The new disease known as COVID-19 has already affected over 260,000 people and caused over 26,000 deaths in our country. In only 3 months, 8000 articles related to COVID-19 have been published, of which about 100 are within the ophthalmological specialty.
Among the multiplicity of symptoms that the COVID-19 disease is able to express, neurological symptoms are beginning to be mentioned in recent publications,1 particularly those related to taste and smell disorders observed in younger patients.2 We have found several papers relating to different cases of ophthalmoparesis in the context of the disease.3,4
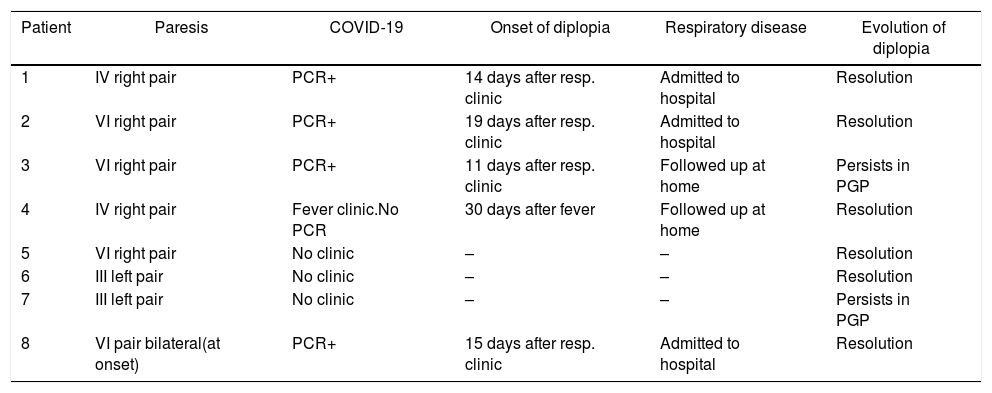
In our experience, last April we have seen 7 cases of isolated oculomotor paresis in our Emergency Dept., 3 of which occurred in the context of the COVID-19 disease (Table 1). Three of these patients tested positive polymerase chain reaction (PCR) for SARS-CoV-2. A fourth patient showed fever clinic compatible with the disease although no PCR was tested. During March and April 2019 we had an average of 3 oculomotor paresis per month, 50% less than those seen in the same period of 2020.
List of patients with diplopia and relationship to COVID-19.
| Patient | Paresis | COVID-19 | Onset of diplopia | Respiratory disease | Evolution of diplopia |
|---|---|---|---|---|---|
| 1 | IV right pair | PCR+ | 14 days after resp. clinic | Admitted to hospital | Resolution |
| 2 | VI right pair | PCR+ | 19 days after resp. clinic | Admitted to hospital | Resolution |
| 3 | VI right pair | PCR+ | 11 days after resp. clinic | Followed up at home | Persists in PGP |
| 4 | IV right pair | Fever clinic.No PCR | 30 days after fever | Followed up at home | Resolution |
| 5 | VI right pair | No clinic | – | – | Resolution |
| 6 | III left pair | No clinic | – | – | Resolution |
| 7 | III left pair | No clinic | – | – | Persists in PGP |
| 8 | VI pair bilateral(at onset) | PCR+ | 15 days after resp. clinic | Admitted to hospital | Resolution |
PCR: polymerase chain reaction; PGP: primary gaze position.
In what concerns compromise of cranial pairs, we have observed 2 paresis of the VI cranial pair and one of the IV pair in the context of COVID-19. These evolved positively, with 2 cases recovering almost completely in the course of the present month. The third case, diagnosed only one week ago, is evolving favorably.
In all of these cases, respiratory symptomatology preceded diplopia clinic by approximately 2 weeks. This timeline matches previously published cases.3,4 Two of our patients had to be admitted to hospital for controlling their respiratory disease while the third was followed up at home. In our review of the literature, oculomotor paresis or neurological syndromes have occurred in patients with moderate-severe disease.3–5
Imaging tests (computerized tomography) did not reveal findings in our patients. Due to current circumstances we do not have other imaging tests such as magnetic resonance that could have shown nerve inflammation in the context of the viral infection.4
In the same hospital, another patient was diagnosed with the Guillain-Barré syndrome, the sensitive and motor axonal of the disimmune acute axonal neuropathy variant (AMSAN) after studies made it with electromyography. Said patient also began showing diplopia clinic 2 weeks after the onset of respiratory clinic (Table 1, case 8). PCR was positive for SARS-CoV-2. The timeline of this clinic case suggests that the virus could be accountable for neurological syndromes that follow a postinfection immune pattern. However, other groups have reported cases for which they proposed a para-infectious or simultaneous infection with the same syndrome.5,6
As pointed out by Gutiérrez-Ortiz et al. it is important to consider that the relationship between ophthalmoparesis and the COVID-19 disease could be coincidental.3 However, just like other respiratory virus, SARS-CoV-2 is able to produce neuroinvasion through the hematogenous or retrograde neuronal pathways.1 This is supported by the evidence of a higher incidence of taste and smell disorders in these patients.2
Other authors suggest that patients in severe condition exhibit hyper-inflammation events that could produce microvascular immunothrombosis events. This mechanism would arise mainly due to the invasion of the virus through receptor 2 of the angiotensin converting enzyme (ACE2) in vascular endothelial cells.7 Even though in our isolated patients afflicted with oculomotor paresis the COVID-19 disease was slight-moderate, this remains as a hypothesis that could match the microvascular etiology of the vasa nervorum.
To summarize, due to the lack of evidence about the cause or causality of these neuro-ophthalmological events in the context of the COVID-19 disease, ophthalmologists can and should contribute to clarify these relationships.
FundingThe authors declare not having received any funding for this paper.
Please cite this article as: Pascual-Prieto J, Narváez-Palazón C, Porta-Etessam J, Gómez-de-Liaño R. Epidemia COVID-19: ¿debe el oftalmólogo estar alerta ante las paresias oculomotoras? Arch Soc Esp Oftalmol. 2020;95:361–362.