Non-alcoholic fatty liver disease (NAFLD) is reaching epidemic proportions worldwide. Collectively, Latin American countries have some of the highest obesity rates in the world and the fastest-growing prevalence of type 2 diabetes mellitus (T2DM). Since obesity and T2DM are intrinsically linked with NAFLD, epidemiological projections are worrisome. In addition to this adverse epidemiological setting, the region of Latin America faces unique challenges and obstacles to addressing the growing burden of NAFLD. In this article, on the occasion of the International NASH Day on June 10, 2021, we describe the main challenges and opportunities to improve care of people living with NAFLD in Latin America. Among the major challenges to be tackled are: lack of disease awareness, limited educational opportunities for healthcare personnel and general public, health system fragmentation, and lack of effective strategies for the prevention and effective treatment of NAFLD and common comorbidities, namely obesity and T2DM. Wide dissemination of current concepts on NAFLD, and extensive collaboration between scientific societies, governments, non-governmental organizations, pharmaceutical industry, and other stakeholders is urgently needed to advance the NAFLD public health policies agenda that allows us to address this disease with a whole of society approach.
Non-alcoholic fatty liver disease (NAFLD) comprises a spectrum of liver lesions ranging from isolated steatosis to non-alcoholic steatohepatitis (NASH), that can lead to serious liver disease, including cirrhosis, cancer and death. NAFLD is considered a “silent” disease because most people with NAFLD are asymptomatic for many years until they develop advanced disease [1]. The condition is associated with substantial morbidity and mortality and is the most rapidly increasing indication for liver transplantation in many countries, resulting in substantial health care costs and economic losses [2,3]. Recently, an international expert panel recommended renaming non-alcoholic fatty liver disease (NAFLD) to metabolic-(dysfunction)associated fatty liver disease (MAFLD) [4], and adopting a set of positive criteria to diagnose the disease that are independent of alcohol intake or other liver diseases [5]. This proposal was recently endorsed by the Latin American Association for the Study of the Liver (ALEH) [6]. The scientific community has broadly reacted with enthusiasm to this change in terminology, although there is still a need for consensus regarding the uniform use of the new acronym. For that reason, we will use NAFLD throughout this article.
The estimated prevalence of NAFLD in Latin America is 31% [7], but estimates for the region are imperfect as primary data from most countries are lacking. Available studies reporting prevalence data from Brazil (35.2%), Chile (23%), Mexico (17%), and Colombia (26.6%) (see Younossi et al. [8] and references therein) were performed more than a decade ago. Rates of NAFLD are likely higher now as this part of the world has witnessed the fastest-growing prevalence of type 2 diabetes mellitus T2DM [9] and has obesity rates that are among the highest in the world [10].
In addition to the high regional rates of obesity and T2DM, proper -NAFLD diagnosis and management is hampered by low disease awareness, extreme social inequalities and fragmented healthcare systems, with poor communication between specialists and between different levels of care. There is also little awareness of the disease among national decision makers, with no action plans to concretely address a rapidly growing health problem. Thus, Latin America faces significant and multilevel challenges regarding NAFLD. In this article, on the occasion of International NASH Day on June 10, 2021, we aim to describe the main challenges and opportunities to improve awareness and patient care of people living with NAFLD in Latin America.
Lack of disease awareness: a serious problem to be tackledDespite being the most common underlying cause of incidental liver test abnormalities and a growing global health problem, NAFLD is mostly under-appreciated by non-liver specialists, including primary care physicians, other specialists, and physicians caring for patients with metabolic disturbances [11]. Several reports from different regions of the world have shown that a significant proportion of physicians have little awareness of NAFLD, underestimate the prevalence and associated-risks of the disease and are not informed about its proper assessment [12–14]. Currently, no such data is available for Latin America. In addition, and importantly, NAFLD awareness is also low among patients, even those with major risk factors for NAFLD, such as overweight or obesity (19% aware of NAFLD), insulin resistance (23%), or both (24%) [15]. Lack of awareness among healthcare professionals results in under-diagnosis as well as in low rates of referral and delayed intervention in patients at risk of liver and metabolic complications [1]. Also, it may lead to under-recording of NAFLD in electronic medical records, affecting resource allocation and epidemiological estimates [16]. Considering that NAFLD is projected to double or even triple by 2030 in many regions of the world and is affecting young people in the region [17], efforts need to be made in order to increase recognition of the disease, its consequences and how it can be prevented and managed.
