Two cases of multifocal unilateral acute idiopathic maculopathy are presented, one in a 24 year-old man, and another in a 37 year-old woman. Both of them presented with acute vision loss and clinical findings compatible with unilateral acute idiopathic maculopathy. As a relatively uncommon finding, they had multifocal lesions around a larger central lesion. They experienced a spontaneous improvement of their vision.
Atypical presentations of unilateral acute idiopathic maculopathy like multifocal lesions are possible. Ophthalmologists should be aware of this rare form of presentation.
Presentamos 2 casos de maculopatía idiopática aguda unilateral en 2 adultos jóvenes, un varón de 24 años y una mujer de 37 años. Ambos sufrieron una pérdida aguda de visión acompañada de manifestaciones clínicas compatibles con la maculopatía idiopática unilateral aguda. Como hallazgo excepcional, presentaron lesiones multifocales alrededor de una lesión central de mayor tamaño. Con el tiempo, se produjo la recuperación espontánea de la pérdida visual.
La maculopatía idiopática aguda unilateral puede presentarse de formas distintas de la convencional, por lo que deberíamos considerar la posibilidad de encontrarnos ante estas formas atípicas.
Unilateral acute idiopathic maculopathy (UAIM) was a rare entity described by Yannuzzi et al. in 1991 in a series of 9 patients.1
The clinic debut of UAIM is sudden and painless loss of central vision, associated or not with a pseudo-flu-like condition in previous days. It typically occurs in young healthy adults. Multiple theories have been developed about its possible causes, including the possibility of involvement of viruses from the Coxsackie family.2
The disease involves the choroid, the retinal pigment epithelium (RPE), the outer layers of the retina and the haematoretinal barrier, resulting in a serous neuroepithelium (NE) detachment, associating a yellow-grey fundus image in the injured area.3
Most cases resolve spontaneously within a few weeks, with almost complete recovery of vision, leaving a characteristic porthole-like macular pigment alteration.1,4
Two clinic cases of UAIM are presented, in which the presence of satellite elements around the central lesion in the posterior pole was observed, a finding not described in previous reports.
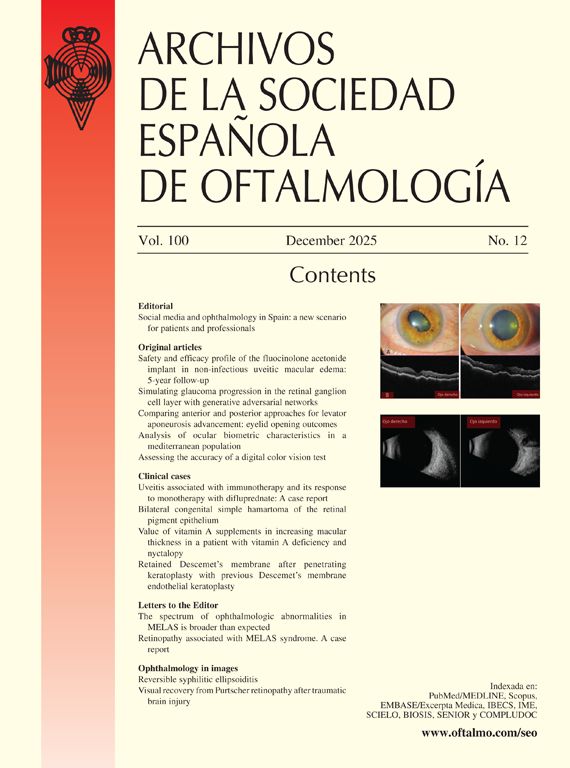
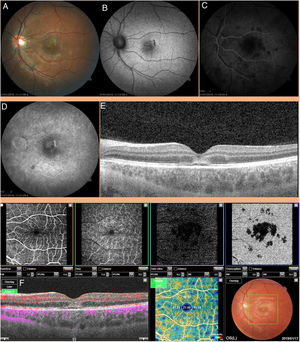
Clinic caseCase 1Healthy 24-year-old male, myopic, 4 diopters, with sole history of circumstantial hypertransaminasemia in the context of feverish clinic, which occurred due to sudden and painless loss of vision in the left eye (LE) after 4 days of evolution. The patient had a visual acuity (VA) of 1.0 in the right eye (RE) and finger counting in the LE. Anterior pole biomicroscopy was normal in both eyes (BE) and intraocular pressure was 15mmHg in BE. Fundus scan in the RE was normal. In the LE a yellow-greyish lesion was observed, rounded and with poorly defined edges, located in the center of the macula. In addition whitish, much fainter, smaller lesions could be observed around the main lesion at the posterior pole. No associated vitritis, vasculitis or papillitis was observed.
