolarity. The problem was that the fluid balances or uresis of the patient was not available in order to determine the causes.
5.3. Intensive therapy (Dra. Lourdes Marroquín Yáñez)
When the patient already has cerebral edema, which leads to endocranial hypertension secondary to liver failure, management becomes complex and difficult, especially electrolytic balance. It is important to remember that cerebral edema is founded on two theories: the first, in relation to ammonia and glutamine; the second, in relation to the loss of cerebral autoregulation due to the release of pro-inflammatory substances, obviously secondary to liver failure. This leads to a disruption of the hematoencephalic barrier. For a patient with cerebral edema and endocranial hypertension, treatment is based on the guidelines for treatment of a patient with cranioencephalic trauma. Patients should have an intracranial pressure measuring device placed; however, it is here where the controversy begins for the management of patients with intracranial hypertension. It is known that 10-20% may present brain hemorrhages as complications, which increases the already established intracranial hypertension. There are large liver transplant centers that handle intracranial hypertension blindly; others do place intracranial hypertension devices and report low complications with improvement in survival and prognosis in these patients. Therefore, there are two options: blind management or with a device with which the treatment objectives can be laid out. Osmotic therapy has as an objective the use of mannitol or hyperosmolar solutions with hypertonic sodium at 3 or 5% to produce a higher serum sodium level and decrease intracranial pressure, increasing osmolarity. However, it is important to look for adverse effects. The superiority between these solutions has not been demonstrated and there is no evidence of such. What is important is to look for secondary effects. Mannitol should not be used for>48 h. In fact, during the first dose one should look for effects of reduction in intracranial pressure and for the following doses the effects already mentioned. Therefore, management of the patient with mannitol for>3 days probably precipitated renal failure, although it is unknown how the volemia was managed.
For management of these patients, an objective, which is liver transplantation in the short term, should be considered. In transplant centers it is done at 5 days of having initiated treatment for hypertension. Treatment is osmolar therapy, either of the two is similar but one must look for adverse effects: no more than 72 h for mannitol so that events of hypovolemia are not precipitated. Alternative therapies should be evaluated if a transplant is not to be done.
5.4. Neurosurgery (Dr. Vicente González)
In regard to placement of a sensor for the PICC, the indication is grade 3 or 4 hepatic encephalopathy. There are recommendations of benefit with this monitoring for a dynamic management. One is faced with a patient who presents alterations in coagulation time with an INR of 3 or 6, which is partially reversible. There are publications that report that the administration of factor VII produces corrections for 30 min. This is an alternative. Therefore, the recommendation would be to place a sensor with times corrected with factor VII in patients with severe encephalopathy, such as in this case. Although our participation is to co-assist as part of multidisciplinary management, in the management established by intensive care, the problem is that we do not have factor VII nor do we have sensors for intracranial pressure.
5.5. Intensive therapy (Dr. Adrián Chávez López)
It must be kept in mind that there is no effective therapy for fulminant liver failure except for a liver transplant. Therefore, the role of the pediatrician is to maintain the patient in good condition in order to reach a liver transplant center. When the child is awaiting a transplant and if the cumulative fluid balance is>20 ml/kg, which generally occurs on the first day, hemofiltration is indicated, which will help but will not save a life. MARS is indicated from the time the patient arrives and will allow time for the transplant. In the centers where it is used, the mortality rate has not decreased but it does prolong the wait time for transplantation. Finally, the excessive number of transfusions and blood products can also be avoided: red blood cells, plasma and platelets, which are harmful to the child. None of these treatments decrease mortality and the patient is not improved if red blood cells are transfused, but it does increase the risk of nosocomial infection and the risk of pulmonary lesion associated with transfusion. It is worthwhile to make this clear because it has been accepted as a formula for seriously ill and unstable patients who are immediately transfused red blood cells or if the PT is prolonged they are transfused plasma, which does not help them.
Finally, plasmapheresis is indicated, as in this case, to correct the coagulation without volume overload of the patient. Volume overload does condition greater morbidity and mortality. Unfortunately, simple plasmapheresis was done in which a series of filters was not used that serve to clean the internal medium of the child from harmful molecules such as ammonia. It must be emphasized that these procedures do not save the life of the child. Finally, it should be mentioned that the patient became infected and this is avoidable as nosocomial infections increase the risk of death. In fact, in large centers mortality continues to be>60-70%; however, if a nosocomial infection is added, the probability of the child surviving is practically nil.
5.6. Emergencies (Dr. Víctor Olivar López)
Management is not easy and should be multidisciplinary. This is an example of a problem that challenges our system: the patient who has a liver problem hemodynamically behaves like a patient who has a vasoplegia. Due to release of nitrous oxide, the patient required dobutamine. The infectious appearance is precisely what was being manifested by the hemodynamic disorder of the individual; therefore, all symptoms presented by the patient should be taken into account.