To address the challenge of increasing awareness about NAFLD, there is a need for education, with a multipronged approach targeting all stakeholders. In the recently published document NAFLD: Sounding the alarm on a global public health challenge [18], prepared by The Economist Intelligence Unit with the support of the European Association for the Study of the Liver (EASL) International Liver Foundation (EILF), several proposals for raising awareness and understanding of NAFLD can be found. Key stakeholders to be targeted include the general public, primary healthcare professionals, relevant non-liver specialists (such as diabetologists and endocrinologists) as well as policy makers.
Proactive efforts to improve awareness among the general public can include information campaigns using educational videos and brochures that can be disseminated through social media or local TV, offering of free liver assessment during dedicated periods of the year, or special events at hospitals or community centers to educate about liver health. Patient education is also key to increase illness perception and thus increase adherence to lifestyle change recommendations [19].
A wide offer of NAFLD education programs is key to providing primary care physicians and non-liver specialists with the knowledge and tools to recognize the disease and assess its severity in order to properly refer patients to specialist care and manage those with mild disease. In addition, promoting a patient-centered NAFLD care by leveraging its links with other diseases may be helpful to address NAFLD issues in a coordinated manner across disciplines [18]. In this regard, conducting collaborative work with obesity, diabetes and cardiovascular disease guideline committees is critical to develop integrated clinical guidelines for NAFLD management.
The NAFLD renaming process [4,5] is also relevant for disease awareness. Some recent data suggest that the acronym MALFD could help in promoting awareness about the condition among non-liver specialists and primary care providers [20,21]. Indeed, the use of simple and easily applicable criteria could help physicians to better recognize and assess the disease. More evidence is needed and work among major scientific liver societies is ongoing regarding this matter.
Finally, policy makers are a key stakeholder group to engage. Hepatology organizations, civil society and patient groups, have a central role in campaigning for awareness and action to address NAFLD. Though the above-mentioned initiatives are challenging tasks, actions to raise awareness about NAFLD in Latin America are urgently needed.
Case finding, risk stratification, and referral pathwaysProper recognition and assessment of NAFLD in the clinic is key to deal with the growing number of patients with the disease. Thus, continuous education on topics such as case finding, risk stratification, and referral pathways should be promoted for all healthcare professionals involved in the management of patients with NAFLD-associated conditions is needed. A short summary of current concepts on these issues is presented below.
NAFLD patients are identified in three scenarios: (1) as an incidental finding in an abdominal ultrasound examination; (2) as part of a diagnostic algorithm for altered liver test results; and (3) when screening for NAFLD in patients with comorbidities associated with metabolic syndrome. The latter approach has not been endorsed by all experts and scientific societies [22,23]. However, screening for NAFLD in at-risk individuals has been endorsed in the recently published ALEH Guidance for NAFLD and by other experts’ groups [1,24]. Due to the increased risk of liver fibrosis among these patients, timely diagnosis is even more crucial. A liver ultrasound is the preferred first-line tool for diagnosis.