A mixed pattern of hyper- and hypo-fluorescence was observed in autofluorescence (AF).
Optical coherence tomography (OCT) (DRI OCT Triton plus, Topcon Medical Systems, Inc., Tokyo, Japan) showed involvement of the external retinal layers, with elevation of the interdigitation zone and increased reflectivity of the layers above, without associated choroidal neovascularization in the angiotomographic image (OCT-A).
In angiofluoresceinography, the lesion showed an early hypofluorescence with the appearance of some hyperfluorescent areas in more advanced stages, especially at the edges of the lesion. Next to the central lesion, other satellite hypofluorescent lesions were observed corresponding to the whitish lesions which could be due to an alteration of choroidal circulation in those areas. These satellite lesions showed a dark pattern in OCT-A, compatible with an choroidal circulation alteration (Fig. 1).
Case 1. (A) White-greyish lesion in central macula. Pale satellite lesions. (B) Mixed pattern in FA. (C) FAG in early times in which the hypofluorescence of the central and satellite lesions can be seen. (D) FAG in more advanced stages with hyperfluorescence at the edges of the lesion. (E) Compromise of external retinal layers, with elevation of the interdigitation zone and increased reflectivity of the layers above. (F) OCT-A. Alteration of choroidal flow in the areas corresponding to the lesions observed in retinography and FAG.