5.7. Neurosurgery (Dr. Gordillo)
Monitoring of intracranial pressure depends on the equipment used. There are different ways of doing this. The standard sensor is intraventricular; however, in light of cerebral edema as severe as the one experienced by the patient, its placement is very difficult. In these cases, those placed in the intraparenchymatous tissue function in the best manner. This does not mean that the subdural sensors that are commonly placed do not work; however, they need to be purged continuously with solution to leave a space that allows for them to work in relation with osmotic pressure. The problem, in this case, was the generalized edema. Risk of hemorrhage was imminent when a subdural sensor was placed.
5.8. Emergencies (Dr. Víctor Olivar López)
When there is evidence of acetaminophen or paracetamol poisoning, specific management is indicated. However, currently N-acetyl-cysteine has been indicated to help these patients.
5.9. Emergencies (Dra. Olga Martínez Pantaleón)
From 2005 to date, use of N-acetyl-cysteine has been documented in patients with acute liver failure, such as the case we are discussing, even when there is no evidence of acetaminophen poisoning. In transplant centers such as King’s College in England, a series has been reported on 111 children who came to the center with acute liver failure from 1995. N-acetyl-cysteine was added to the supportive treatment and compared with the group prior to 1995 where this drug was not used. Higher survival was found in the first group, even without liver transplant. In the group in which this drug was not used, mortality was 25% but decreased to 19% in the group of 111 patients in which N-acetyl-cysteine was used.17 Justification for the use of this antioxidant medication was based not only on the production of hepatic glutathione, which is the mechanism it produces in patients with acetaminophen poisoning, but were given various characteristics such as improving local circulation to the liver, improve the local delivery and consumption of oxygen as well as to decrease the systemic inflammatory response that has repercussions in the macrophages and neutrophils. These are features noted to favor the patient. Throughout time greater evidence has been found for its use while waiting for transplant to be done. It has been used in continuous intravenous infusion until the patient shows improvement with an INR of at least 1.4, until the transplant is carried out, or the death of the patient. From recent reports, the FDA has authorized it as treatment of Amanita phalloides and Amanita virosa mushroom poisoning, which are hepatotoxic. In the hospital it has been used in two patients who were admitted to the intensive care unit. This type of treatment was successful. More cases need to be evaluated and reconsidered by the intensive care team of transplants and toxicology. New possibilities are being seen. The etiology is very varied from that of the previously mentioned group.
5.10. Emergencies (Dr. Víctor Olivar López)
Uncertainty remains about the approach or thinking of the transplant services. Initially, the possibility of reversibility of the problem was addressed, but later on it was discussed that the patient was gravely ill, making transplantation impossible. There are clinical and ethical aspects that warrant comment from the transplant service.
5.11. Pediatric surgery (Dr. Rubén Figeroa Portillo, 7th year resident)
Reversibility was expected because one of the two coagulation factors was within normal limits. A study in our hospital included 62 patients with fulminant hepatitis, of whom 20% had reversibility. This percentage was in line with the percentage of activity of coagulation factors V and VII. Of the 62 patients, 20 were waitlisted for liver transplantation and in whom the two coagulation factors were not frankly altered. From this group, ten patients were transplanted with a survival of 80%. Only in 4% of the patients listed did the liver regenerate, even though their factors were below the normal limits. Six patients (30%) died in the following 6 days. Therefore, a percentage of patients have liver reversibility when one of the two factors is above the normal values.
5.12. Emergencies (Dr. Víctor Olivar López)
Another concern is related to the ethical situation. To inform parents that their child will be referred to a center to be integrated into a transplant process is difficult, and it is not easy for the parents to assimilate this situation. What would be the procedures for patients in an acute state? In the patient with a chronic disease, the parents are better prepared. What would be the impact on parents who are suddenly advised that their child should be transplanted because of liver disease?
5.13. Surgery (Dr. Eduardo Bracho Blanchet)
For parents who speak Spanish and are able to communicate with the medical team, it is the worst news to be told that their previously healthy child, over the last 2 or 3 weeks, is dying and needs to be transplanted. With greater reason there were difficulties to translate this information into the Nahuatl language. This will depend much on the sociocultural quality and knowledge of the family; however, it does not cease to be terribly difficult news to assimilate.
5.14. Emergencies (Dr. Víctor Olivar López)
This aspect is very important and the entire panorama must be guarded. There is no evidence in the record about a psychological approach that would complement this condition.
In summary, this was a patient from a rural environment with a disease of multiple etiologies. This was a case of acetaminophen poisoning and of viral processes, but all patients are exposed to a variety of substances that can cause liver failure. Patient transfer should have taken place earlier and under optimal conditions with intubation and critical care, multidisciplinary management. All details should be carefully monitored so that the patient can be prepared for what is hoped—a transplant. Unfortunately, in the case of this patient, the normal evolution of liver failure took place.
Conflict of interest
The authors declare no conflict of interest of any nature.
* Corresponding author.
E-mail:gramon55@hotmail.com (G. Ramón García).
Received 22 July 2014;
accepted 28 July 2014