Risk stratification of both hepatic and extrahepatic risks is of paramount importance in defining the prognosis of NAFLD patients [25]. Even though liver fibrosis is the main factor associated with NAFLD mortality, only a small proportion of patients will develop significant fibrosis. Thus, the currently preferred algorithm includes easily available and inexpensive tools with high negative predictive value at the first step of evaluation, such as non-invasive and non-patented scores (e.g., NAFLD fibrosis score, FIB-4) [26,27]. When advanced fibrosis cannot be excluded, the second step of assessment includes an elastography technique, with transient elastography the most validated tool. Again, when advanced fibrosis cannot be ruled out, patients should be considered for a liver biopsy. Several shortcomings of this algorithm are still to be solved, such as the ideal cut-off points for non-invasive scores in special populations [28,29], as well as reassessment intervals. Clearly designed and tailored algorithms are needed in Latin America to facilitate the adherence of primary care physicians and to improve the efficient access to more expensive second-line technology, such as elastography [18,30].
Regarding extrahepatic risk assessment, cardiovascular risk assessment using easily available tools such as the Framingham score have been proposed [31], although specific scores for NAFLD patients are yet to be validated.
Effective referral pathways aim to optimize cost-effectiveness by reducing the number of unnecessary specialist care referrals [18]. Since NAFLD is part of a systemic disease, the development of multidisciplinary teams integrated by primary care physicians, liver specialists and specialists involved in the management of other features of the metabolic syndrome could be the key to optimize the management of these patients [1], by conveying clear referral rules adjusted to local context, and to discuss and agree on therapeutic strategies to optimize these patients’ outcomes [18].
Management: The challenge of creating operational integrated multidisciplinary teamsThere is currently no approved therapy for NAFLD. Several drugs are in advanced stages of development. Healthy lifestyle and weight reduction are key in the prevention and treatment of the disease [22]. Cardiovascular disease and malignancy are the leading causes of death in these patients. The management of this disease requires a multidisciplinary panel of caregivers, including primary care practitioners, endocrinologists and hepatologists, among others, taking into account that the nature of the disease crosses different specialties and that the number of patients is so large that all patients cannot be treated by hepatologists alone [32]. Unfortunately, the fragmented healthcare systems that exist in the region, with poor communication between specialists and between different levels of care, do not lend themselves to the creation of multidisciplinary teams of medical and allied health professionals to tackle the multiple NAFLD-associated comorbidities. Also, not all stakeholders have fully realized the fact that to fight NAFLD there should be a coordinated effort of all players in a multidisciplinary approach. Scientific societies, public health authorities, pharmaceutical industry and non-governmental organizations (NGOs) need to work together as a task force triggered by an effective ‘Call to Action’ [18]. Raising awareness of this disease is crucial in order to take actions to control it [33]. Another challenge to tackle is to promote the change of the siloed structures within health systems aiming to achieve integrated care for patients with NAFLD. Some innovative strategies to promote and facilitate integration are building NAFLD care programs on existing structures such as diabetes or cardiovascular clinics, proper training and close work with allied health professionals (i.e., dieticians, exercise specialists, counsellors or clinical psychologists) and creation of programs centered around the patient’s experience [18].
Balance between nutrients and energy is pivotal in the development of NAFLD. Central obesity is an important driver of disease through the promotion of insulin resistance and proinflammatory signaling [32]. Despite the imperative for effective pharmacotherapy, there is no standard-of-care treatment currently available. Several treatment strategies have been evaluated, with different study populations and efficacy endpoints, and thus, with heterogeneous results. Numerous drugs with different mechanisms of action, targeting lipid metabolism, inflammatory, or fibrotic pathways, are currently in development [1]. To achieve full FDA approval, two histological endpoints must be accomplished: NASH resolution without worsening of fibrosis or an improvement in fibrosis of one stage or more without worsening of NASH. The refinement of therapeutic strategies, including thoughtful combination approaches, tailored to the patient’s individual disease drivers, will be needed to increase response rates, which at present time are rather disappointing.
In addition to the implementation of a multidisciplinary approach for NAFLD management, a number of questions are still unsolved: Which patients should be treated beyond the diet and lifestyle approach? Which treatment should we consider for different groups of patients? For how long? How are we going to measure their effectiveness in real life? Indeed, progress being made in precision medicine approaches will help to answer these questions in the near future [34]. In the meantime, we have a real challenge ahead of us. It's time to face it and start working together before it's too late.