After ruling out central serous choroidopathy, treatment was initiated with 60mg daily of oral prednisone. All analytical, serological and immunological tests were negative, except for blood creatinine 1.1mg/dl, HLA-B51+, herpes simplex virus (HSV) type 1+.
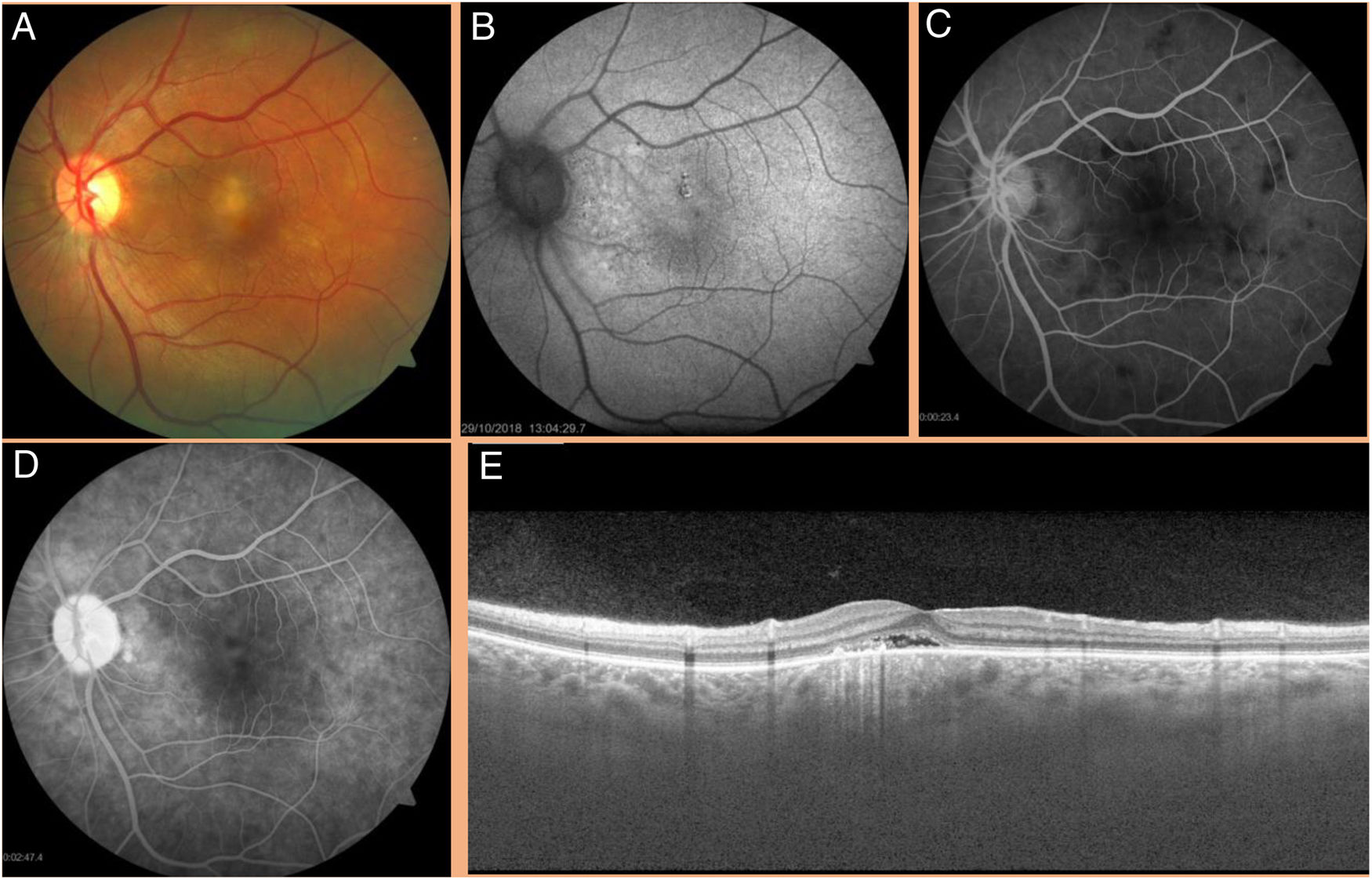
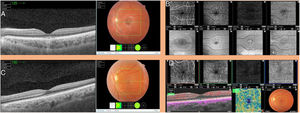
After 6 weeks treatment with steroids in descending pattern, the patient referred mild visual improvement (VA LE 0.16). Focal loss of subfoveal photoreceptors and RPE hypertrophy was documented. At 12 months of follow-up without medication, the LE VA was 0.6. The subfoveal hyperreflective zone above the external bands was not observed in OCT, although focal alterations of the external limiting membrane, ellipsoid and interdigitation layer persisted.
In OCT-A, the dark pattern of the satellite lesions had disappeared, which would indicate a recovery of choroidal circulation (Fig. 2).
Case 1 (A and B) and case 2 (C and D) at the end of the monitoring. (A and B) OCT and OCT-A case 1. Disappearance of the subfoveal hyper-reflective zone. Persistence of focal external bands alterations. OCT-A and in face angio of LE. Almost complete normalization of OCT-A images. The en face mode allows the identification of structural alterations in the external layers of the retina. (C and D) OCT and OCT-A LE case 2. Almost complete normalization of the macula.
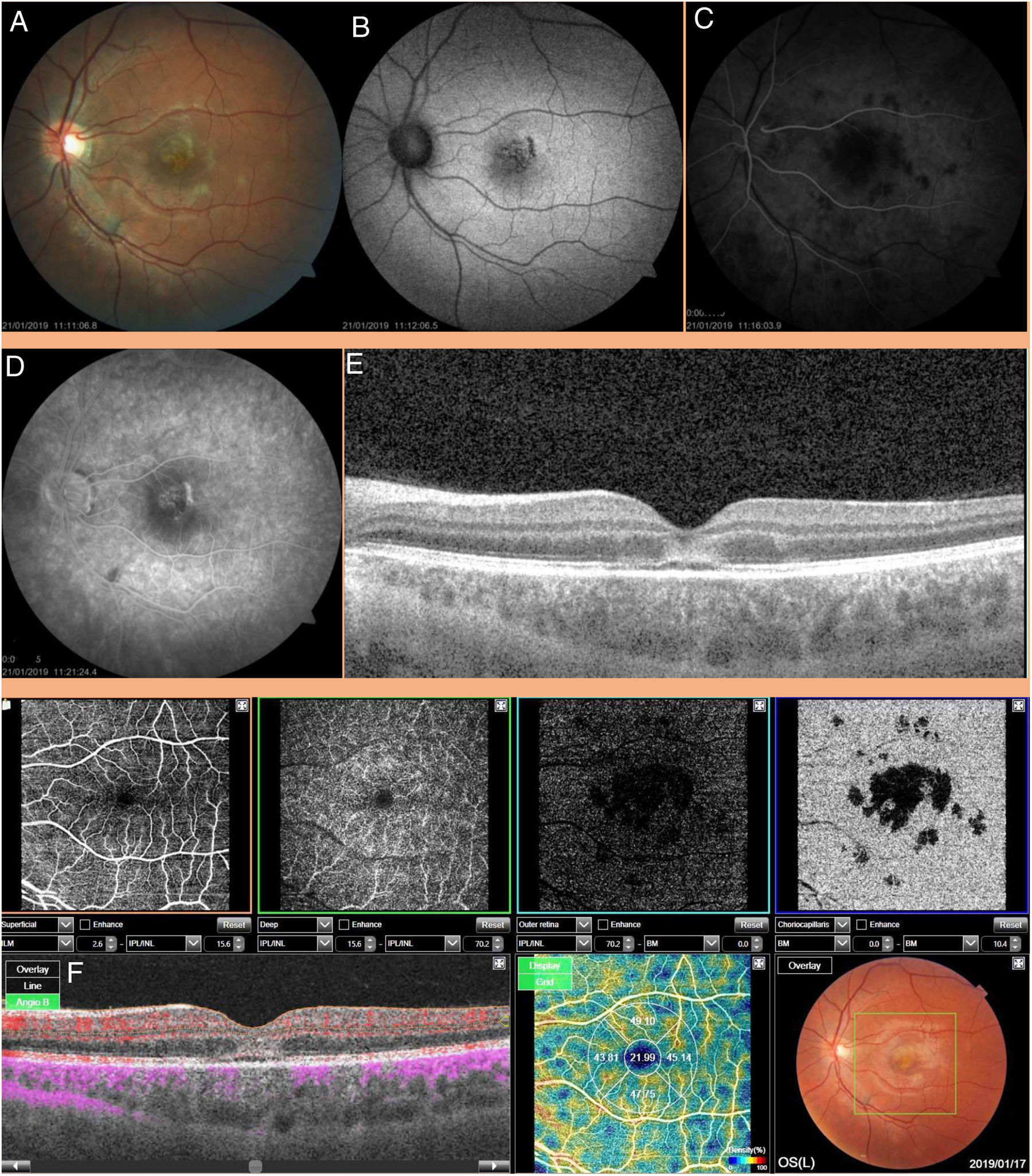
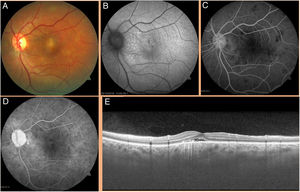
A 37 year-old female with no relevant history visited for diminished VA in the LE with a few days evolution associated with periorbital headache. LE exploration discovered a choroidal nevus temporal to the macula as a casual finding. In the LE a yellow-greyish lesion was observed located in the central macular area surrounded by smaller lesions of the same color in the posterior pole. There were no other inflammatory signs such as vasculitis, papillitis or vitritis. VA was 1.0 in the RE and 0.6 in the LE. In FA the central macula showed a mixed hyper- and hypoautofluorescent pattern.
OCT revealed a subfoveal NE detachment. In FAG, the central lesion showed initial hypofluorescence. In more advanced stages, a slight hyperfluorescence was observed at the edges of the lesion. The satellite lesions showed an initial hypofluorescence with a tendency to disappear along the angiogram (Fig. 3).
Case 2. (A) White-greyish lesion in the central macula with satellite lesions. (B) FA with mixed autofluorescence pattern. (C) Early FAG with hypofluorescent lesions. (D) FAG in more advanced stages. Mild hyperfluorescence in the central area. (E) Detachment of the subfoveal neuroepithelium.