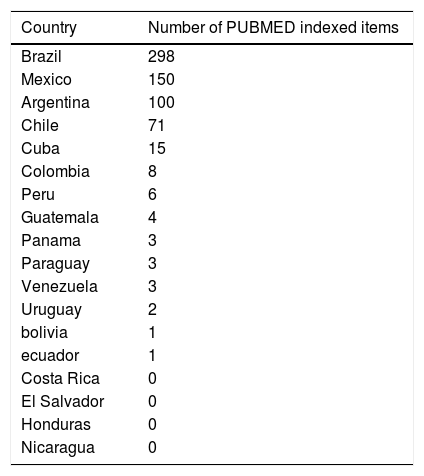
NAFLD research in Latin AmericaNAFLD research faces important challenges in Latin American countries [7]. In spite of being one of the regions with the highest NAFLD prevalence, research output remains low, which is reflected by low publication rates in scientific journals. A PubMed search examining publications generated in the last decade shows that most of the 18 countries analyzed exhibit a very low scientific productivity related to all aspects of NAFLD (Table 1). Thus, information about important NAFLD-related issues in the region is scarce or limited including data on epidemiology and genetic background, socioeconomic conditions, lifestyles, diets and cultural traditions and how these factors impact the disease.
NAFLD related publications listing Latin-American authors 2010-2021.
| Country | Number of PUBMED indexed items |
|---|---|
| Brazil | 298 |
| Mexico | 150 |
| Argentina | 100 |
| Chile | 71 |
| Cuba | 15 |
| Colombia | 8 |
| Peru | 6 |
| Guatemala | 4 |
| Panama | 3 |
| Paraguay | 3 |
| Venezuela | 3 |
| Uruguay | 2 |
| bolivia | 1 |
| ecuador | 1 |
| Costa Rica | 0 |
| El Salvador | 0 |
| Honduras | 0 |
| Nicaragua | 0 |
Publications appeared from 2010 to date that list authors from Latin American countries. Search conducted in PubMed (https://pubmed.ncbi.nlm.nih.gov/ ) on April 26, 2021. Search terms: fatty liver, steatohepatitis, NASH and NAFLD in the article title and author affiliation.
The reasons for the low research activity in the Latin-American region is likely related to factors such as income disparities, clinically-oriented medical training and insufficient availability of research funding among others. Collaboration between researchers from Brazil, Chile, Mexico and Argentina have generated important papers in the field of NAFLD. However, more coordinated efforts are needed in order to address the peculiarities of NAFLD in the region, update epidemiological information and conduct careful evaluation of the cost effectiveness of implementing treatment programs and new drugs as well as the development and validation of economic models to evaluate NAFLD disease burden. Indeed, financial support to generate and maintain research initiatives is needed, plus efforts to increase awareness of the relevance of research funding among stakeholders in the region. Also, institutional strengthening through North-South and South-South collaboration and articulation of multicenter consortia [35] is relevant to conduct impactful research. Collaboration with high-income countries where NAFLD has been researched for a long time (e.g., the United States and parts of western Europe) through existing international networks [36–38] as well as a more extensive participation in large international clinical trials may also help in improving NAFLD research in Latin America. Building large biobanks from well characterized patient populations integrating clinical, genetic, biomarkers and OMICs information is also key to this end. Scientific societies such as the Latin American Association for the Study of the Liver and all those devoted to group physicians and health professionals caring for patients with poor metabolic health may have a pivotal role in improving the situation by joining both political and scientific efforts.
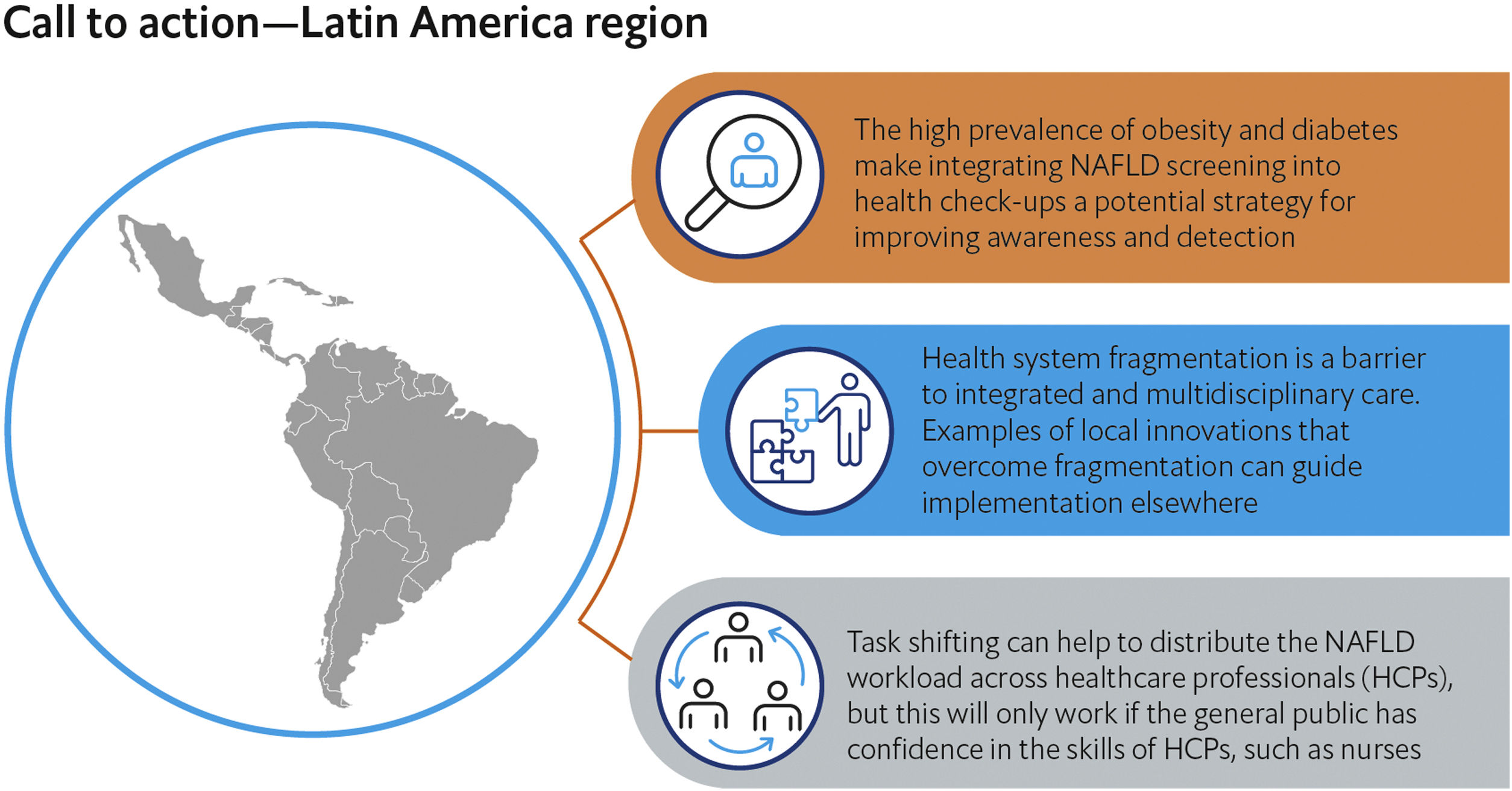
Public Health Policies: Addressing NAFLD with a whole of society approachNAFLD can affect all age groups, including children and adolescents. With rapidly rising (but currently underestimated) prevalence in Latin America, it is essential to have public policies to reduce and manage the burden of NAFLD and its health consequences [18,39]. The previously mentioned Economist Intelligence Unit workshop series convened worldwide experts–from liver disease and diabetes specialists to primary care providers and public health leaders–including those from Latin America. These panels helped to develop global and regional calls to action around awareness, risk stratification, integrated care, patient involvement and integration with other programs of non-communicable diseases, based on the responses of the expert panel members [18]. For Latin America, the report concluded that: 1) The high prevalence of obesity and diabetes makes integrating NAFLD screening into health check-ups a potential strategy for improving awareness and detection; 2) Health system fragmentation is a barrier to integrated and multidisciplinary care, but there are examples of innovations to overcome fragmentation that can guide implementation elsewhere; and 3) Task shifting can help to distribute the NAFLD workload across healthcare professionals (HCPs), but this will only work if the general public has confidence in the skills of HCPs, such as nurses [18]. These priorities provide a rallying point for stakeholders to align around as we seek to develop a roadmap for advancing the NAFLD public health agenda. (Fig. 1).