All serological, immunological and analytical tests were normal, except IgG ELISA+ for Epstein–Barr virus (EBV). Oral prednisone treatment was initiated 60mg/day. However, clinic worsening was observed with steroids being discontinued after 1 week.
Without treatment, both clinical and anatomical improvement occurred up to disappearance within a period of 6 weeks, with resolution of the multiple NE detachments and LE VA of 1. After 15 months of follow-up, there have been no recurrences and the situation remains stable (Fig. 2).
DiscussionUAIM appears to be an inflammatory disease involving the external retina and RPE, characterized by an acute loss of central vision, preceded by a viral prodrome. Although the exact etiology is unknown, there are numerous studies that relate it to Coxsackie virus.3–5 Prognosis was usually good, with spontaneous recovery occurring in weeks or months.6
The initial work of Yannuzzi et al.,1 based on possible viral etiology, referred to possible bilateral, multifocal and even recurrent forms of the disease. In accordance with this assessment, 2 cases of UAIM with multiple satellite lesions around a larger central foveal lesion are presented. This multifocal form had been described in only one paper published in 1998.7 Therefore, UAIM could include characteristics not described in the initial work of Yannuzzi et al.1
As mentioned above, the disease has been associated with the Coxsackie virus. UAIM could be a consequence of direct infection by the virus or also due to an autoimmune response to the viral infection. Some forms of Coxsackie virus are capable of infecting RPE cells in vitro. The virus would reach these cells during viraemia through haematogenous spread.8
On one occasion, the disease was linked to yellow fever.8
In none of our cases was a Coxsackie virus infection identified. On the other hand, we consider the presence of HSV in the first patient and EBV in the second as a casual phenomenon, given its relatively high frequency in the general population.
Comparing the literature with the findings of our cases, a correspondence in all the mentioned tests and in their evolution along time was evidenced, i.e., white-greyish lesions in posterior pole associated to ND, FA, angiographic characteristics and tomographic alterations. We highlight the alteration in choroidal flow observed in OCT-A and FAG. This choroidal flow alteration has already been suggested based on studies made with OCT-A.9
Some authors, given the spontaneous resolution of the clinic, recommend avoiding the use of steroids based on the direct viral infection theory. Others defend its use when considering possible autoimmune damage. In our cases, the case 1 patient received steroid treatment. Case 2 experienced a worsening of the clinic a week after starting treatment with prednisone, so said treatment was suspended. This poor response to steroids could be related to damage caused by the direct action of the viral infection. In both, the visual and anatomical result was similar and good.6,10 Due to its inhibitory effect on vascular permeability, some have suggested the possibility of using aflibercept as an alternative treatment to the use of steroids.
CSC and Harada disease should be considered in the differential diagnosis. CSC can be ruled out by the behavior of the lesion in FAG (absence of the characteristic diffusion), indocyanine green (ICGA) (choroidal circulation alterations in UAIM, in the form of choroidal vascular involvement, dilatation of choroidal vessels with the presence of moth-eaten-looking vessels). Harada disease was characterized by the presence of multiple serous retina detachments and in FAG multiple hyperfluorescent point lesions are typical. ICGA, on the other hand, would show a patchy hypofluorescent pattern in the posterior pole.
By way of conclusion, the UAIM entity is an ophthalmological disorder associated to Coxsackie virus with good evolution and prognosis. This entity should be taken into account in acute unilateral conditions, with involvement of external retinal layers and choroidal vascular involvement in the macular region, without ruling out some less frequent forms of presentation such as bilateral, multifocal or recurrent.
Conflict of interestThe authors declare the absence of any conflict of interest and deny having received any financial support.
Please cite this article as: Sánchez-Vicente JL, Moruno-Rodríguez A, de las Morenas-Iglesias J, Rueda-Rueda T, Lechón-Caballero B, López-Herrero F. Presentación multifocal en 2 casos de maculopatía unilateral aguda idiopática. Arch Soc Esp Oftalmol. 2020. https://doi.org/10.1016/j.oftal.2020.05.023