Call to action on NAFLD in the Latin America region.
Key actions to tackle NAFLD lack of awareness and management in the Latin America region were identified by a group of experts participating in a series of meetings organized by The Economist Intelligence Unit with the support of EASL International Liver Foundation (ELIF). Source: The Economist Intelligence Unit report “NAFLD: Sounding the alarm on a global public health challenge”. Available at: https://eiuperspectives.economist.com/healthcare/nafld-sounding-alarm-global-public-health-challenge.
Despite the clear imperative for multilevel action on NAFLD, the disease has received little attention in national and global health agendas. In Latin America, the key challenges are a lack of disease awareness, health system fragmentation and lack of effective strategies for the prevention and treatment of obesity and T2DM. There are however opportunities to put NAFLD on the radar of other specialties, particularly among those caring T2DM patients. Wide dissemination of current concepts on NAFLD and extensive collaboration between scientific societies, governments, NGOs, pharmaceutical industry and other stakeholders is urgently needed to advance the public health agenda for NAFLD and ensure we have the tools, knowledge and resources to address this public health challenge.
Authors contributionsJPA, MD, AG AND MA contributed to the conception and design of the article, JPA, LAD, MD, HEM, JVL, NMS, CPO, AG AND MA contributed to collection of relevant literature and data analysis contained in selected papers and wrote sections of the manuscript. JPA, LAD, MD, HM, JL, EV, NMS, CPO, AG AND contributed to drafting the article or revising it critically for important intellectual content, all authors approved the final version to be submitted.
Conflict of interestThe authors have no conflicts of interest to declare.
Funding sourcesThis article was partially supported by the Chilean government through the Fondo Nacional de Desarrollo Científico y Tecnológico (FONDECYT 1200227 to JPA and 1191145 to MA) and the Comisión Nacional de Investigación Científica y Tecnológica (CONICYT, AFB170005, CARE Chile UC). MA is part of the European- Latin American ESCALON consortium funded by the European Union’s Horizon 2020 Research and Innovation Program under grant agreement no. 825510.AbbreviationsNAFLD Non-alcoholic fatty liver disease Non-alcoholic steatohepatitis Metabolic (dysfunction)-associated fatty liver disease Latin American Association for the Study of the Liver Type 2 diabetes mellitus European Association for the Study of the Liver EASL International Liver Foundation non-governmental organizations
To Alan Lovell and Anelia Boshnakova from The Economist Intelligence Unit (The EIU) and to Jeffrey V Lazarus and Henry E Mark from the EASL International Liver Foundation for leading the discussion at a series of workshops on NAFLD in Latin America. The other Latin American experts who participating in the panel: Dr Paulo Archila, Dr Gabriela Castillo, Professor Nelia Hernández, Dr Natacha Jreige, Dr Mariana Lazo, Professor Patricio López-Jaramillo, Professor Sophia Martínez Vázquez, Dr Carla Musso, Dr Edna Nava, Dr Marlene Pérez Figueroa, Professor Mario Reis Alvares da Silva, Dr Josefina Selmo, Professor Marcelo Silva, Dr María José Suárez, and Dr Juan José Suarez Martinez.